1. INTRODUCTION
1.1. Background
It’s a well-known fact that the majority of emergency medical care for children is delivered in general emergency departments (EDs), rather than specialized pediatric EDs.[1] Numerous studies have highlighted significant disparities in both the quality of care and patient outcomes between general and pediatric EDs.[2, 3] For instance, children treated in general EDs are less likely to receive asthma care that adheres to established guidelines[4], and they are more prone to undergoing computed tomography (CT) scans for abdominal pain evaluation[2], potentially exposing them to higher doses of radiation.[5] A thorough understanding of the differences in quality and outcomes between these two types of emergency care settings is crucial for enhancing emergency medical services for children across all environments.
Much of the research in health services relies on large administrative datasets, such as the State Emergency Department Databases provided by the Agency for Healthcare Research and Quality (AHRQ). For studies aimed at comparing care quality or patient outcomes between pediatric and general EDs, a precise and reliable definition of what constitutes a “pediatric” ED is absolutely essential. However, current definitions of pediatric EDs are remarkably inconsistent. Some studies have categorized pediatric EDs based on self-reporting within a healthcare system[2] or the presence of a dedicated pediatric area.[6] Others have employed volume-based thresholds (e.g., >75% pediatric visits)[3] or the Children’s Hospital Association (CHA) roster of pediatric facilities.[5] A recent investigation utilized data from the American Hospital Association (AHA) survey on self-reported pediatric services[7] to classify hospitals as either pediatric or non-pediatric.
1.2. Importance
The considerable variation in how a pediatric ED is defined significantly undermines the validity of health services research in pediatric emergency medicine. Without a consistent and valid definition, it becomes impossible to reliably compare findings across different studies or to pinpoint the critical factors that contribute to better patient care. Furthermore, the AHA assigns unique identifiers to hospitals and hospital systems, which are frequently used to link databases for health services research purposes.[8, 9] Therefore, understanding how emergency care for children is represented in linked databases is of paramount importance for researchers planning to investigate pediatric care and outcomes using administrative data.
1.3. Goals of this investigation
The primary goal of this study was to assess how frequently an ED would be classified as “pediatric” when applying the most common definitions used in health services research. This Comparing Definition approach is crucial to understand the scope of variability and its implications.
2. METHODS
2.1. Study design, setting, and data collection
This study employed a cross-sectional design, utilizing linked data from two administrative databases: the AHRQ’s New York State Emergency Department Database and State Inpatient Database (SEDD/SID), and the National Emergency Department Inventory–USA (NEDI).[10] Detailed descriptions of the data collection methods for AHRQ data[11] and NEDI [12] have been previously published. We focused on data from the 2016 calendar year. The Partners Healthcare Human Research Committee reviewed and exempted this project from full review.
The Bottom Line.
Defining a pediatric emergency department (ED) accurately is a major hurdle in health services research. This study, analyzing linked data from two extensive administrative datasets, revealed a striking and broad variation in the number of EDs in New York State that met the criteria for being pediatric, based on four commonly applied definitions.
2.2. Administrative databases
We constructed a combined SEDD/SID-NEDI database, using SEDD/SID for patient visit data and NEDI for hospital characteristic data, such as the presence of a dedicated pediatric waiting area. SEDD/SID includes three hospital identifiers: the data source identifier (DSHOSPID), the AHA identifier (AHAID) for database linkage, and a unique Healthcare Cost and Utilization Project hospital identifier (HOSPID). In the New York data, HOSPID and AHAID have a one-to-one correspondence. NEDI also incorporates the AHAID for database linkage. Consequently, we utilized the unique hospital AHAID to link SEDD/SID data with NEDI data.[13]
The AHA frequently groups EDs by hospital network, meaning that SEDD-SID data may represent multiple EDs, whereas NEDI lists each ED individually. We applied a previously established matching algorithm to consolidate ED-specific NEDI data into observations for linkage with the AHA-based datasets.[13] When multiple NEDI EDs were matched to a single AHAID, data were aggregated into a single observation using sums or weighted averages of responses, as detailed in prior research.
2.3. Outcomes
We evaluated four distinct definitions of pediatric ED: (1) pediatric admission capability,[7] (2) physically distinct pediatric area within the ED,[6] (3) membership in the CHA,[14] and (4) volume of pediatric ED visits.[3] For pediatric admission capability, we gathered data on both pediatric bed availability, as reported in the AHA survey, and the presence of inpatient care for children, as indicated by SID pediatric admissions. Regarding a physically distinct pediatric area in the ED, the AHA definition refers to a hospital ED capable of stabilizing and managing pediatric patients, including transfer to a definitive care facility. In contrast, NEDI defines it more broadly as any dedicated physical ED space for children, even encompassing EDs with only a pediatric waiting room but shared treatment areas for adults and children. For volume of pediatric visits, we defined pediatric as ≥70% of ED visits being for the pediatric population (defined as patients <18 years of age in SEDD/SID data or using ED-specific pediatric cut-offs in NEDI).
