How Many People Died In 2020 Compared To 2019 is a critical question, and COMPARE.EDU.VN delves into the detailed mortality statistics, offering a comprehensive analysis of the factors contributing to the increase in deaths. Our analysis provides a clear understanding of death rate trends, life expectancy shifts, and the leading causes of mortality. Explore detailed comparisons and insightful data on mortality rates and life expectancy with us.
1. Understanding Mortality Trends: A 2019 vs. 2020 Comparison
1.1. Overall Mortality Increase in 2020
In 2020, the United States experienced a significant increase in mortality. A total of 3,383,729 resident deaths were registered, marking an increase of 528,891 deaths compared to 2019. This surge in mortality is a crucial indicator of the impact of various factors, including the COVID-19 pandemic, on public health. The rise in the number of deaths highlights the need for detailed comparative analysis to understand the underlying causes and their effects on different demographic groups. This data underscores the importance of continuous monitoring and evaluation of mortality trends to inform public health strategies and interventions.
1.2. Age-Adjusted Death Rates: A Comprehensive Overview
The age-adjusted death rate, which accounts for differences in age distribution across populations, saw a significant increase of 16.8% from 715.2 per 100,000 standard population in 2019 to 835.4 in 2020. This metric is crucial for accurately comparing mortality trends over time and across different groups. The substantial increase reflects the broad impact of factors such as the COVID-19 pandemic, healthcare access, and socioeconomic disparities on mortality rates. Understanding these age-adjusted rates provides valuable insights into the changing patterns of mortality and helps identify areas where public health interventions are most needed.
1.3. Impact of COVID-19 on Mortality Statistics
COVID-19 was officially recognized as a cause of death in 2020, contributing significantly to the increase in mortality. The number of deaths attributed to COVID-19 as the underlying cause was 350,831, accounting for 10.4% of all deaths in 2020. This new cause of death ranked as the third leading cause of mortality, underscoring the profound impact of the pandemic on public health. The emergence of COVID-19 as a major cause of death necessitated a reevaluation of mortality patterns and healthcare priorities. Tracking the specific effects of COVID-19 on mortality rates has been essential for implementing effective prevention and treatment strategies.
2. Examining Life Expectancy Changes in 2020
2.1. Decline in Overall Life Expectancy
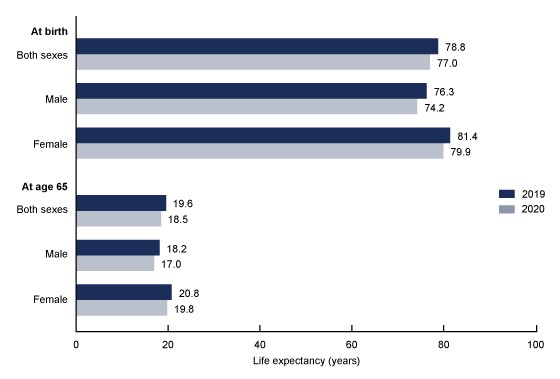
In 2020, life expectancy at birth for the total U.S. population was 77.0 years, representing a decrease of 1.8 years from 78.8 years in 2019. This decline marks the largest single-year decrease in life expectancy in more than 75 years, highlighting the severe impact of the pandemic and other factors on population health. The reduction in life expectancy underscores the urgent need for comprehensive public health interventions to address the underlying causes and mitigate the long-term effects on population health outcomes.
2.2. Gender Disparities in Life Expectancy
Significant gender disparities were observed in the decline of life expectancy. For males, life expectancy decreased by 2.1 years, from 76.3 years in 2019 to 74.2 years in 2020. Females experienced a decrease of 1.5 years, from 81.4 years in 2019 to 79.9 years in 2020. The difference in life expectancy between females and males increased by 0.6 years, from 5.1 years in 2019 to 5.7 years in 2020. These disparities highlight the different health challenges faced by men and women and the need for gender-specific interventions to improve overall life expectancy.
2.3. Impact on Life Expectancy at Age 65
Life expectancy at age 65 also saw a decline in 2020. For the total population, life expectancy at age 65 was 18.5 years, a decrease of 1.1 years from 2019. Males experienced a decrease of 1.2 years, from 18.2 years in 2019 to 17.0 years in 2020, while females saw a decrease of 1.0 year, from 20.8 years in 2019 to 19.8 years in 2020. These figures indicate that the older population was significantly affected by the factors contributing to increased mortality, emphasizing the importance of targeted healthcare and support services for seniors.
3. Race and Ethnicity: Disparities in Mortality Rates
3.1. Increased Death Rates Across All Groups
In 2020, age-adjusted death rates increased across all race and ethnicity groups compared to 2019. This widespread increase underscores the pervasive impact of factors such as the COVID-19 pandemic and systemic health inequities on mortality rates across different populations. Understanding these trends is crucial for developing targeted interventions to address specific health challenges and reduce disparities.
