Introduction
Human Papillomavirus (HPV) is a common sexually transmitted infection that can lead to several types of cancer, including cervical, vaginal, vulvar, penile, anal, and oropharyngeal cancers. Appalachia, a region in the eastern United States encompassing states like West Virginia, Kentucky, and Ohio, faces significant health disparities, including higher cancer rates. While cervical cancer disparities in Appalachia are well-documented, the broader burden of HPV-related cancers and the potential impact of HPV vaccination in this region require closer examination. This article analyzes HPV-related cancer incidence in West Virginia and Appalachian regions of Kentucky and Ohio, comparing them to national averages and non-Appalachian areas, to highlight the critical need for improved HPV vaccination rates in West Virginia and similar areas. Understanding these disparities is crucial for public health initiatives aimed at cancer prevention and reducing health inequities.
HPV-Related Cancer Incidence in Appalachian States: A Disparity
Research examining cancer registry data from 1996 to 2008 in Ohio, Kentucky, West Virginia, and the SEER 9 program (Surveillance, Epidemiology, and End Results) reveals significant disparities in HPV-related cancer incidence.
Higher Rates Among Females in Appalachia
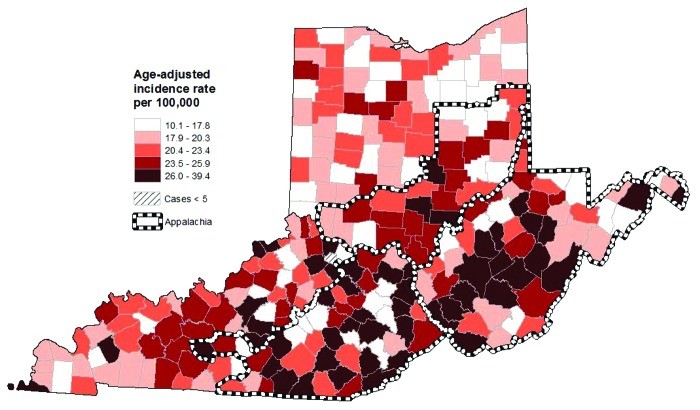
For females, the incidence rates of all HPV-related cancers combined were notably higher in Appalachian Kentucky [24.6 per 100,000 population (95% CI: 23.5–25.7)], West Virginia [22.8 (95% CI: 22.0–23.6)], and Appalachian Ohio [21.9 (95% CI: 21.0–22.8)] when compared to the SEER 9 average [18.8 (95% CI: 18.6–19.0)]. This indicates a greater burden of HPV-related cancers among women living in these Appalachian regions.
Figure 1: Geographic variations in HPV-related cancer incidence among females in Ohio, West Virginia, and Kentucky, highlighting higher rates in specific Appalachian counties.
Delving into specific cancer types, Appalachian Kentucky [cervical: 12.4 (95% CI: 11.6–13.2); vulvar: 3.6 (95% CI: 3.2–4.0)], Appalachian Ohio [cervical: 10.9 (95% CI: 10.2–11.6); vulvar: 2.9 (95% CI: 2.6–3.3)], and West Virginia [cervical: 11.1 (95% CI: 10.5–11.7); vulvar: 2.9 (95% CI: 2.6–3.2)] demonstrated elevated incidence rates for both cervical and vulvar cancers compared to SEER 9 [cervical: 7.7 (95% CI: 7.6–7.8); vulvar: 2.4 (95% CI: 2.3–2.4)]. West Virginia’s rates are particularly concerning as the entire state is considered Appalachian.
Disparities Among Males in Appalachian Ohio
Among males, Appalachian Ohio showed a higher incidence rate for all HPV-related cancers combined compared to non-Appalachian Ohio [17.6 (95% CI: 16.8–18.5) vs. 16.3 (95% CI: 16.0–16.6)]. While Kentucky showed higher rates than SEER 9, there wasn’t a significant difference between Appalachian and non-Appalachian Kentucky in overall HPV-related cancer incidence for males. However, Appalachian regions of both Kentucky and Ohio had higher penile cancer incidence rates compared to their non-Appalachian counterparts.
Figure 2: County-level map showing HPV-related cancer incidence in males across Ohio, West Virginia, and Kentucky, illustrating regional variations within Appalachia.
Factors Contributing to Higher Cancer Rates in Appalachia
Several factors may contribute to the higher HPV-related cancer incidence in Appalachia, and consequently underscore the importance of vaccination efforts in West Virginia and the broader region:
- Socioeconomic Factors: Appalachia is characterized by lower education levels, higher poverty rates, and poorer overall health compared to the rest of the US. These socioeconomic challenges can impact access to healthcare, preventive services like cancer screenings, and health literacy, all crucial for HPV prevention and early cancer detection.
- Risky Health Behaviors: Studies suggest that risky sexual behaviors, which increase HPV transmission risk, and tobacco use, which can hinder HPV clearance, may be more prevalent in Appalachia. Higher smoking rates in West Virginia, Kentucky, and Ohio compared to the national average further exacerbate the risk of HPV-related cancers.