2.4. Analysis
For each of the four definitions, we calculated the proportion of EDs that would be classified as pediatric. We then examined the variations in the number and demographic characteristics of patient visits that would be attributed to a pediatric ED, depending on the comparing definition used.
3. RESULTS
3.1. Inclusion
The combined/linked dataset included a total of 160 New York State EDs. EDs lacking AHAIDs in SEDD or not listed in the NEDI database were excluded.
3.2. Main outcomes
Across the four comparing definitions, the proportion of EDs meeting the criteria in the linked database varied significantly, ranging from 0% to 86% (Table 1). The definition based on admission capability was met by 86% of EDs. Between 27% and 38% of EDs reported having a physically distinct pediatric ED area (depending on the data source), and 8% were members of the CHA (Figure 1).
TABLE 1.
Number of emergency departments (EDs) captured by each definition of a pediatric ED, among a total of 160 EDs in New York state
| Category | Definition | Data source | EDs meeting definition, n (%) |
|---|---|---|---|
| Admission | AHA pediatric bed availability | AHA | 77 (48) |
| SID pediatric admissions | SID | 138 (86) | |
| Separate pediatric care area | AHA separate pediatric area | AHA | 60 (38) |
| NEDI separate pediatric area | NEDI | 43 (27) | |
| Membership | CHA membership | CHA | 13 (8) |
| Volume | SEDD/SID ≥70% visits of patients <18 years of age (after linkage) | SEDD/SID | 0 (0) |
| NEDI ≥70% visits defined as pediatric (generally patients <18 years of age) | NEDI | 3 (2) a |
AHA, American Hospital Association; CHA, Children’s Hospital Association; ED, emergency department; NEDI, National Emergency Department Inventory–USA; SEDD/SID, State Emergency Department Databases and State Inpatient Databases.
a From NEDI alone (not grouped by AHA identifiers for SEDD/SID merger).
FIGURE 1.
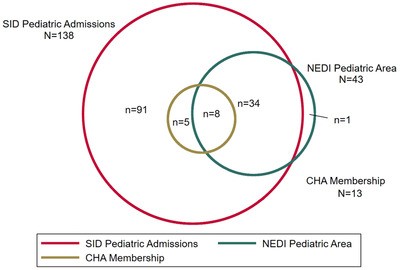 FIGURE 1
FIGURE 1
Number of emergency departments identified as pediatric by definition of pediatric ED, New York State 2016. Each circle represents a potential definition of a pediatric ED and shows the number of EDs that would be included within that definition; overlapping circles show EDs that would have qualified as a pediatric ED under more than 1 definition. CHA, Children’s Hospital Association; NEDI, National Emergency Department Inventory–USA; SID, State Inpatient Databases
Before database linkage, using only the individual hospital identifiers in SEDD/SID, three hospitals had over 70% pediatric ED visits. However, using the AHAID in SEDD/SID (as necessary for database linkage in future studies), no hospitals met the 70% cutoff for pediatric visits. Similarly, before linkage, 3 (2%) hospitals reported to NEDI that ≥70% visits were defined as pediatric. Thus, after creating the merged database, no hospitals satisfied the SEDD/SID criteria of ≥70% visits for patients <18 years of age in the merged SEDD/SID/NEDI database.
3.3. Patient visits and characteristics by pediatric ED definition
Using the merged SEDD/SID and NEDI dataset, the percentage of ED visits by children attributed to a pediatric ED varied from 30% to 97%, depending on the comparing definition of pediatric ED. Using pediatric bed availability, the proportion of visits was 78% (AHA). Applying the SID pediatric admission definition in the merged database captured 97% of pediatric ED visits. Based on having a separate pediatric area, the proportions were 73% (AHA) and 60% (NEDI). Only 30% of pediatric visits would have been attributed to a pediatric ED using the CHA membership definition (Table 2).
TABLE 2.
