What Is The Comparative Value Of The Us Healthcare System? This is a crucial question for anyone seeking to understand how the American healthcare model stacks up against those of other developed nations, and COMPARE.EDU.VN is here to provide you with the answers. By exploring the various aspects of healthcare delivery, spending, and outcomes, we can gain valuable insights into the strengths and weaknesses of the US system. Discover a comprehensive healthcare system comparison that helps you make informed decisions about healthcare policies, delivery, and access.
1. Introduction: The Enigma of US Healthcare
The United States healthcare system is often the subject of intense debate and scrutiny. Renowned for its innovation and technological advancements, it also faces criticism for its high costs and unequal access. Understanding the comparative value of the US healthcare system requires a detailed examination of its performance relative to other developed nations. This article aims to provide a comprehensive analysis, drawing on credible sources and statistical data to offer a balanced perspective.
The question remains: Is the US healthcare system truly the best, or are there lessons to be learned from other models? Let’s dive into the numbers and explore the facts.
2. Understanding the Basics of Healthcare Systems
Before delving into a comparison, it’s essential to understand the fundamental components of a healthcare system. These include:
- Funding Mechanisms: How healthcare is financed (e.g., taxes, insurance premiums, out-of-pocket payments).
- Delivery Models: How healthcare services are provided (e.g., public hospitals, private clinics, managed care organizations).
- Coverage and Access: Who is covered by health insurance and how easily people can access healthcare services.
- Regulation and Oversight: How healthcare providers and insurers are regulated and monitored.
Different countries employ various combinations of these elements, leading to diverse healthcare outcomes and experiences.
3. Healthcare Spending: The US Outlier
One of the most striking aspects of the US healthcare system is its high level of spending.
3.1. Per Capita Spending
The United States spends significantly more per person on healthcare than any other developed nation.
In 2022, health expenditures per person in the U.S. were $12,555, which was over $4,000 more than any other high-income nation. The average amount spent on health per person in comparable countries ($6,651) is about half of what the U.S. spends per person.
This high spending is driven by several factors, including:
- Higher prices for pharmaceuticals and medical services.
- Greater administrative costs.
- More intensive use of technology.
3.2. Health Spending as a Percentage of GDP
The US also allocates a larger share of its gross domestic product (GDP) to healthcare than other developed countries. In 2022, the U.S. spent 16.6% of its GDP on health-related expenditures. This is substantially higher than in peer countries.
The high level of spending raises questions about the value the US receives in return. Are the health outcomes in the US commensurate with the level of investment?
4. Comparing Health Outcomes
While the US spends more on healthcare, its health outcomes are not necessarily better than those of other developed nations.
4.1. Life Expectancy
Life expectancy in the US is lower than in many other high-income countries. According to the CDC, life expectancy in the U.S. is around 77.5 years. In comparison, countries like Japan and Switzerland have life expectancies exceeding 83 years.
4.2. Infant Mortality
The infant mortality rate in the US is also higher than in many peer nations. The CDC reported a rate of 5.4 deaths per 1,000 live births in 2021. This is higher than the rates in countries like Finland and Slovenia.
4.3. Maternal Mortality
Maternal mortality rates in the US have been rising in recent years, a trend that contrasts with the declines seen in many other developed countries. The CDC reported a maternal mortality rate of 32.9 deaths per 100,000 live births in 2021.
4.4. Chronic Diseases
The prevalence of chronic diseases, such as diabetes and heart disease, is also a concern in the US. While the US has made progress in treating these conditions, prevention efforts may lag behind those in other countries.
5. Access to Healthcare
Access to healthcare is another critical aspect of the comparative value of a healthcare system.
5.1. Health Insurance Coverage
The US is unique among developed nations in not having universal health insurance coverage. While the Affordable Care Act (ACA) has reduced the number of uninsured Americans, millions still lack coverage. According to the Kaiser Family Foundation, approximately 8.5% of the US population was uninsured in 2022.
5.2. Barriers to Access
Even for those with insurance, access to healthcare can be challenging due to:
- High deductibles and co-payments.
- Limited provider networks.
- Geographic barriers, particularly in rural areas.
These barriers can lead to delayed or forgone care, which can negatively impact health outcomes.
6. Strengths of the US Healthcare System
Despite its challenges, the US healthcare system also has several strengths.
6.1. Innovation and Technology
The US is a leader in medical innovation, developing cutting-edge treatments and technologies. US spending on research and development (R&D) is among the highest in the world, driving advancements in pharmaceuticals, medical devices, and diagnostic tools.
6.2. Specialist Care
The US has a highly specialized healthcare workforce, with experts in a wide range of medical fields. This allows for advanced and specialized care for complex medical conditions.
6.3. Choice and Flexibility
Many Americans value the choice and flexibility offered by the US healthcare system. Patients can often choose their doctors, hospitals, and insurance plans, providing a sense of control over their healthcare decisions.
