Are you trying to understand the difference between GMI and A1C for better diabetes management? At COMPARE.EDU.VN, we provide a clear comparison of Glucose Management Indicator (GMI) and A1C, helping you make informed decisions about your health. Discover their calculations, interpretations, and practical applications.
1. What Is A1C and How Is It Used?
A1C is a blood test that measures your average blood sugar levels over the past 2-3 months. It stands for Glycated Hemoglobin, indicating the percentage of your red blood cells that have glucose attached to them. The higher your A1C level, the higher your average blood sugar levels have been.
A1C is a crucial tool for:
- Diagnosing diabetes: An A1C of 6.5% or higher indicates diabetes.
- Monitoring diabetes management: A1C levels show how well your treatment plan is working over time.
- Assessing the risk of diabetes complications: High A1C levels are associated with an increased risk of long-term complications such as heart disease, kidney disease, and nerve damage.
1.1. Target A1C Levels
Target A1C levels vary depending on individual factors such as age, overall health, and the presence of other medical conditions. However, for most adults with diabetes, the American Diabetes Association recommends an A1C goal of less than 7%.
1.2. Factors Affecting A1C Accuracy
Several factors can affect the accuracy of A1C tests, including:
- Anemia: Conditions that affect red blood cell production can alter A1C levels.
- Hemoglobinopathies: Variations in hemoglobin structure can interfere with A1C measurements.
- Pregnancy: A1C levels may be lower during pregnancy due to increased red blood cell turnover.
- Kidney disease: Kidney disease can affect red blood cell lifespan and alter A1C results.
2. What Is GMI and How Is It Calculated?
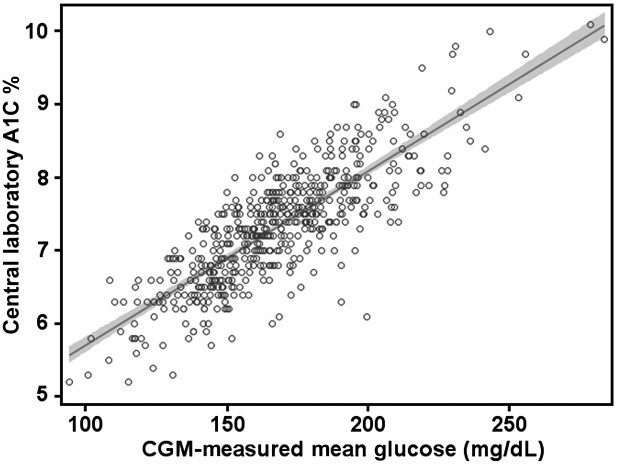
GMI stands for Glucose Management Indicator. It’s an estimate of your A1C level based on continuous glucose monitoring (CGM) data, providing a real-time view of your glucose trends. GMI is calculated using a formula that converts average glucose levels from CGM readings into an estimated A1C percentage.
2.1. GMI Calculation Formula
The formula to calculate GMI is:
- GMI (%) = 3.31 + 0.02392 × [mean glucose in mg/dL]
For mean glucose expressed in mmol/L, the formula is:
- GMI (mmol/mol) = 12.71 + 4.70587 × [mean glucose in mmol/L]
This calculation is based on extensive clinical trials and provides a reliable estimate of A1C levels based on CGM data.
 GMI Calculation
GMI Calculation
2.2. The Importance of CGM Data
CGM provides a comprehensive view of glucose levels throughout the day and night, capturing fluctuations that A1C tests may miss. Using at least 10-14 days of CGM data ensures a more accurate GMI calculation.
2.3. Where to Find a GMI Calculator
You can find a GMI calculator at www.jaeb.org/gmi and www.AGPreport.org/agp/links. These tools make it easy to convert your average glucose levels into a GMI value.
