How Does American Healthcare Compare To Other Countries? The American healthcare system is often a topic of intense debate, particularly when contrasted with the systems of other developed nations. COMPARE.EDU.VN offers a detailed exploration of the American healthcare landscape, comparing key metrics and outcomes with those of comparable countries, offering insights into healthcare quality and accessibility. Understand the strengths and weaknesses of the US healthcare system, and explore international healthcare system comparisons to make informed decisions.
1. Introduction to American Healthcare: A Comparative Overview
The United States healthcare system is unique among wealthy, developed nations. It is characterized by a mix of private and public insurance, with a significant portion of the population receiving coverage through their employers. However, this system also faces challenges such as high costs, uneven access to care, and variable quality outcomes. This comparative analysis aims to provide a comprehensive overview of how the U.S. healthcare system measures up against those of other developed countries, considering factors like access, cost, quality, and efficiency. Understanding these differences is crucial for informed discussions about healthcare reform and policy improvements in the U.S.
1.1 The U.S. Healthcare System: A Brief Overview
The U.S. healthcare system is a complex web of private and public insurance, employer-sponsored plans, and direct payments. Unlike many other developed nations with universal healthcare systems, the U.S. relies heavily on private insurance companies. This structure leads to a diverse range of coverage options, but it also contributes to significant disparities in access and affordability. Medicare, a federal program, provides health insurance for individuals aged 65 and older, as well as some younger people with disabilities. Medicaid, another federal program, provides coverage for low-income individuals and families. Despite these programs, a significant portion of the population remains uninsured or underinsured, leading to concerns about access to necessary medical care. The fragmented nature of the U.S. system can result in administrative inefficiencies and higher costs compared to more centralized systems.
1.2 Why Compare U.S. Healthcare to Other Countries?
Comparing the U.S. healthcare system to those of other developed countries offers valuable insights into its strengths and weaknesses. By examining key metrics such as healthcare spending, access to care, quality of services, and health outcomes, we can identify areas where the U.S. excels and areas where it lags behind. This comparative approach allows policymakers, healthcare professionals, and the public to understand how different healthcare models impact population health and economic efficiency. It also provides a basis for identifying best practices and potential reforms that could improve the U.S. system. Moreover, understanding the nuances of different healthcare systems can inform individual decisions about healthcare choices and advocacy efforts for better healthcare policies.
2. Key Metrics for Comparing Healthcare Systems
To effectively compare healthcare systems, it is essential to focus on key metrics that reflect the performance of each system. These metrics typically include healthcare spending, access to care, quality of care, efficiency, and health outcomes. Each metric provides a different lens through which to evaluate the strengths and weaknesses of a healthcare system. By analyzing these metrics across different countries, we can gain a more comprehensive understanding of how the U.S. healthcare system compares to its international counterparts.
2.1 Healthcare Spending: A Major Point of Divergence
Healthcare spending is one of the most significant points of divergence between the U.S. and other developed countries. The U.S. consistently spends more on healthcare per capita than any other nation in the OECD. Despite this higher spending, the U.S. does not consistently achieve better health outcomes compared to countries that spend less. This discrepancy raises questions about the efficiency and value of healthcare spending in the U.S. Factors contributing to higher spending include higher prices for prescription drugs, greater administrative costs, and a fee-for-service payment model that incentivizes volume over value. Examining healthcare spending in the U.S. requires a deeper look into the specific drivers of these costs and whether they translate into improved health outcomes for the population.
2.2 Access to Care: Insurance Coverage and Affordability
Access to care is a critical metric for evaluating the performance of a healthcare system. In the U.S., access to care is often linked to insurance coverage and affordability. While the Affordable Care Act (ACA) has expanded insurance coverage, a significant portion of the population remains uninsured or underinsured. This lack of coverage can lead to delayed or forgone medical care, resulting in poorer health outcomes. The high cost of healthcare, including premiums, deductibles, and co-pays, also poses a barrier to access for many Americans. Compared to countries with universal healthcare systems, the U.S. struggles with ensuring that all residents have access to necessary medical services regardless of their income or employment status. Addressing these challenges is crucial for improving health equity and overall population health.