3.2. Highest Increase Among Hispanic Populations
Hispanic males experienced the most significant increase in age-adjusted death rates, with a rise of 42.7%. Hispanic females also saw a substantial increase of 32.4%. These figures highlight the disproportionate impact of health crises on the Hispanic community, necessitating culturally competent and linguistically appropriate healthcare services. Addressing socioeconomic factors, such as access to healthcare, employment, and housing, is essential for reducing these disparities and improving health outcomes for Hispanic populations.
3.3. Substantial Increases Among Black Populations
Non-Hispanic Black males saw an increase of 28.0% in age-adjusted death rates, while non-Hispanic Black females experienced a rise of 24.9%. These increases reflect the persistent health inequities faced by the Black community, including disparities in healthcare access, quality of care, and exposure to environmental hazards. Addressing these systemic issues is crucial for achieving health equity and reducing mortality rates among Black populations.
3.4. Increases Among White Populations
Non-Hispanic White males experienced an increase of 13.4% in age-adjusted death rates, and non-Hispanic White females saw a rise of 12.1%. While the increases were smaller compared to other groups, they still indicate a significant impact on the White population, underscoring the broad reach of factors such as the COVID-19 pandemic and other health challenges. Understanding these trends is important for developing comprehensive public health strategies that address the needs of all segments of the population.
4. Age-Specific Mortality Rates: Changes Across Age Groups
4.1. Increases in Mortality for Older Age Groups
From 2019 to 2020, death rates increased for each age group 15 years and over. The increases were particularly pronounced in older age groups, reflecting the greater vulnerability of these populations to health crises and underlying health conditions. These trends underscore the importance of targeted interventions to protect and support older adults.
4.2. Significant Increases for Young Adults
Age groups 15–24 and 25–34 experienced substantial increases in death rates. The rate for the 15–24 age group increased by 20.8%, from 69.7 deaths per 100,000 population in 2019 to 84.2 in 2020. The rate for the 25–34 age group increased by 23.8%, from 128.8 to 159.5. These increases highlight the need for targeted public health interventions to address factors such as mental health, substance abuse, and accidental injuries among young adults.
4.3. Moderate Increases for Middle-Aged Adults
The 35–44 age group saw an increase of 24.5% in death rates, from 199.2 to 248.0, while the 45–54 age group experienced an increase of 20.7%, from 392.4 to 473.5. These figures indicate that middle-aged adults were also significantly affected by the factors contributing to increased mortality, emphasizing the importance of preventive healthcare and early detection of health conditions.
4.4. Highest Rates Among Older Adults
The 65–74 age group saw an increase of 17.4% in death rates, from 1,764.6 to 2,072.3, while the 75–84 age group experienced an increase of 16.0%, from 4,308.3 to 4,997.0. The 85 and over age group saw an increase of 15.0%, from 13,228.6 to 15,210.9. These rates highlight the continued vulnerability of older adults and the need for comprehensive healthcare and support services to improve their health outcomes.
5. Leading Causes of Death: Shifting Patterns
5.1. Top Causes of Mortality in 2020
In 2020, the leading cause of death was heart disease, followed by cancer. COVID-19 emerged as the third leading cause, highlighting its significant impact on mortality. The remaining leading causes included unintentional injuries, stroke, chronic lower respiratory diseases, Alzheimer’s disease, diabetes, influenza and pneumonia, and kidney disease. Understanding these leading causes is crucial for prioritizing public health interventions and allocating resources effectively.
5.2. Changes in Rankings Compared to 2019
Several leading causes of death changed ranks from 2019 to 2020. Unintentional injuries, which were the third leading cause in 2019, became the fourth leading cause in 2020. Chronic lower respiratory diseases moved from the fourth to the sixth position, while Alzheimer’s disease shifted from the sixth to the seventh. Diabetes moved from the seventh to the eighth position, and kidney disease moved from the eighth to the tenth. These shifts reflect the changing patterns of mortality and the impact of factors such as the COVID-19 pandemic on different causes of death.
5.3. Notable Increases in Death Rates for Specific Causes
Age-adjusted death rates increased for several leading causes of death from 2019 to 2020. Heart disease saw an increase of 4.1%, from 161.5 to 168.2, while unintentional injuries increased by 16.8%, from 49.3 to 57.6. Stroke increased by 4.9%, from 37.0 to 38.8, and Alzheimer’s disease increased by 8.7%, from 29.8 to 32.4. Diabetes increased by 14.8%, from 21.6 to 24.8, and influenza and pneumonia increased by 5.7%, from 12.3 to 13.0. These increases highlight the need for targeted interventions to address these specific causes of death and improve public health outcomes.
