Which Best Compares Self Renewal And Differentiation in the context of hematopoietic stem cells (HSCs)? Self-renewal enables HSCs to maintain their population over time, while differentiation allows them to produce various blood cell types; understanding this balance is crucial for regenerative medicine and treating blood disorders, as explored comprehensively on COMPARE.EDU.VN. This article delves into the intricacies of these processes, examining clonal behaviors, differentiation patterns, and the impact of factors like aging and stress, and ultimately providing insights into stem cell fate decisions, clonal hematopoiesis, and cellular expansion.
1. What Is Self-Renewal and Differentiation and How Are They Compared in Hematopoietic Stem Cells (HSCs)?
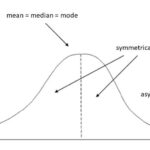
Self-renewal is the ability of a stem cell to divide and create more stem cells identical to itself, ensuring a stable pool of stem cells. Differentiation is the process by which a stem cell transforms into specialized cell types with specific functions. In HSCs, self-renewal maintains the HSC population in the bone marrow, while differentiation produces all the different types of blood cells, such as red blood cells, white blood cells, and platelets. Comparing these two processes involves understanding their balance, regulation, and how they are affected by various factors.
-
Self-Renewal: The hallmark of stem cells is their capacity to self-replicate, ensuring a persistent pool of these cells throughout an organism’s lifespan. This process is tightly regulated to prevent depletion or excessive proliferation, which can lead to diseases like cancer.
-
Differentiation: The ability of stem cells to transform into specialized cell types is critical for tissue maintenance and repair. This process involves a series of steps guided by various signaling pathways and transcription factors, which ultimately define the cell’s identity and function.
-
Balance: Maintaining a delicate balance between self-renewal and differentiation is crucial for tissue homeostasis. Disruptions in this balance can lead to various disorders, including anemia, immunodeficiency, and leukemia.
2. How Does Clonal Analysis Help in Comparing Self-Renewal and Differentiation?
Clonal analysis involves tracking individual stem cells and their progeny to understand their self-renewal and differentiation patterns. By labeling HSCs with unique “barcodes,” researchers can follow the fate of each cell and its descendants over time. This approach provides insights into the heterogeneity of HSCs, revealing that some HSCs are more prone to self-renewal, while others are more likely to differentiate into specific blood cell types.
-
Barcoding Techniques: These methods use genetic markers or unique DNA sequences to label individual stem cells and trace their lineage. This allows researchers to track the self-renewal and differentiation patterns of each cell and its progeny.
-
Heterogeneity: Clonal analysis has revealed that HSCs are not a homogenous population. Some HSCs are more likely to self-renew and maintain the stem cell pool, while others are more prone to differentiation into specific blood cell types.
-
Fate Mapping: By following the fate of individual HSCs and their progeny, researchers can map the differentiation pathways and identify key regulatory factors involved in lineage commitment.
3. What Are the Key Differentiation Patterns Observed in HSCs?
HSCs exhibit diverse differentiation patterns, including:
- Balanced Differentiation: Production of all types of blood cells in roughly equal proportions.
- Myeloid-Biased Differentiation: Predominant production of myeloid cells, such as granulocytes and monocytes.
- Lymphoid-Biased Differentiation: Predominant production of lymphoid cells, such as B cells and T cells.
- Megakaryocyte-Restricted Differentiation: Primarily production of megakaryocytes, which produce platelets.
Understanding these patterns is essential for tailoring therapies to specific blood disorders, as discussed in detail on COMPARE.EDU.VN.
-
Factors Influencing Differentiation: Various factors, including age, inflammation, and genetic mutations, can influence the differentiation patterns of HSCs. For example, aging is often associated with myeloid-biased differentiation, which can increase the risk of myeloid malignancies.
-
Clinical Relevance: Understanding the differentiation patterns of HSCs is critical for developing targeted therapies for blood disorders. For example, in some cases, it may be desirable to promote lymphoid differentiation to boost the immune system, while in others, it may be necessary to suppress myeloid differentiation to prevent leukemia.
4. How Does Aging Affect Self-Renewal and Differentiation in HSCs?
Aging significantly impacts HSC function. Aged HSCs tend to exhibit increased self-renewal but reduced differentiation potential, often leading to a myeloid-biased output. This shift can result in decreased immune function and an increased risk of myeloid malignancies.