7. Weaknesses of the US Healthcare System
The weaknesses of the US healthcare system are well-documented and contribute to its lower comparative value.
7.1. High Costs
As discussed earlier, the high cost of healthcare in the US is a major concern. These costs can create financial burdens for individuals, families, and businesses.
7.2. Lack of Universal Coverage
The lack of universal health insurance coverage leaves millions vulnerable to financial hardship and poor health outcomes. This also contributes to disparities in access to care based on income, race, and ethnicity.
7.3. Administrative Complexity
The US healthcare system is notoriously complex, with a multitude of payers, providers, and regulations. This complexity drives up administrative costs and can create confusion for patients and providers alike.
8. Comparative Analysis: US vs. Other Developed Nations
To better understand the comparative value of the US healthcare system, let’s compare it to those of other developed nations.
8.1. Canada
Canada has a universal healthcare system, funded primarily through taxes. Healthcare is publicly administered, and most services are free at the point of use. While Canada’s healthcare spending is lower than that of the US, wait times for certain procedures can be longer.
8.2. United Kingdom
The United Kingdom’s National Health Service (NHS) is a publicly funded healthcare system that provides comprehensive coverage to all residents. The NHS is funded through general taxation, and most services are free at the point of use. The UK’s healthcare spending is significantly lower than that of the US, but the NHS has faced challenges with funding and staffing in recent years.
8.3. Germany
Germany has a social health insurance system, where healthcare is funded through mandatory contributions from employers and employees. Health insurance is universal, and individuals can choose from a range of public and private health insurance plans. Germany’s healthcare spending is lower than that of the US, and its health outcomes are generally better.
8.4. Australia
Australia has a mixed public-private healthcare system, with universal coverage provided through Medicare, a publicly funded health insurance scheme. Australians can also purchase private health insurance to cover services not covered by Medicare. Australia’s healthcare spending is lower than that of the US, and its health outcomes are comparable to those of other developed nations.
9. Key Metrics in Comparative Healthcare Analysis
When comparing healthcare systems, several key metrics are commonly used:
9.1. Cost
- Healthcare spending per capita.
- Healthcare spending as a percentage of GDP.
9.2. Access
- Percentage of the population with health insurance coverage.
- Availability of primary care physicians and specialists.
- Wait times for appointments and procedures.
9.3. Quality
- Mortality rates for common conditions.
- Hospital readmission rates.
- Patient satisfaction scores.
9.4. Outcomes
- Life expectancy.
- Infant mortality rate.
- Maternal mortality rate.
10. Factors Influencing Healthcare Value
Several factors can influence the value of a healthcare system:
10.1. System Design
The structure of a healthcare system, including its funding mechanisms and delivery models, can significantly impact its value.
10.2. Policy Choices