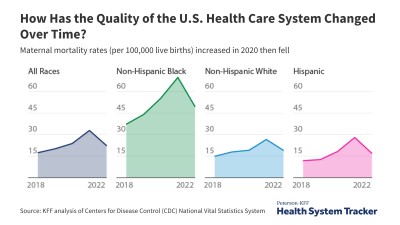
2.3 Quality of Care: Outcomes and Patient Safety
Quality of care encompasses a range of factors, including treatment effectiveness, patient safety, and patient satisfaction. While the U.S. excels in some areas, such as cancer survival rates, it lags behind other developed countries in other key areas, such as infant mortality and maternal mortality. Preventable medical errors and hospital-acquired infections are also significant concerns in the U.S. healthcare system. Measuring quality of care involves analyzing a variety of outcomes, including mortality rates for specific conditions, rates of preventable hospital readmissions, and patient experiences. Improving the quality of care requires a focus on evidence-based practices, patient-centered care, and continuous quality improvement initiatives.
2.4 Efficiency: Administrative Costs and Wait Times
Efficiency in healthcare refers to how well resources are used to deliver services. The U.S. healthcare system is often criticized for its administrative inefficiencies, which contribute to higher costs without necessarily improving patient care. Administrative costs in the U.S. are significantly higher than in other developed countries, due to factors such as the complexity of insurance billing and the lack of standardized processes. Wait times for certain medical services, such as specialist appointments and elective procedures, can also be a challenge in the U.S., although this varies by region and specialty. Improving efficiency requires streamlining administrative processes, adopting value-based payment models, and investing in technology to improve coordination of care.
2.5 Health Outcomes: Life Expectancy and Mortality Rates
Health outcomes are the ultimate measure of a healthcare system’s effectiveness. The U.S. has a lower life expectancy and higher mortality rates for certain conditions compared to many other developed countries. Factors contributing to these outcomes include higher rates of chronic diseases, such as obesity and diabetes, as well as disparities in access to care and social determinants of health. Infant mortality rates in the U.S. are also higher than in many other developed countries, reflecting challenges in prenatal care and maternal health. Improving health outcomes requires a comprehensive approach that addresses both healthcare and social factors, such as poverty, education, and access to healthy food.
3. Comparing U.S. Healthcare with Other Developed Countries
When comparing the U.S. healthcare system to those of other developed countries, several key differences emerge. Countries with universal healthcare systems, such as Canada, the United Kingdom, and Australia, generally provide more equitable access to care and have lower healthcare costs per capita. However, these systems may also have longer wait times for certain services. Understanding these trade-offs is essential for evaluating the strengths and weaknesses of different healthcare models.
3.1 Canada: A Universal Healthcare Model
Canada’s healthcare system, often referred to as Medicare, is a publicly funded, universal healthcare system. It provides access to medically necessary services for all Canadian citizens and permanent residents. Healthcare is funded through taxes, and most services are provided by private doctors and hospitals. One of the main advantages of the Canadian system is its emphasis on equity and accessibility. However, the Canadian system also faces challenges, such as longer wait times for certain elective procedures and specialist appointments. Despite these challenges, Canada generally achieves comparable health outcomes to the U.S. at a lower cost.
3.2 The United Kingdom: The National Health Service (NHS)
The United Kingdom’s National Health Service (NHS) is another example of a universal healthcare system. The NHS provides healthcare services free at the point of use to all legal residents of the UK. It is funded through general taxation, and most healthcare providers are employed by the government. The NHS is known for its comprehensive coverage and emphasis on primary care. However, it also faces challenges, such as long wait times for certain services and budgetary constraints. Despite these challenges, the NHS generally achieves good health outcomes at a lower cost than the U.S.