-
Increased Self-Renewal: Aged HSCs often show an increased propensity for self-renewal, leading to an expansion of the HSC pool. However, this expansion is not necessarily beneficial, as it can be associated with genomic instability and clonal dominance.
-
Reduced Differentiation Potential: Aged HSCs may lose their ability to differentiate into all blood cell types, resulting in a biased output. This can lead to a decline in immune function and an increased risk of anemia.
-
Myeloid Bias: Aging is often associated with a shift towards myeloid-biased differentiation, which can increase the risk of myeloid malignancies, such as acute myeloid leukemia (AML).
5. What Role Does the Microenvironment Play in Regulating HSC Self-Renewal and Differentiation?
The bone marrow microenvironment, or niche, provides critical signals that regulate HSC self-renewal and differentiation. Factors such as cell-cell interactions, growth factors, and cytokines influence HSC fate decisions. Disruptions in the microenvironment can impair HSC function and contribute to blood disorders.
-
Cell-Cell Interactions: Direct contact between HSCs and other cells in the bone marrow, such as stromal cells and osteoblasts, can provide critical signals that regulate self-renewal and differentiation.
-
Growth Factors and Cytokines: Various growth factors and cytokines, such as thrombopoietin (TPO), stem cell factor (SCF), and interleukin-3 (IL-3), play important roles in HSC survival, proliferation, and differentiation.
-
Hypoxia: The low oxygen tension in the bone marrow microenvironment can promote HSC quiescence and self-renewal, while inhibiting differentiation.
6. How Do Genetic and Epigenetic Factors Influence HSC Self-Renewal and Differentiation?
Genetic mutations and epigenetic modifications can profoundly influence HSC self-renewal and differentiation. Mutations in genes involved in DNA methylation, chromatin remodeling, and transcription factor function can alter HSC fate decisions and contribute to clonal hematopoiesis and blood disorders.
-
Genetic Mutations: Mutations in genes such as TET2, DNMT3A, and ASXL1 are commonly found in HSCs and can alter their self-renewal and differentiation patterns. These mutations can lead to clonal hematopoiesis and increase the risk of blood disorders.
-
Epigenetic Modifications: Epigenetic modifications, such as DNA methylation and histone modifications, play a critical role in regulating gene expression and influencing HSC fate decisions. Aberrant epigenetic modifications can disrupt normal HSC function and contribute to disease.
-
Transcription Factors: Transcription factors, such as GATA-1, PU.1, and RUNX1, are essential for regulating lineage-specific gene expression and directing HSC differentiation. Mutations or dysregulation of these factors can lead to lineage-biased differentiation or differentiation arrest.
7. What Is Clonal Hematopoiesis and How Does It Relate to Self-Renewal and Differentiation?
Clonal hematopoiesis is the expansion of a single HSC clone with a specific genetic or epigenetic alteration. This phenomenon is common in aging and is often driven by mutations that enhance self-renewal. While many individuals with clonal hematopoiesis remain healthy, it increases the risk of developing blood cancers and cardiovascular disease. COMPARE.EDU.VN provides a detailed analysis of the risks associated with clonal hematopoiesis.
-
Driver Mutations: Clonal hematopoiesis is often driven by mutations in genes that regulate self-renewal, such as DNMT3A, TET2, and ASXL1. These mutations confer a competitive advantage to the affected HSCs, allowing them to expand and outcompete normal HSCs.
-
Age-Related Phenomenon: Clonal hematopoiesis becomes more prevalent with age, likely due to the accumulation of genetic and epigenetic alterations in HSCs over time.
-
Risk Factor for Disease: While many individuals with clonal hematopoiesis remain healthy, it is associated with an increased risk of developing blood cancers, such as acute myeloid leukemia (AML), and cardiovascular disease.
8. How Does 5-Fluorouracil (5-FU) Treatment Affect HSC Self-Renewal and Differentiation?
5-FU is a chemotherapy drug that damages DNA and preferentially kills rapidly dividing cells. In the context of HSCs, 5-FU treatment can initially deplete the HSC pool but is followed by a regenerative phase where the surviving HSCs repopulate the bone marrow. This process can alter the self-renewal and differentiation dynamics of HSCs, sometimes leading to a myeloid-biased output.
-
Depletion of HSCs: 5-FU treatment initially depletes the HSC pool, particularly the more proliferative HSCs.
-
Regenerative Phase: After 5-FU treatment, the surviving HSCs repopulate the bone marrow, leading to a regenerative phase of hematopoiesis.