Government policies, such as regulations on insurance and pharmaceuticals, can also influence healthcare costs and outcomes.
10.3. Socioeconomic Factors
Socioeconomic factors, such as poverty and education levels, can affect health outcomes and access to care.
10.4. Cultural Factors
Cultural factors, such as attitudes towards health and healthcare, can also play a role in shaping the value of a healthcare system.
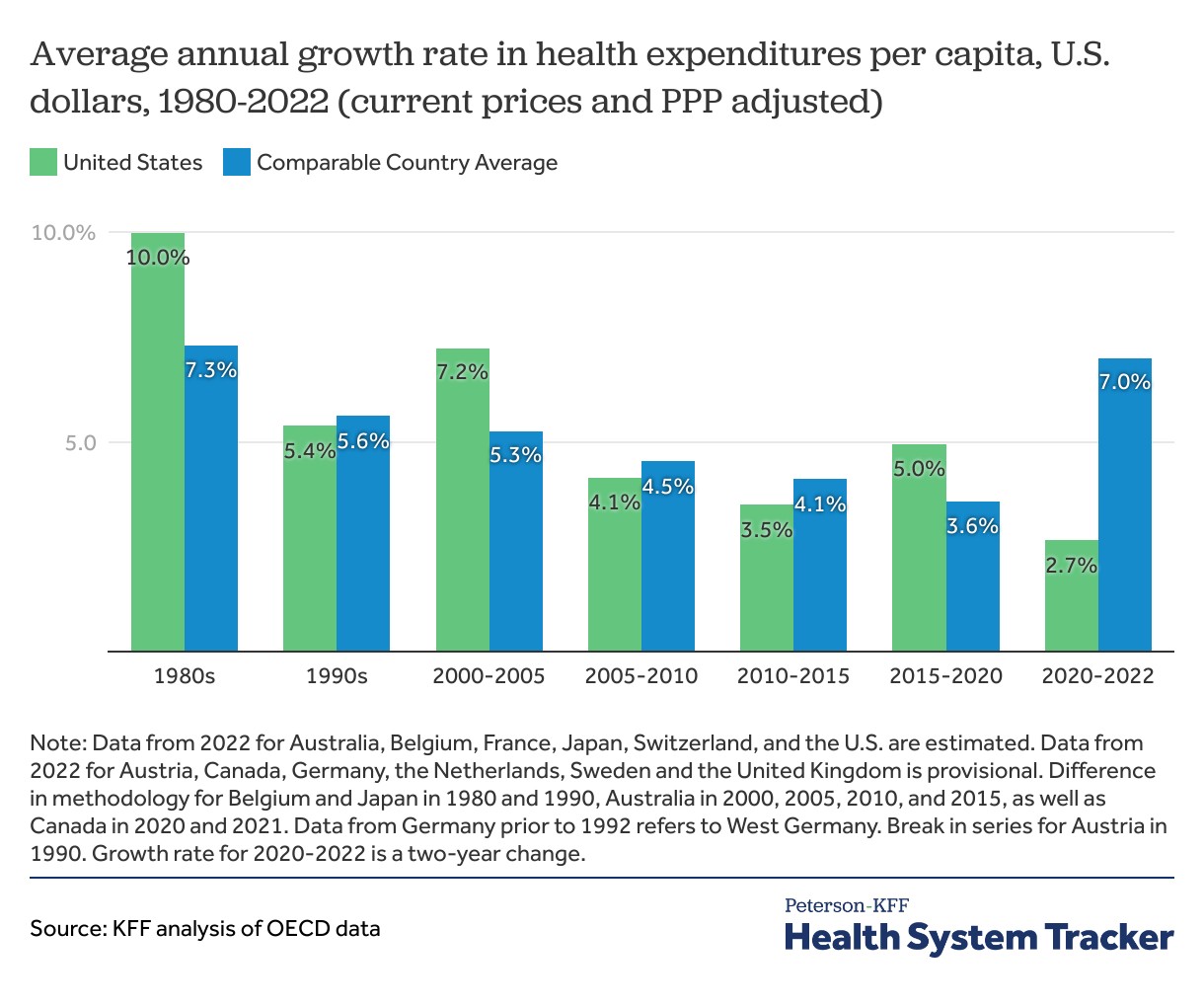
11. Understanding Health Spending Growth Rates
Health spending growth rates provide insights into how rapidly healthcare costs are increasing in different countries.
While the U.S. has long had higher than average health spending, recent years have seen higher spending growth in other nations. The annual growth rate for the average of comparable countries increased between 2020 and 2022 to 7.0% versus a 2.7% increase for the U.S. during the same period.
12. The Role of Technology in Healthcare
Technology plays an increasingly important role in healthcare, with the potential to improve efficiency, quality, and access.
12.1. Telemedicine
Telemedicine allows patients to receive medical care remotely, using technology such as video conferencing and mobile apps.
12.2. Electronic Health Records
Electronic health records (EHRs) can improve communication and coordination among healthcare providers, leading to better care.
12.3. Artificial Intelligence
Artificial intelligence (AI) has the potential to transform healthcare by improving diagnosis, treatment, and prevention.
13. Impact of Policy and Reform on US Healthcare
Policy and reform efforts have had a significant impact on the US healthcare system.
13.1. Affordable Care Act (ACA)
The ACA has expanded health insurance coverage to millions of Americans, but it has also faced criticism for its impact on premiums and deductibles.
13.2. Medicare and Medicaid
Medicare and Medicaid are government-funded health insurance programs that provide coverage to seniors, low-income individuals, and people with disabilities.
13.3. Value-Based Care
Value-based care models aim to improve healthcare quality and reduce costs by rewarding providers for achieving better outcomes.
14. Future Trends in Healthcare
Several trends are expected to shape the future of healthcare:
14.1. Aging Population
As the population ages, the demand for healthcare services will increase, placing greater strain on healthcare systems.
14.2. Rise of Chronic Diseases
The prevalence of chronic diseases is expected to continue to rise, requiring greater investment in prevention and management.
14.3. Personalized Medicine
Personalized medicine, which tailors treatment to individual characteristics, has the potential to improve outcomes and reduce costs.
15. Analyzing Healthcare System Performance
Analyzing the performance of healthcare systems involves assessing their strengths, weaknesses, opportunities, and threats (SWOT analysis).
15.1. Strengths
- Innovation and technology.
- Specialist care.
- Choice and flexibility.
15.2. Weaknesses
- High costs.
- Lack of universal coverage.
- Administrative complexity.
15.3. Opportunities
- Expanding access to care through telemedicine.
- Improving care coordination through EHRs.
- Reducing costs through value-based care models.
15.4. Threats
- Rising healthcare costs.
- Aging population.
- Political uncertainty.