3.3 Australia: A Mix of Public and Private Healthcare
Australia’s healthcare system is a mix of public and private insurance. Medicare, the public healthcare system, provides access to free or subsidized medical care for all Australian citizens and permanent residents. Private health insurance is also available and is often used to cover services not fully covered by Medicare, such as dental and vision care. Australia’s healthcare system is known for its relatively high quality and equitable access. However, it also faces challenges, such as rising healthcare costs and disparities in access to care for rural and indigenous populations.
4. The Impact of Healthcare Systems on Specific Health Outcomes
The design and implementation of a healthcare system can have a significant impact on specific health outcomes. By examining how different countries perform on key health indicators, we can gain insights into the strengths and weaknesses of their respective healthcare systems. This analysis can inform efforts to improve health outcomes in the U.S. by adopting best practices from other countries.
4.1 Cancer Survival Rates: A U.S. Strength
The U.S. generally has higher cancer survival rates compared to many other developed countries. This may be due to factors such as early detection, advanced treatment options, and greater access to specialized cancer care. However, these advantages come at a higher cost, and not all Americans have equal access to these services. While the U.S. excels in cancer care, it is important to consider whether these outcomes justify the higher costs and whether similar outcomes could be achieved more efficiently.
4.2 Infant and Maternal Mortality: Areas for Improvement
Infant and maternal mortality rates are areas where the U.S. lags behind many other developed countries. The U.S. has a higher infant mortality rate than most OECD countries, reflecting challenges in prenatal care, maternal health, and access to healthcare services for pregnant women and newborns. Maternal mortality rates in the U.S. have also been rising in recent years, which is a concerning trend. Addressing these issues requires a focus on improving access to prenatal care, addressing social determinants of health, and implementing evidence-based practices in maternal healthcare.
4.3 Chronic Disease Management: Prevention and Care Coordination
Chronic diseases, such as diabetes, heart disease, and obesity, are major health challenges in the U.S. The prevalence of these conditions is higher in the U.S. compared to many other developed countries, and the U.S. also spends more on managing these conditions. Improving chronic disease management requires a focus on prevention, early detection, and coordinated care. This includes promoting healthy lifestyles, providing access to preventive services, and implementing integrated care models that address the multiple needs of patients with chronic conditions.
5. Challenges and Opportunities for U.S. Healthcare Reform
The U.S. healthcare system faces numerous challenges, including high costs, uneven access to care, and variable quality outcomes. However, these challenges also present opportunities for reform. By learning from the experiences of other countries and implementing innovative solutions, the U.S. can improve the efficiency, equity, and quality of its healthcare system.
5.1 Addressing High Healthcare Costs
Addressing high healthcare costs is one of the most pressing challenges facing the U.S. healthcare system. Strategies to reduce costs include negotiating drug prices, promoting value-based payment models, and reducing administrative waste. Negotiating drug prices could significantly lower the cost of prescription medications, which are often much higher in the U.S. compared to other countries. Value-based payment models incentivize providers to deliver high-quality, cost-effective care, rather than simply billing for volume. Reducing administrative waste involves streamlining processes, standardizing billing practices, and investing in technology to improve efficiency.
5.2 Expanding Access to Care
Expanding access to care is crucial for improving health equity and overall population health in the U.S. Strategies to expand access include strengthening the Affordable Care Act, expanding Medicaid, and implementing a public health insurance option. Strengthening the ACA could involve increasing subsidies to make insurance more affordable and addressing gaps in coverage. Expanding Medicaid could provide coverage to more low-income individuals and families. A public health insurance option could provide a competitive alternative to private insurance plans and help drive down costs.
5.3 Improving Quality of Care and Patient Safety
Improving quality of care and patient safety is essential for ensuring that Americans receive the best possible medical care. Strategies to improve quality include implementing evidence-based practices, promoting patient-centered care, and enhancing quality measurement and reporting. Implementing evidence-based practices involves using the best available scientific evidence to guide clinical decision-making. Patient-centered care focuses on meeting the individual needs and preferences of patients. Enhancing quality measurement and reporting allows for the tracking of performance and identification of areas for improvement.