-
Myeloid Bias: 5-FU treatment can sometimes lead to a myeloid-biased output, potentially due to the selective survival and expansion of myeloid-biased HSCs.
9. What Are the Implications of HSC Self-Renewal and Differentiation for Regenerative Medicine?
Understanding the mechanisms that govern HSC self-renewal and differentiation is crucial for regenerative medicine. By manipulating these processes, researchers aim to develop therapies that can regenerate healthy blood cells in patients with blood disorders, such as anemia, immunodeficiency, and leukemia.
-
Stem Cell Transplantation: HSC transplantation is a well-established regenerative medicine approach for treating blood disorders. By transplanting healthy HSCs into patients, it is possible to restore normal blood cell production.
-
Ex Vivo Expansion: Researchers are developing methods to expand HSCs ex vivo (outside the body) to generate larger numbers of cells for transplantation. This approach could overcome the limitations of donor availability and improve the success of transplantation.
-
Directed Differentiation: By understanding the signaling pathways and transcription factors that regulate HSC differentiation, researchers aim to develop methods to direct HSCs to differentiate into specific blood cell types, such as red blood cells or platelets.
10. How Can COMPARE.EDU.VN Help in Understanding HSC Self-Renewal and Differentiation?
COMPARE.EDU.VN serves as a valuable resource for comparing and understanding complex biological processes like HSC self-renewal and differentiation. The website offers detailed analyses, comparisons of different research findings, and insights into the latest advancements in the field. It helps students, researchers, and healthcare professionals stay informed and make well-informed decisions about regenerative medicine and treatment strategies for blood disorders.
-
Detailed Analyses: COMPARE.EDU.VN provides in-depth analyses of the mechanisms and factors that regulate HSC self-renewal and differentiation.
-
Comparative Research: The website offers comparisons of different research findings, helping users to understand the complexities and controversies in the field.
-
Latest Advancements: COMPARE.EDU.VN keeps users informed about the latest advancements in HSC research, including new technologies, therapies, and clinical trials.
11. What Techniques Are Used to Analyze Clonal Behavior and Differentiation Patterns of Hematopoietic Stem Cells?
Several advanced techniques are employed to analyze the clonal behavior and differentiation patterns of hematopoietic stem cells (HSCs). These techniques provide insights into how HSCs self-renew and differentiate into various blood cell types. Some of the key methods include:
-
Transposon-Mediated Tagging:
- Mechanism: This method uses transposons (mobile genetic elements) to insert unique DNA “tags” into the genome of HSCs. These tags act as barcodes, allowing researchers to track the clonal descendants of individual HSCs.
- Application: By analyzing the distribution of these tags in different blood cell populations, scientists can reconstruct the differentiation patterns of HSCs and identify clones that are biased towards specific lineages.
-
Cre-Based Lineage Tracing:
- Mechanism: This technique involves using the Cre recombinase enzyme to activate or delete specific genes in HSCs, thereby marking them and their progeny. The Cre enzyme is typically placed under the control of a promoter that is active only in HSCs.
- Application: Cre-based lineage tracing allows researchers to follow the fate of HSCs and their descendants over time, providing direct evidence of HSC differentiation and self-renewal.
-
Single-Cell RNA Sequencing (scRNA-seq):
- Mechanism: scRNA-seq involves isolating individual HSCs and sequencing their RNA to determine the expression levels of thousands of genes. This technique provides a snapshot of the transcriptional state of each cell.
- Application: By analyzing scRNA-seq data, researchers can identify distinct subpopulations of HSCs with different differentiation potentials and track the changes in gene expression that occur during HSC differentiation.
-
Flow Cytometry and Cell Sorting:
- Mechanism: Flow cytometry is a technique that allows researchers to identify and isolate specific cell populations based on the expression of surface markers. Cells are labeled with fluorescent antibodies that bind to specific surface proteins, and then passed through a laser beam. The light scattered by each cell is measured, allowing for the identification and quantification of different cell types.
- Application: Flow cytometry is often used in conjunction with cell sorting to isolate HSCs and their progeny for further analysis, such as scRNA-seq or transposon-mediated tagging.
-
Limiting Dilution Assays:
- Mechanism: Limiting dilution assays involve transplanting decreasing numbers of HSCs into recipient mice to determine the frequency of HSCs that are capable of long-term engraftment and multi-lineage reconstitution.
- Application: This technique provides a functional measure of HSC self-renewal and differentiation potential.