Demographics of children presenting to a pediatric ED, for each pediatric ED definition a
| AHA pediatric bed availability, n (%) | SID pediatric admissions, n (%) | AHA separate pediatric area, n (%) | NEDI separate pediatric area, n (%) | CHA membership, n (%) | Total, N (%) | |
|---|---|---|---|---|---|---|
| Overall | 1,192,215 (78) | 1,488,243 (97) | 1,111,176 (73) | 911,878 (60) | 453,793 (30) | 1,528,133 |
| Age, years | ||||||
| <1, infant | 146,844 (12) | 174,167 (12) | 138,976 (13) | 114,239 (13) | 62,047 (14) | 176,425 (12) |
| 1–11.9 | 745,693 (63) | 920,077 (62) | 701,949 (63) | 583,194 (64) | 284,095 (63) | 943,418 (62) |
| 12–17.9 | 299,678 (25) | 393,999 (26) | 270,251 (24) | 214,445 (24) | 107,651 (24) | 408,290 (27) |
| Race/ethnicity | ||||||
| Non‐Hispanic White | 320,597 (27) | 443,321 (30) | 235,758 (21) | 144,537 (16) | 132,283 (30) | 471,262 (31) |
| Non‐Hispanic Black | 271,445 (23) | 346,647 (23) | 270,867 (24) | 251,327 (28) | 82,826 (18) | 353,347 (23) |
| Hispanic | 324,832 (27) | 387,372 (26) | 335,637 (30) | 290,985 (32) | 104,660 (23) | 389,987 (26) |
| Other race/ethnicity | 275,341 (23) | 310,903 (21) | 268,914 (24) | 225,029 (25) | 134,024 (30) | 313,537 (21) |
| Type of insurance | ||||||
| Private insurance | 320,822 (27) | 412,142 (28) | 290,961 (26) | 208,488 (23) | 153,887 (34) | 426,603 (28) |
| Public insurance | 774,603 (65) | 943,263 (63) | 731,287 (66) | 625,296 (69) | 269,650 (59) | 965,988 (63) |
| No insurance | 82,499 (7) | 102,423 (7) | 79,501 (7) | 67,378 (7) | 24,304 (5) | 104,503 (7) |
| Other b | 14,009 (1) | 30,056 (2) | 9,273 (1) | 10,503 (1) | 5,951 (1) | 30,676 (2) |
| Missing insurance information | 282 (0.02) | 359 (0.02) | 154 (0.01) | 213 (0.02) | 1 (0) | 363 (0.02) |
Each column represents a definition of a pediatric ED and the demographic of the visits that would have been reported as presenting to a “pediatric ED” in a research study using that definition. AHA, American Hospital Association; CHA, Children’s Hospital Association; CHAMPUS, Civilian Health and Medical Program of the Uniformed Services; CHAMPVA, Civilian Health and Medical Program of the Department of Veterans Affairs; NEDI, National Emergency Department Inventory–USA; SEDD/SID, State Emergency Department Databases and State Inpatient Databases.
a We were unable to calculate demographics for the following definitions: SEDD/SID ≥70% visits of patients <18 years of age and NEDI ≥70% visits defined as pediatric because of the limitations of the data merge based on AHA identifiers.
b Other includes pediatric ED visits with no charge or used other type of insurance (Worker’s Compensation, CHAMPUS, CHAMPVA, Title V, or other government programs).
Patient characteristics also varied based on the comparing definition utilized (Table 2). While the proportion of visits by infants (<1 year) seen in a pediatric ED remained relatively consistent across definitions, the percentages for children of other age groups also remained fairly stable. However, the proportions of visits by Black, Hispanic, and White children attributed to a pediatric ED showed greater variability across definitions (Table 2). Among ED visits by non-Hispanic Black children in our cohort, the percentage attributed to a pediatric ED ranged from 18% to 28%, for Hispanic children from 23% to 32%, and for non-Hispanic White children from 16% to 30%. Using the CHA membership definition resulted in the highest percentage of visits for White children being categorized as pediatric and the lowest for non-Hispanic Black and Hispanic children. Similar trends were observed for insurance type, where the proportion of children with public insurance seen in pediatric EDs varied from 59% to 69%, depending on the definition, with the highest percentage based on the NEDI pediatric area and the lowest percentages for definitions based on CHA membership.
4. DISCUSSION
Our study clearly demonstrates that the number of EDs identified as pediatric, the percentage of visits attributed to a pediatric ED, and the demographic characteristics of the pediatric population seen in a “pediatric” ED all fluctuate significantly depending on the comparing definition employed. Even definitions that appear to measure similar aspects (e.g., admission capability in SID and bed availability in AHA) still captured different sets of EDs and patient populations (see Figure 1). These findings also highlight the challenges associated with using AHAIDs for linking datasets. The AHA’s practice of grouping EDs by hospital network can complicate the calculation of volume-based ED metrics for specific locations. Given the frequent use of SEDDs/SIDs for evaluating emergency services and health services research,[9, 11, 15, 16, 17, 18] it is crucial for researchers to understand the limitations of these databases in identifying primary pediatric hospitals within larger healthcare systems. Specifically, recognizing how standardized linkage methodologies can obscure pediatric volume within medical systems is vital, particularly for researchers intending to study pediatric care in general EDs or to compare pediatric care between general and pediatric EDs. Our data reveal 13 CHA member hospitals that would not be identified as pediatric centers based on volume criteria in linked data, and three pediatric centers in each of the unlinked NEDI and SEDD/SID datasets that would be masked in linked data.