5.4. Decreases in Death Rates for Specific Causes
Age-adjusted death rates decreased for some leading causes of death from 2019 to 2020. Cancer saw a decrease of 1.4%, from 146.2 to 144.1, while chronic lower respiratory diseases decreased by 4.7%, from 38.2 to 36.4. These decreases may reflect improvements in prevention and treatment efforts for these conditions, although further research is needed to fully understand the underlying factors.
6. Infant Mortality: Trends and Causes
6.1. Overall Decline in Infant Mortality Rate (IMR)
The infant mortality rate (IMR), which measures the number of infant deaths per 100,000 live births, declined by 2.9% from 558.3 in 2019 to 541.9 in 2020. This decline indicates improvements in infant health outcomes, although further efforts are needed to address persistent disparities and reduce infant mortality rates further.
6.2. Leading Causes of Infant Death
In 2020, the leading causes of infant death included congenital malformations, low birth weight, sudden infant death syndrome (SIDS), unintentional injuries, maternal complications, cord and placental complications, bacterial sepsis of newborn, respiratory distress of newborn, diseases of the circulatory system, and neonatal hemorrhage. These ten leading causes accounted for 67.5% of all infant deaths in the United States.
6.3. Changes in Rankings Compared to 2019
Some leading causes of infant death exchanged ranks from 2019 to 2020. Sudden infant death syndrome moved from the fourth to the third position, while unintentional injuries moved from the third to the fourth position. Necrotizing enterocolitis of newborn, which was the tenth leading cause in 2019, dropped from the list and was replaced by neonatal hemorrhage in 2020.
6.4. Increases and Decreases in Mortality Rates for Specific Causes
The IMR for sudden infant death syndrome increased by 15.3%, from 33.3 in 2019 to 38.4 in 2020. The IMR for low birth weight decreased by 5.4%, from 91.9 in 2019 to 86.9 in 2020. Mortality rates for other leading causes of infant death did not change significantly.
7. The Role of COMPARE.EDU.VN in Data-Driven Decisions
7.1. Comprehensive Comparative Analysis
COMPARE.EDU.VN is dedicated to providing comprehensive comparative analyses to help individuals and organizations make informed decisions. Our platform offers detailed comparisons of various datasets, including mortality statistics, to identify trends, disparities, and key factors influencing public health outcomes. By offering a side-by-side comparison, we empower our users to understand complex issues and take appropriate action.
7.2. Data-Driven Insights for Public Health
Our analyses provide data-driven insights that are essential for public health professionals, policymakers, and researchers. By examining trends in mortality rates, causes of death, and demographic disparities, we help identify areas where interventions are most needed. Our platform supports evidence-based decision-making and promotes the development of effective strategies to improve public health outcomes.
7.3. Empowering Informed Decisions
COMPARE.EDU.VN empowers individuals to make informed decisions about their health and well-being. By providing clear, accessible, and reliable data, we help people understand the factors that affect their health outcomes and take proactive steps to improve their lives. Our platform promotes health literacy and encourages individuals to engage in preventive healthcare practices.
8. Factors Contributing to Mortality Changes
8.1. Public Health Emergencies
Public health emergencies, such as the COVID-19 pandemic, can significantly impact mortality rates. The emergence of new infectious diseases can strain healthcare systems, disrupt preventive care services, and lead to increased mortality. Effective preparedness, rapid response, and robust healthcare infrastructure are essential for mitigating the impact of public health emergencies on mortality rates.
8.2. Healthcare Access and Quality
Access to quality healthcare services is a critical determinant of mortality rates. Disparities in healthcare access, affordability, and quality can lead to poorer health outcomes and increased mortality, particularly among vulnerable populations. Addressing these disparities requires policies and programs that promote equitable access to healthcare services, improve healthcare quality, and reduce barriers to care.
8.3. Socioeconomic Factors
Socioeconomic factors, such as poverty, education, employment, and housing, can significantly influence mortality rates. Individuals living in poverty or facing socioeconomic disadvantages may have limited access to healthcare, nutritious food, safe housing, and other essential resources, leading to poorer health outcomes and increased mortality. Addressing these underlying social determinants of health is essential for reducing health disparities and improving overall population health.
8.4. Lifestyle and Behavioral Factors
Lifestyle and behavioral factors, such as diet, physical activity, tobacco use, and alcohol consumption, can contribute to mortality rates. Unhealthy behaviors can increase the risk of chronic diseases, such as heart disease, cancer, and diabetes, which are leading causes of death. Promoting healthy lifestyles through education, prevention programs, and policy interventions is crucial for reducing mortality rates and improving overall health outcomes.