16. Healthcare Disparities
Healthcare disparities are differences in access to or quality of healthcare based on race, ethnicity, socioeconomic status, or other factors.
16.1. Racial and Ethnic Disparities
Racial and ethnic minorities often face barriers to healthcare, leading to poorer health outcomes.
16.2. Socioeconomic Disparities
Low-income individuals and families may struggle to afford healthcare, leading to delayed or forgone care.
17. Impact of Social Determinants on Health
Social determinants of health are the conditions in which people are born, grow, live, work, and age. These factors can have a significant impact on health outcomes.
17.1. Income and Education
Income and education levels can affect access to healthy food, safe housing, and quality healthcare.
17.2. Access to Healthy Food
Lack of access to healthy food can contribute to chronic diseases such as diabetes and heart disease.
18. Strategies for Improving Healthcare Value
Several strategies can be used to improve the value of the US healthcare system:
18.1. Cost Containment Measures
Cost containment measures, such as negotiating lower drug prices and reducing administrative waste, can help lower healthcare costs.
18.2. Expanding Access to Care
Expanding access to care through universal health insurance coverage and telemedicine can improve health outcomes.
18.3. Improving Quality of Care
Improving quality of care through value-based care models and care coordination can lead to better outcomes and lower costs.
19. The Role of Public Health
Public health plays a critical role in preventing disease and promoting health.
19.1. Prevention Efforts
Prevention efforts, such as vaccinations and smoking cessation programs, can help reduce the burden of chronic diseases.
19.2. Health Education
Health education can empower individuals to make informed decisions about their health.
20. Consumerism in Healthcare
Consumerism in healthcare refers to the increasing role of consumers in making healthcare decisions.
20.1. Transparency
Transparency in healthcare pricing and quality can help consumers make informed choices.
20.2. Patient Engagement
Patient engagement, such as shared decision-making, can improve patient satisfaction and outcomes.
21. The Future of US Healthcare
The future of US healthcare is uncertain, but several factors are likely to shape its evolution.
21.1. Technological Advancements
Technological advancements, such as AI and personalized medicine, have the potential to transform healthcare.
21.2. Policy Changes
Policy changes, such as reforms to the ACA, could significantly impact the US healthcare system.
22. Conclusion: Evaluating the US Healthcare System
The US healthcare system is a complex and multifaceted entity. While it excels in innovation and specialist care, it lags behind other developed nations in terms of cost, access, and health outcomes. Improving the value of the US healthcare system will require a concerted effort to address its weaknesses and build on its strengths.
For more in-depth comparisons and detailed analyses, visit COMPARE.EDU.VN. We provide the resources you need to make informed decisions about healthcare policies, delivery, and access.
23. Call to Action
Ready to make a more informed decision about your healthcare choices? Visit COMPARE.EDU.VN today to explore detailed comparisons, access expert insights, and find the best options for your needs. Our comprehensive resources are designed to empower you with the knowledge you need to navigate the complexities of healthcare and make the right choices for you and your family.
Don’t navigate the complexities of healthcare alone. Trust COMPARE.EDU.VN to provide the comprehensive comparisons and expert insights you need to make informed decisions. Visit our website at compare.edu.vn or contact us at 333 Comparison Plaza, Choice City, CA 90210, United States. Whatsapp: +1 (626) 555-9090. Let us help you find the best healthcare solutions for your unique needs.
24. FAQs About the US Healthcare System
Here are some frequently asked questions about the US healthcare system:
24.1. Why is healthcare so expensive in the US?
Healthcare in the US is expensive due to higher prices for pharmaceuticals and medical services, greater administrative costs, and more intensive use of technology.
24.2. What is the Affordable Care Act (ACA)?
The ACA is a healthcare reform law enacted in 2010 that aimed to expand health insurance coverage and improve access to care.
24.3. What is Medicare?
Medicare is a government-funded health insurance program that provides coverage to seniors and people with disabilities.
24.4. What is Medicaid?
Medicaid is a government-funded health insurance program that provides coverage to low-income individuals and families.
24.5. How does the US healthcare system compare to those of other developed nations?
The US healthcare system spends more per person on healthcare than any other developed nation, but its health outcomes are not necessarily better.
24.6. What are some of the challenges facing the US healthcare system?
Some of the challenges facing the US healthcare system include high costs, lack of universal coverage, and administrative complexity.
24.7. What are some of the strengths of the US healthcare system?
Some of the strengths of the US healthcare system include innovation and technology, specialist care, and choice and flexibility.
24.8. How can the value of the US healthcare system be improved?
The value of the US healthcare system can be improved through cost containment measures, expanding access to care, and improving quality of care.
24.9. What is value-based care?
Value-based care is a healthcare delivery model that rewards providers for achieving better outcomes and reducing costs.
24.10. What is the role of public health in improving health outcomes?
Public health plays a critical role in preventing disease and promoting health through prevention efforts and health education.