3. Key Differences Between GMI and A1C
Understanding the differences between GMI and A1C is crucial for effective diabetes management. Here’s a detailed comparison:
| Feature | A1C | GMI |
|---|---|---|
| Measurement Type | Blood test | Calculated from CGM data |
| Time Frame | 2-3 months average | 10-14 days of CGM data |
| Information Provided | Overall average glucose level | Estimated A1C based on real-time glucose trends |
| Frequency of Testing | Typically every 3-6 months | Continuous monitoring |
| Accuracy Factors | Affected by anemia, hemoglobinopathies, etc. | Dependent on CGM accuracy and data completeness |
| Clinical Use | Diagnosis, long-term monitoring | Real-time management, pattern identification, therapy adjustments |
3.1. Time Frame and Data Collection
A1C provides a retrospective view of average glucose levels over 2-3 months, while GMI offers a more immediate estimate based on recent CGM data.
3.2. Clinical Applications
A1C is primarily used for diagnosis and long-term monitoring, while GMI is valuable for making real-time adjustments to diabetes management plans.
3.3. Accuracy and Influencing Factors
A1C accuracy can be affected by various medical conditions, whereas GMI accuracy depends on the reliability and completeness of CGM data.
4. Why the Change from eA1C to GMI Was Necessary
The shift from “estimated A1C” (eA1C) to “Glucose Management Indicator” (GMI) was driven by the need to reduce confusion among patients and clinicians. The term eA1C implied a direct correlation with lab-measured A1C, which wasn’t always the case.
4.1. Avoiding Misinterpretation
The term “estimated” suggested a precise match with lab-measured A1C, leading to frustration when discrepancies occurred.
4.2. Conveying a Clearer Message
GMI conveys that the metric is derived from glucose values and indicates the current state of a person’s glucose management, without implying a precise match with lab-measured A1C.
4.3. Positive Language
The term “management” was chosen over “control” to promote a more positive and empowering approach to diabetes care, as suggested by Dickinson et al. in “The Use of Language in Diabetes Care and Education.”
5. How to Explain GMI to Individuals with Diabetes
Explaining GMI in a clear and understandable way is crucial for patient engagement and effective diabetes management.
5.1. Key Points to Communicate
- GMI is an estimate of what your A1C is likely to be, based on your average glucose levels from CGM readings.
- Your lab-measured A1C might be similar, higher, or lower than your GMI.
- GMI is calculated from your average CGM glucose, which measures glucose in interstitial fluid every 1-5 minutes.
- Lab-measured A1C reflects how much glucose has attached to the hemoglobin in your red blood cells over approximately 120 days.
5.2. Understanding Discrepancies
Explain that differences between lab-measured A1C and GMI can occur due to various factors, including the lifespan of red blood cells and conditions affecting glucose attachment to red blood cells.
5.3. Table 2: Explaining GMI to Individuals with Diabetes
| GMI tells you what your approximate A1C level is likely to be, based on the average glucose level from your CGM readings for 14 or more days. |
|---|
| – • GMI gives you the A1C level that would usually be expected from a large number of individuals with diabetes who have the same average CGM glucose level as you. – • However, your laboratory A1C might be similar to, higher than, or lower than your GMI. ○ Your GMI is calculated from your average CGM glucose, which measures glucose in interstitial fluid (under the skin) every 1–5 min. – ○ Laboratory A1C is a measure of how much glucose has attached to the hemoglobin in your red blood cells over the life of each red blood cell, ∼120 days. – ○ Each person’s red blood cells may live for a slightly different number of days, and there may be differences in factors that affect how glucose attaches to your red blood cells. Therefore, we do not expect people with the same average glucose or calculated GMI to have the exact same laboratory A1C value. – ○ There also are certain medical conditions that affect the life span of red blood cells that may explain differences between the GMI and laboratory A1C, including hemoglobinopathies and hemolytic anemia. |
| Here is what having a difference in laboratory-measured A1C and GMI may mean: |
| Laboratory A1C vs. GMI |
| 8.0% vs. 7.8% |
| 8.0% vs. 7.2% |
| 7.2% vs. 8.0% |
5.4. When GMI and A1C Might Not Agree
Explain scenarios where GMI and lab-measured A1C might differ, such as during short periods of acute hyperglycemia or significant changes in diet and exercise.
6. Using GMI to Inform Glucose Management Targets
GMI can be a valuable tool in setting personalized glucose management targets.
