The US healthcare system often faces criticism for its high costs and unequal access compared to other developed nations. One key difference lies in the financial burden on patients. In 2020, 26.8% of Americans reported skipping medical consultations due to cost, a stark contrast to the 7% average in comparable countries like Australia, Austria, Belgium, Canada, France, Germany, Japan, the Netherlands, Sweden, Switzerland, and the United Kingdom. Avoiding necessary medical care due to financial constraints can lead to poorer health outcomes and ultimately more expensive treatments down the line.
Key Differences in Healthcare Access and Outcomes
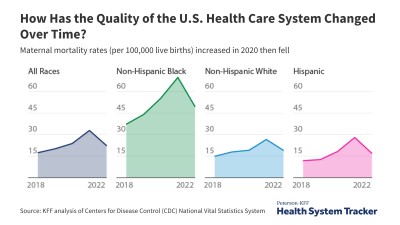
The COVID-19 pandemic further highlighted disparities in healthcare utilization. In 2020, as resources shifted towards COVID-19 care, routine appointments and procedures were often delayed or canceled, leading to a decrease in overall healthcare utilization. This disruption likely exacerbated existing access issues for many Americans.
Beyond cost-related barriers, international comparisons reveal significant differences in health outcomes. While comprehensive data is not always available for every country in every year, analyses of mortality rates, hospital admission rates for chronic conditions, and other key indicators consistently show areas where the US lags behind its peers. For example, certain measures like age-adjusted mortality rates for specific conditions are unavailable for some countries in particular years, making direct comparisons challenging. However, available data consistently points towards room for improvement in the US system.
Data Collection and Analysis: A Look at the OECD
The Organization for Economic Co-operation and Development (OECD) serves as a primary source for these international comparisons. The OECD gathers data on health quality and statistics from its member nations, allowing researchers to analyze trends and identify areas of strength and weakness in different healthcare systems. However, variations in data collection methods and population demographics across countries necessitate careful interpretation of these comparisons.
Despite these data limitations, analyzing metrics like 30-day mortality rates after acute myocardial infarction or stroke, hospital admission rates for chronic conditions like COPD and congestive heart failure, and C-section rates offers valuable insights into the relative performance of the US healthcare system. For example, C-section data is incomplete for certain countries in specific years, requiring interpolation or relying on inpatient rates in the absence of comprehensive data. Similarly, countries lacking 2021 data are excluded from certain comparative analyses.
Conclusion: The Need for Continued Improvement
While the US healthcare system boasts advanced medical technology and specialized care, its performance on measures of access, affordability, and outcomes often falls short of other high-income countries. Understanding these international comparisons is crucial for identifying areas where the US can learn from other systems and improve its own approach to healthcare delivery. The ongoing challenge lies in ensuring that all Americans have access to quality, affordable care, leading to improved health outcomes for the entire population.