9. Strategies for Reducing Mortality Rates
9.1. Strengthening Public Health Infrastructure
Investing in public health infrastructure is essential for preventing and controlling diseases, promoting health equity, and improving overall population health. Strong public health systems can effectively respond to public health emergencies, implement evidence-based prevention programs, and address the social determinants of health.
9.2. Improving Healthcare Access and Quality
Ensuring equitable access to quality healthcare services is crucial for reducing mortality rates and improving health outcomes. This requires policies and programs that expand health insurance coverage, increase access to primary care, improve healthcare quality, and reduce healthcare disparities.
9.3. Addressing Social Determinants of Health
Addressing the underlying social determinants of health is essential for reducing health disparities and improving overall population health. This requires comprehensive strategies that address poverty, education, employment, housing, and other socioeconomic factors that impact health outcomes.
9.4. Promoting Healthy Lifestyles
Promoting healthy lifestyles through education, prevention programs, and policy interventions is crucial for reducing mortality rates and improving overall health outcomes. This includes encouraging healthy diets, promoting physical activity, reducing tobacco use and alcohol consumption, and preventing substance abuse.
10. Future Directions in Mortality Research
10.1. Longitudinal Studies
Longitudinal studies that follow individuals over time are essential for understanding the long-term effects of various factors on mortality rates. These studies can provide valuable insights into the complex relationships between socioeconomic factors, lifestyle behaviors, healthcare access, and health outcomes.
10.2. Data Integration and Analytics
Integrating data from multiple sources, such as electronic health records, vital statistics, and socioeconomic data, can provide a more comprehensive understanding of mortality trends. Advanced data analytics techniques, such as machine learning and artificial intelligence, can help identify patterns and predict future mortality rates.
10.3. Community-Based Participatory Research
Community-based participatory research (CBPR) involves engaging community members in the research process to ensure that research questions, methods, and interventions are culturally appropriate and address community needs. CBPR can help identify and address the social determinants of health that contribute to mortality disparities.
10.4. Policy and Program Evaluation
Rigorous evaluation of policies and programs aimed at reducing mortality rates is essential for determining their effectiveness and identifying areas for improvement. Evaluation studies can provide valuable information on the impact of interventions on health outcomes, healthcare costs, and health equity.
In conclusion, the increase in mortality in 2020 compared to 2019 underscores the profound impact of the COVID-19 pandemic and other factors on public health. Addressing these challenges requires comprehensive strategies that strengthen public health infrastructure, improve healthcare access and quality, address the social determinants of health, and promote healthy lifestyles. By investing in research, data integration, and community engagement, we can gain a deeper understanding of mortality trends and develop effective interventions to improve population health outcomes.
Ready to compare more data and make informed decisions? Visit COMPARE.EDU.VN today!
For further information or inquiries, please contact us:
Address: 333 Comparison Plaza, Choice City, CA 90210, United States
Whatsapp: +1 (626) 555-9090
Website: COMPARE.EDU.VN
This information is intended to provide a detailed comparison and should not be considered medical advice. Always consult with a healthcare professional for personalized recommendations.
FAQ: Mortality Rates and Life Expectancy in 2020 vs. 2019
1. What was the main reason for the increase in deaths in 2020 compared to 2019?
The primary driver behind the increase in deaths in 2020 was the COVID-19 pandemic, which became the third leading cause of death.
2. How much did life expectancy decrease in 2020 compared to 2019?
Life expectancy at birth for the total U.S. population decreased by 1.8 years in 2020 compared to 2019.
3. Which racial or ethnic group experienced the largest increase in death rates in 2020?
Hispanic males experienced the largest increase in age-adjusted death rates in 2020, with a rise of 42.7%.
4. What were the top three leading causes of death in 2020?
The top three leading causes of death in 2020 were heart disease, cancer, and COVID-19.
5. Did infant mortality rates increase or decrease in 2020 compared to 2019?
Infant mortality rates decreased by 2.9% in 2020 compared to 2019.
6. How did age-adjusted death rates change for cancer and heart disease between 2019 and 2020?
Age-adjusted death rates decreased slightly for cancer and increased for heart disease between 2019 and 2020.
7. What age groups saw the most significant increases in death rates in 2020?
Age groups 15-24 and 25-34 experienced substantial increases in death rates in 2020.
8. What role did unintentional injuries play in the increased mortality rates in 2020?
Unintentional injuries were a significant factor, with age-adjusted death rates increasing by 16.8% between 2019 and 2020.
9. Where can I find more detailed data on mortality rates for different causes of death?
More detailed data can be found on the websites of organizations like the CDC and the National Center for Health Statistics (NCHS), as well as on compare.edu.vn.
10. How can communities work to reduce mortality rates in the future?
Communities can focus on strengthening public health infrastructure, improving healthcare access and quality, addressing the social determinants of health, and promoting healthy lifestyles.