-
CRISPR-Based Barcoding:
- Mechanism: CRISPR-based barcoding involves using the CRISPR-Cas9 system to introduce random insertions and deletions (indels) into a specific genomic locus in HSCs. These indels act as unique barcodes that can be used to track the clonal descendants of individual HSCs.
- Application: This technique offers a high-throughput approach for tracking HSC clones and analyzing their differentiation patterns.
These techniques, often used in combination, provide a comprehensive toolkit for dissecting the clonal behavior and differentiation patterns of HSCs, thereby enhancing our understanding of hematopoiesis and related disorders.
12. What Are the Key Signaling Pathways Involved in HSC Self-Renewal and Differentiation?
Hematopoietic stem cell (HSC) self-renewal and differentiation are intricately regulated by a network of signaling pathways. These pathways respond to various intrinsic and extrinsic cues, orchestrating the balance between maintaining the HSC pool and producing differentiated blood cells. Key signaling pathways include:
-
Wnt Signaling:
- Role: The Wnt signaling pathway plays a critical role in HSC self-renewal, proliferation, and maintenance. Activation of Wnt signaling can promote HSC expansion, while inhibition can drive differentiation.
- Mechanism: Wnt ligands bind to Frizzled receptors on the cell surface, leading to the activation of downstream signaling cascades, including the stabilization of β-catenin. β-catenin then translocates to the nucleus, where it interacts with transcription factors to regulate the expression of target genes involved in HSC self-renewal.
-
Notch Signaling:
- Role: Notch signaling is essential for HSC self-renewal and lineage commitment. It regulates the balance between quiescence and proliferation, as well as the differentiation of HSCs into specific blood cell types.
- Mechanism: Notch receptors interact with ligands on neighboring cells, leading to proteolytic cleavage of the Notch receptor and release of the Notch intracellular domain (NICD). NICD translocates to the nucleus, where it interacts with transcription factors to regulate the expression of target genes involved in HSC fate decisions.
-
Hedgehog Signaling:
- Role: The Hedgehog (Hh) signaling pathway is involved in HSC self-renewal and maintenance. It promotes the expansion of HSCs and regulates their interactions with the bone marrow microenvironment.
- Mechanism: Hh ligands bind to the Patched (Ptch) receptor, relieving its inhibition of the Smoothened (Smo) receptor. Smo then activates downstream signaling cascades, leading to the activation of transcription factors that regulate the expression of target genes involved in HSC self-renewal.
-
TGF-β Signaling:
- Role: The transforming growth factor-beta (TGF-β) signaling pathway plays a complex role in HSC regulation. It can promote quiescence and inhibit proliferation in HSCs, as well as regulate their differentiation into specific blood cell types.
- Mechanism: TGF-β ligands bind to TGF-β receptors on the cell surface, leading to the activation of downstream signaling cascades, including the phosphorylation of Smad proteins. Smad proteins then translocate to the nucleus, where they interact with transcription factors to regulate the expression of target genes involved in HSC fate decisions.
-
PI3K/Akt/mTOR Signaling:
- Role: The phosphatidylinositol 3-kinase (PI3K)/Akt/mammalian target of rapamycin (mTOR) signaling pathway is involved in HSC proliferation, survival, and metabolism. Activation of this pathway can promote HSC expansion, while inhibition can induce quiescence.
- Mechanism: Growth factors and cytokines activate PI3K, which phosphorylates phosphatidylinositol-4,5-bisphosphate (PIP2) to generate phosphatidylinositol-3,4,5-trisphosphate (PIP3). PIP3 then recruits Akt to the cell membrane, where it is phosphorylated and activated. Activated Akt phosphorylates and activates mTOR, which regulates protein synthesis and cell growth.
-
JAK/STAT Signaling:
- Role: The Janus kinase (JAK)/signal transducer and activator of transcription (STAT) signaling pathway is essential for HSC self-renewal, differentiation, and response to cytokines. It mediates the effects of various cytokines, such as thrombopoietin (TPO) and erythropoietin (EPO), on HSCs.
- Mechanism: Cytokines bind to their receptors on the cell surface, leading to the activation of JAKs. Activated JAKs phosphorylate STATs, which then dimerize and translocate to the nucleus, where they interact with transcription factors to regulate the expression of target genes involved in HSC fate decisions.
Understanding these signaling pathways and their interplay is crucial for developing targeted therapies that can modulate HSC self-renewal and differentiation for regenerative medicine and the treatment of blood disorders.