6. Innovations in Healthcare Delivery and Technology
Innovations in healthcare delivery and technology offer promising solutions for improving the efficiency, quality, and accessibility of healthcare services. Telehealth, artificial intelligence, and electronic health records are just a few examples of innovations that have the potential to transform healthcare. By embracing these technologies and implementing innovative delivery models, the U.S. can improve health outcomes and reduce costs.
6.1 Telehealth: Expanding Access to Remote Care
Telehealth, which involves the use of technology to provide healthcare services remotely, has the potential to expand access to care, particularly for patients in rural areas or those with limited mobility. Telehealth can be used for a variety of services, including consultations, monitoring, and education. The COVID-19 pandemic has accelerated the adoption of telehealth, and it is likely to play an increasingly important role in healthcare in the future.
6.2 Artificial Intelligence: Enhancing Diagnosis and Treatment
Artificial intelligence (AI) has the potential to enhance diagnosis and treatment by analyzing large amounts of data and identifying patterns that may not be apparent to human clinicians. AI can be used to improve the accuracy of diagnoses, personalize treatment plans, and predict patient outcomes. While AI is still in its early stages of development, it has the potential to revolutionize healthcare.
6.3 Electronic Health Records: Improving Care Coordination
Electronic health records (EHRs) can improve care coordination by providing a comprehensive and up-to-date view of a patient’s medical history. EHRs can facilitate communication between healthcare providers, reduce medical errors, and improve patient safety. While the adoption of EHRs has been widespread in the U.S., there is still work to be done to ensure that they are used effectively and that they are interoperable across different healthcare systems.
7. The Role of Policy and Regulation in Shaping Healthcare Systems
Policy and regulation play a crucial role in shaping healthcare systems. Government policies can influence healthcare spending, access to care, quality of services, and health outcomes. By implementing effective policies and regulations, policymakers can create a healthcare system that is more efficient, equitable, and effective.
7.1 The Affordable Care Act: Expanding Coverage and Improving Access
The Affordable Care Act (ACA) has been a landmark piece of legislation in the U.S. that has expanded health insurance coverage and improved access to care for millions of Americans. The ACA has also implemented several provisions aimed at improving the quality of care and reducing healthcare costs. While the ACA has faced challenges and criticisms, it has had a significant impact on the U.S. healthcare system.
7.2 Government Regulation of Healthcare Costs
Government regulation of healthcare costs can play a crucial role in controlling spending and ensuring that healthcare is affordable for all Americans. Strategies for regulating costs include negotiating drug prices, setting payment rates for healthcare services, and implementing cost-control measures in government-funded healthcare programs. Effective regulation can help to ensure that healthcare resources are used efficiently and that patients receive value for their money.
7.3 Ensuring Quality and Safety Through Regulation
Ensuring quality and safety through regulation is essential for protecting patients and promoting high-quality healthcare. Government regulations can set standards for healthcare providers, require quality reporting, and implement patient safety initiatives. Effective regulation can help to prevent medical errors, reduce hospital-acquired infections, and improve patient outcomes.
8. Future Trends in Healthcare: What to Expect
The healthcare landscape is constantly evolving, and it is important to stay informed about future trends. Emerging technologies, changing demographics, and evolving patient expectations are all shaping the future of healthcare. By understanding these trends, healthcare providers, policymakers, and patients can prepare for the challenges and opportunities that lie ahead.
8.1 Personalized Medicine: Tailoring Treatment to the Individual
Personalized medicine, which involves tailoring treatment to the individual based on their genetic makeup, lifestyle, and other factors, is a promising trend in healthcare. Personalized medicine has the potential to improve the effectiveness of treatments, reduce side effects, and improve patient outcomes. While personalized medicine is still in its early stages of development, it is likely to play an increasingly important role in healthcare in the future.
8.2 Aging Population: Addressing the Needs of Older Adults
The aging population is a major demographic trend that is shaping the future of healthcare. As the population ages, there will be a greater need for healthcare services for older adults, including geriatric care, long-term care, and chronic disease management. Addressing the needs of older adults will require a comprehensive approach that includes healthcare, social services, and community support.