Because the demographic profiles of patients treated varied with the selected definition, even basic descriptive studies of populations treated in “pediatric” or “general” EDs can be meaningfully impacted by the choice of definition. This variability may hinder our ability to identify disparities in care and outcomes. For example, a study using CHA membership criteria would include a higher proportion of non-Hispanic White and privately insured patients as pediatric visits compared to a study using AHA pediatric bed availability criteria. These inherent differences have the potential to introduce bias into studies examining care provided to diverse populations in general and pediatric EDs. Therefore, careful consideration of the chosen definition is critically important for researchers planning to investigate pediatric emergency care.
This study has several important limitations. Given that over 90% of ED visits by children are reported to occur in non-specialty facilities (general EDs),[1] the percentage of pediatric visits attributed to pediatric EDs in our data is higher than expected. This may reflect a greater prevalence of pediatric specialty care in New York State compared to other regions of the United States, the broadness of the definitions examined, or the linkage methodology itself.
There is no universally accepted “gold standard” definition of a pediatric ED for comparison. For volume-based definitions, using AHA hospital identification codes to merge SEDD/SID and NEDI data resulted in the aggregation of pediatric and adult facilities within the same organization. This aggregation makes it challenging to identify pediatric hospitals based on volume criteria in the merged dataset. We present data from a single state, although New York is a diverse state with both urban and rural areas. Furthermore, we were unable to capture data on physician staffing (e.g., pediatric emergency medicine (PEM) fellowship training), nurse staffing, or other hospital characteristics that could influence care outcomes for children in pediatric EDs and potentially serve as alternative definitions. Future research should focus on collecting data on pediatric-specific staffing to assess the specific impact of PEM-trained clinicians on care and outcomes for pediatric patients, as staffing may be a more influential factor than the definitions we explored. Additionally, replicating these analyses in different states is necessary to better understand how to accurately identify pediatric hospitals in administrative data.
In conclusion, the merged SEDD-SID-NEDI database serves as a representative example of a linked dataset used to explore various health services research questions related to pediatric emergency care and to illustrate the limitations of such databases for pediatric health services research. Our findings emphasize the crucial need for careful attention to the definition comparison and selection of a pediatric ED definition when examining hospital quality and comparing quality and outcomes between pediatric and general EDs. Currently, there is no standardized definition of a “pediatric ED”. The number of EDs identified and the characteristics of ED patients seen vary depending on the definition used. Volume-based definitions, in particular, may hinder the identification of pediatric hospitals. Therefore, an improved, ideally consensus-driven, definition of a pediatric ED is urgently needed. Such a definition would facilitate the accurate representation of pediatric EDs in national databases and support initiatives to improve the quality of emergency care provided to all children. In the meantime, we urge researchers and policymakers to be mindful of this ambiguity and how different definitions can influence research outcomes.
CONFLICTS OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
MSK wrote the manuscript and conceptualized and designed the study. AS and CC conceptualized and designed the study, assisted with interpretation of the results, and critically reviewed the manuscript for important intellectual content. KB oversaw data collection for NEDI, created the combined data set for use in the study, and reviewed the manuscript for important intellectual content. JG conducted the data analysis, and reviewed and revised the manuscript. EA assisted with interpretation of the results and critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
5. ACKNOWLEDGMENTS
This analysis was supported by a grant from R Baby Foundation (New York, NY). Dr. Samuels-Kalow is supported by the Harvard Catalyst, The Harvard Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health Award UL 1TR002541) and financial contributions from Harvard University and its affiliated academic healthcare centers. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic healthcare centers, nor the National Institutes of Health.
Biography
Margaret E. Samuels-Kalow, MD, MPhil, is an Associate Professor of Emergency Medicine and Pediatrics at Harvard Medical School and an Attending Physician in both emergency medicine and pediatric emergency medicine at Massachusetts General Hospital.
Samuels-Kalow ME, Sullivan AF, Boggs KM, Gao J, Alpern ER, Camargo Jr CA. Comparing definitions of a pediatric emergency department. JACEP Open. 2021;2:e12478. 10.1002/emp2.12478
Supervising Editor: Benjamin Kerrey, MD, MS.
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org ). The authors have stated that no such relationships exist.