13. How Does the Bone Marrow Niche Influence HSC Fate?
The bone marrow niche is the microenvironment in which hematopoietic stem cells (HSCs) reside. It provides essential signals and interactions that regulate HSC self-renewal, differentiation, and mobilization. Key components of the bone marrow niche include:
-
Cellular Components:
- Mesenchymal Stem Cells (MSCs): MSCs secrete growth factors and cytokines that support HSC survival and self-renewal. They also contribute to the formation of the extracellular matrix.
- Osteoblasts: Osteoblasts are bone-forming cells that play a role in HSC maintenance. HSCs are often found in close proximity to osteoblasts in the endosteal niche.
- Endothelial Cells: Endothelial cells line the blood vessels in the bone marrow and regulate HSC trafficking and mobilization.
- Macrophages: Macrophages are immune cells that can either support or suppress HSC function, depending on their activation state.
- Megakaryocytes: Megakaryocytes produce platelets and secrete factors that regulate HSC self-renewal and differentiation.
-
Extracellular Matrix (ECM):
- Composition: The ECM is a complex network of proteins and polysaccharides that provides structural support and biochemical cues to HSCs. Key components of the ECM include collagen, fibronectin, laminin, and hyaluronic acid.
- Function: The ECM regulates HSC adhesion, migration, and signaling. It also provides a reservoir for growth factors and cytokines.
-
Soluble Factors:
- Growth Factors: Growth factors such as stem cell factor (SCF), thrombopoietin (TPO), and Flt3 ligand promote HSC survival, self-renewal, and proliferation.
- Cytokines: Cytokines such as interleukin-3 (IL-3), interleukin-6 (IL-6), and granulocyte colony-stimulating factor (G-CSF) regulate HSC differentiation and mobilization.
- Chemokines: Chemokines such as CXCL12 and CXCL4 regulate HSC trafficking and localization within the bone marrow.
-
Physical Factors:
- Hypoxia: The bone marrow is a relatively hypoxic environment, which promotes HSC quiescence and self-renewal.
- Mechanical Forces: Mechanical forces such as fluid shear stress and matrix stiffness can influence HSC fate decisions.
The bone marrow niche regulates HSC fate through a combination of these cellular, molecular, and physical factors. Disruptions in the niche can impair HSC function and contribute to blood disorders such as myelodysplastic syndromes (MDS) and acute myeloid leukemia (AML).
14. What Are the Clinical Implications of Understanding HSC Self-Renewal and Differentiation?
A deeper understanding of HSC self-renewal and differentiation has profound clinical implications, impacting the treatment of various hematological disorders and advancing regenerative medicine:
-
Improved Stem Cell Transplantation:
- Optimized HSC Expansion: Knowledge of self-renewal pathways allows for ex vivo expansion of HSCs, increasing the number of cells available for transplantation. This is particularly useful when dealing with limited donor material.
- Enhanced Engraftment: Manipulating the differentiation pathways can improve the engraftment efficiency of transplanted HSCs, reducing the risk of graft failure and improving patient outcomes.
-
Targeted Therapies for Hematological Malignancies:
- Disrupting Malignant Clones: Understanding the signaling pathways that drive the proliferation and survival of malignant HSCs can lead to the development of targeted therapies that specifically disrupt these clones.
- Restoring Normal Hematopoiesis: Therapies aimed at restoring normal differentiation pathways can help to re-establish a healthy balance of blood cell production in patients with leukemia and myelodysplastic syndromes.
-
Regenerative Medicine Applications:
- Blood Disorder Treatment: Directing HSC differentiation towards specific lineages can provide a source of functional blood cells for patients with anemia, thrombocytopenia, or immune deficiencies.
- Gene Therapy Delivery: HSCs can be used as a vehicle for delivering gene therapy to treat genetic blood disorders. By correcting the genetic defect in HSCs, it is possible to achieve long-term correction of the disease.
-
Personalized Medicine Approaches:
- Risk Stratification: Identifying genetic and epigenetic markers that predict HSC self-renewal and differentiation potential can help to stratify patients based on their risk of developing hematological malignancies.
- Tailored Treatment Strategies: Understanding the individual characteristics of a patient’s HSCs can inform the development of personalized treatment strategies that are tailored to their specific needs.
-
Drug Discovery and Development:
- Screening Assays: HSC self-renewal and differentiation assays can be used to screen for novel drugs that modulate these processes.