8.3 Patient Empowerment: Engaging Patients in Their Own Care
Patient empowerment, which involves engaging patients in their own care and giving them more control over their healthcare decisions, is an important trend in healthcare. Empowered patients are more likely to adhere to treatment plans, make informed decisions, and achieve better health outcomes. Strategies for patient empowerment include providing patients with access to their medical records, offering patient education and support, and involving patients in shared decision-making.
9. Conclusion: Improving U.S. Healthcare Through Comparative Analysis
Comparative analysis of healthcare systems provides valuable insights into the strengths and weaknesses of the U.S. system. By learning from the experiences of other countries and implementing innovative solutions, the U.S. can improve the efficiency, equity, and quality of its healthcare system. Addressing high healthcare costs, expanding access to care, and improving quality of care are all essential for creating a healthcare system that meets the needs of all Americans. As healthcare continues to evolve, it is important to stay informed about future trends and to embrace innovation in order to improve health outcomes and reduce costs.
9.1 Key Takeaways and Recommendations
Here’s a summary of the key takeaways and recommendations from this comparative analysis:
- The U.S. spends more on healthcare per capita than any other developed country, but it does not consistently achieve better health outcomes.
- Access to care in the U.S. is often linked to insurance coverage and affordability, and a significant portion of the population remains uninsured or underinsured.
- The U.S. excels in some areas of quality of care, such as cancer survival rates, but it lags behind other developed countries in other key areas, such as infant and maternal mortality.
- Administrative inefficiencies contribute to higher costs in the U.S. healthcare system.
- Addressing high healthcare costs, expanding access to care, and improving quality of care are all essential for creating a more efficient, equitable, and effective healthcare system in the U.S.
9.2 Call to Action: Explore More Comparisons on COMPARE.EDU.VN
Ready to make informed decisions about your healthcare and understand the options available? Visit COMPARE.EDU.VN today for detailed comparisons, expert reviews, and comprehensive resources to help you navigate the complex world of healthcare. Whether you’re comparing insurance plans, treatment options, or healthcare providers, COMPARE.EDU.VN is your trusted source for objective information. Take control of your healthcare journey and explore the possibilities at COMPARE.EDU.VN.
Need more information or have questions? Contact us at 333 Comparison Plaza, Choice City, CA 90210, United States, or reach out via WhatsApp at +1 (626) 555-9090. Your health decisions matter, and compare.edu.vn is here to support you every step of the way.
10. Frequently Asked Questions (FAQ)
Here are some frequently asked questions about the U.S. healthcare system compared to other countries:
- Why is healthcare so expensive in the U.S.?
- Healthcare costs in the U.S. are driven by factors such as high drug prices, administrative inefficiencies, and a fee-for-service payment model.
- Does the U.S. have universal healthcare?
- No, the U.S. does not have a universal healthcare system. While programs like Medicare and Medicaid provide coverage to certain populations, a significant portion of the population remains uninsured.
- How does the U.S. healthcare system compare to Canada’s?
- Canada has a universal healthcare system that provides access to medically necessary services for all citizens. The U.S. relies on a mix of private and public insurance, leading to disparities in access and affordability.
- What are the main challenges facing the U.S. healthcare system?
- The main challenges include high costs, uneven access to care, and variable quality outcomes.
- What is the Affordable Care Act (ACA)?
- The ACA is a law that has expanded health insurance coverage and improved access to care for millions of Americans.
- How can the U.S. improve its healthcare system?
- The U.S. can improve its healthcare system by addressing high costs, expanding access to care, and improving quality of services.
- What role does technology play in healthcare?
- Technology, such as telehealth, artificial intelligence, and electronic health records, has the potential to improve the efficiency, quality, and accessibility of healthcare services.
- What is personalized medicine?
- Personalized medicine involves tailoring treatment to the individual based on their genetic makeup, lifestyle, and other factors.
- How is the aging population affecting healthcare?
- The aging population is increasing the need for healthcare services for older adults, including geriatric care and chronic disease management.
- What is patient empowerment?
- Patient empowerment involves engaging patients in their own care and giving them more control over their healthcare decisions.