- Limited Access to Screening: Cervical cancer screening rates are lower among women in Appalachia compared to non-Appalachian women. Reduced screening means precancerous lesions may go undetected and untreated, progressing to invasive cancer.
The Critical Role of HPV Vaccination in West Virginia and Appalachia
The disparities in HPV-related cancer incidence in West Virginia and Appalachia highlight the urgent need for effective prevention strategies, with HPV vaccination standing out as a powerful tool.
HPV Vaccine: A Proven Cancer Prevention Tool
HPV vaccines are safe and highly effective in preventing infection from the HPV types that cause the majority of HPV-related cancers. Vaccination can significantly reduce the incidence of cervical, vulvar, vaginal, anal, penile, and oropharyngeal cancers.
Vaccination Rates: Room for Improvement in Appalachia
Despite the availability and recommendation of HPV vaccines, vaccination rates, particularly in regions like Appalachia, lag behind national goals. While specific HPV vaccination rates for West Virginia compared to other states weren’t directly assessed in the original study, data indicates that states with Appalachian regions often have lower HPV vaccine uptake. This is likely influenced by factors similar to those contributing to higher cancer rates: socioeconomic barriers, access to healthcare, and potentially vaccine hesitancy in certain communities.
Recent national data reveals that while HPV vaccine initiation among adolescent females in the US is around 50%, completion rates (receiving all recommended doses) are significantly lower. Moreover, vaccine uptake among adolescent males is even lower. Within the 13 states containing Appalachian counties, a majority show lower statewide HPV vaccine initiation and completion rates among females compared to national averages. This suggests that West Virginia and other Appalachian states likely face challenges in achieving optimal HPV vaccination coverage.
Public Health Implications and Call to Action
The findings underscore that West Virginia and Appalachia stand to benefit immensely from increased HPV vaccination efforts. Widespread vaccination has the potential to dramatically reduce HPV-related cancer incidence and mitigate the existing cancer disparities in this region. Public health initiatives should focus on:
- Improving Access to Vaccination: Addressing socioeconomic barriers and healthcare access limitations in Appalachia is crucial to ensure all adolescents and young adults have the opportunity to receive the HPV vaccine.
- Education and Awareness Campaigns: Targeted campaigns are needed to educate communities in West Virginia and Appalachia about HPV, HPV-related cancers, and the safety and effectiveness of HPV vaccines. Addressing vaccine hesitancy through culturally sensitive and community-engaged approaches is essential.
- Healthcare Provider Recommendations: Healthcare providers in Appalachia play a vital role in recommending and administering HPV vaccines. Efforts to improve provider education and promote strong vaccine recommendations are key to increasing uptake.
Conclusion
This analysis of HPV-related cancer incidence data confirms the existence of significant disparities in West Virginia and Appalachia compared to national averages and non-Appalachian regions. These disparities, particularly among women, highlight the urgent need to prioritize cancer prevention efforts in this region. HPV vaccination is a powerful and proven tool to reduce the burden of these cancers and address health inequities. Improving HPV vaccination rates in West Virginia and across Appalachia through targeted public health interventions is essential to achieving cancer prevention goals and promoting health equity in this vulnerable population. Further research is needed to specifically assess HPV vaccination rates within West Virginia and Appalachia to guide and monitor the effectiveness of intervention strategies.
Materials and Methods
This analysis is based on data from the Kentucky, West Virginia, and Ohio Cancer Registries, and the SEER 9 cancer registries for the years 1996-2008. Cancer incidence rates were calculated and age-adjusted to the 2000 U.S. standard population. HPV-related cancers included cervical, vaginal, vulvar, penile, anal, and oral cavity/pharyngeal cancers, categorized according to ICDO-3 and SEER Program site recode classifications. Appalachian counties were defined using the Appalachian Regional Commission’s classification scheme. Statistical significance was determined using non-overlapping 95% confidence intervals. County-level incidence rates were mapped using ArcGIS to visualize geographic patterns within Appalachia.
Acknowledgments
Data for this analysis were provided by the Kentucky and West Virginia Cancer Registries and the Ohio Cancer Incidence Surveillance System. This work was supported by grants from the National Cancer Institute and the Centers for Disease Control and Prevention.
Glossary
- HPV: Human papillomavirus
- STI: Sexually transmitted infection
- SEER: Surveillance, Epidemiology and End Results
- CI: Confidence interval
- KCR: Kentucky Cancer Registry
- OCISS: Ohio Cancer Incidence Surveillance System
- WVCR: West Virginia Cancer Registry
- ICDO-3: International Classification of Diseases for Oncology, third edition
- IR: Incidence rate
Disclosure of Potential Conflicts of Interest
P.L.R. and E.D.P. have received research grants from Merck Sharp and Dohme Corp., but this funding was not used for this specific study.
Footnotes
Previously published online: www.landesbioscience.com/journals/vaccines/article/22389