- Mechanism of Action Studies: Understanding the molecular mechanisms by which drugs affect HSCs can help to optimize their use and minimize side effects.
-
Aging-Related Blood Disorders:
- Counteracting Age-Related Changes: Strategies aimed at counteracting the age-related decline in HSC function can help to prevent or delay the onset of blood disorders in older adults.
- Promoting Healthy Aging: Understanding how HSC self-renewal and differentiation change with age can provide insights into the mechanisms of healthy aging and potential interventions to promote longevity.
These clinical implications underscore the importance of continued research into the fundamental mechanisms of HSC self-renewal and differentiation, highlighting the potential for these discoveries to improve human health.
15. What Are the Recent Advances in Understanding HSC Self-Renewal and Differentiation?
Recent advances in understanding hematopoietic stem cell (HSC) self-renewal and differentiation are revolutionizing our approach to treating blood disorders and advancing regenerative medicine. Key developments include:
-
Single-Cell Multiomics:
- Advancement: Combining single-cell RNA sequencing (scRNA-seq) with other omics technologies, such as ATAC-seq (assay for transposase-accessible chromatin) and proteomics, provides a more comprehensive view of HSC heterogeneity and differentiation.
- Impact: This approach allows researchers to link gene expression patterns with chromatin accessibility and protein levels, revealing the regulatory mechanisms that govern HSC fate decisions.
-
CRISPR-Based Gene Editing:
- Advancement: CRISPR-Cas9 technology enables precise editing of the genome in HSCs, allowing for the correction of genetic defects and the manipulation of signaling pathways that regulate self-renewal and differentiation.
- Impact: CRISPR-based gene editing holds great promise for treating genetic blood disorders such as sickle cell anemia and beta-thalassemia.
-
3D Culture Systems:
- Advancement: 3D culture systems that mimic the bone marrow microenvironment provide a more physiologically relevant platform for studying HSC self-renewal and differentiation in vitro.
- Impact: These systems allow researchers to investigate the role of cell-cell interactions, extracellular matrix components, and soluble factors in regulating HSC fate decisions.
-
Metabolic Regulation of HSCs:
- Advancement: Recent studies have revealed that metabolic pathways play a critical role in regulating HSC self-renewal and differentiation.
- Impact: Understanding the metabolic requirements of HSCs can lead to the development of novel strategies for manipulating their fate, such as targeting specific metabolic enzymes or providing metabolic support.
-
Epigenetic Regulation of HSCs:
- Advancement: Epigenetic modifications, such as DNA methylation and histone modifications, are increasingly recognized as key regulators of HSC self-renewal and differentiation.
- Impact: Targeting epigenetic enzymes with small-molecule inhibitors can alter HSC fate decisions and may have therapeutic potential for treating blood disorders.
-
Immunomodulation of HSCs:
- Advancement: The immune system plays a complex role in regulating HSC self-renewal and differentiation.
- Impact: Immunomodulatory therapies, such as checkpoint inhibitors and cytokine blockade, can influence HSC function and may have therapeutic potential for treating bone marrow failure syndromes and other blood disorders.
-
Lineage Tracing Technologies:
- Advancement: Improved lineage tracing technologies, such as CRISPR-based barcoding and multicolor lineage tracing, allow for more precise tracking of HSC clones and their differentiation patterns.
- Impact: These technologies provide a deeper understanding of HSC heterogeneity and the clonal dynamics of hematopoiesis.
-
Artificial Intelligence and Machine Learning:
- Advancement: Artificial intelligence (AI) and machine learning (ML) are being used to analyze large datasets from HSC studies, such as scRNA-seq and flow cytometry data.
- Impact: AI and ML can identify novel patterns and relationships in the data, leading to new insights into HSC self-renewal and differentiation.
These recent advances highlight the rapid progress being made in our understanding of HSC biology and the potential for these discoveries to transform the treatment of blood disorders and advance regenerative medicine.
Navigating the complexities of self-renewal and differentiation requires a reliable source of information. Visit COMPARE.EDU.VN, your guide to making informed comparisons and decisions. For inquiries, reach out to us at 333 Comparison Plaza, Choice City, CA 90210, United States, or contact us via Whatsapp at +1 (626) 555-9090.
Understanding the intricacies of self-renewal and differentiation in HSCs is essential for advancing regenerative medicine and treating blood disorders. At compare.edu.vn, we provide comprehensive comparisons and insights to help you make informed decisions. Explore our resources today to delve deeper into this fascinating field.