6.1. Setting Individualized A1C Goals
If a person’s GMI is consistently lower than their lab-measured A1C, it’s important to avoid setting the therapeutic goal too low to prevent hypoglycemia.
6.2. Adjusting Therapy Based on GMI
Conversely, if a person’s GMI is consistently higher than their lab-measured A1C, it might be safe to set the A1C target slightly lower to minimize excessive hyperglycemia.
6.3. Table 3: Difference Between GMI and Laboratory-Measured A1C
| Absolute value of difference between GMI and laboratory A1C (%) | Percentage of values (%) | 95% CI (%) |
|---|---|---|
| 0 to | 19 | 16–22 |
| ≥0.1 | 81 | 78–84 |
| ≥0.2 | 67 | 63–71 |
| ≥0.3 | 51 | 47–55 |
| ≥0.4 | 39 | 34–43 |
| ≥0.5 | 28 | 24–32 |
| ≥0.6 | 19 | 15–22 |
| ≥0.7 | 12 | 9–15 |
| ≥0.8 | 8 | 5–10 |
| ≥0.9 | 4 | 3–6 |
| ≥1.0 | 3 | 2–4 |
7. The Importance of Using Both A1C and CGM in Diabetes Management
Both lab-measured A1C and CGM-derived glucose data play unique roles in informing a glucose management plan.
7.1. Individualized A1C Targets
A1C targets should be tailored based on patient characteristics, engagement in self-management, and glucose monitoring data, including GMI.
7.2. Real-Time and Retrospective Data
CGM provides real-time glucose data and retrospective patterns, offering additional insights for medication and lifestyle adjustments.
7.3. Core Glucose Metrics
CGM metrics such as average glucose, GMI, time in range, time in hypoglycemia, and glycemic variability provide a comprehensive view of glucose management.
8. Clinical Scenarios: GMI vs A1C
Understanding how to interpret GMI and A1C in different clinical scenarios is essential for personalized diabetes care.
8.1. Acute Hyperglycemia
During short periods of acute hyperglycemia (illness, steroid administration), GMI will likely be higher than lab-measured A1C.
8.2. Short Periods of Lower Glucose Readings
Conversely, GMI may be lower than lab-measured A1C if there are short periods of significantly lower glucose readings (new diet, exercise regimen).
8.3. Stable Glucose Levels
Most of the time, when there are no acute or dramatic changes in glucose levels, the difference between GMI and A1C can help refine and personalize glucose management plans.
9. The Future of Diabetes Management: CGM and GMI
As CGM technology continues to advance, GMI and other CGM metrics are likely to play an increasingly important role in diabetes management.
9.1. Potential for Routine Use
The day may come when CGM is routinely used in conjunction with A1C or even in place of A1C, with CGM metrics becoming key indicators of quality diabetes care.
9.2. Connecting CGM Metrics to A1C
Changing the name from eA1C to GMI provides a useful measure for connecting CGM metrics to lab-measured A1C, reinforcing the need for ongoing management and engagement.
9.3. Global Adoption
The hope is that the term GMI and its calculation will be adopted by the global diabetes community, standardizing diabetes management practices.
10. FAQs About GMI and A1C
Here are some frequently asked questions to help you better understand GMI and A1C:
10.1. What is the normal range for A1C?
For most adults with diabetes, the recommended A1C target is less than 7%.
10.2. How often should I get an A1C test?
Typically, A1C tests are performed every 3-6 months, depending on your diabetes management plan.
10.3. Can GMI replace A1C testing?
While GMI provides valuable insights, A1C testing remains a standard diagnostic and monitoring tool.
10.4. What factors can affect A1C accuracy?
Factors such as anemia, hemoglobinopathies, pregnancy, and kidney disease can affect A1C accuracy.
10.5. How is GMI calculated?
GMI is calculated using a formula that converts average glucose levels from CGM readings into an estimated A1C percentage.
10.6. What does GMI tell me about my glucose management?
GMI provides an estimate of your A1C based on recent CGM data, helping you understand your glucose trends.
10.7. Why is my GMI different from my A1C?
Differences can occur due to factors such as the lifespan of red blood cells and short-term fluctuations in glucose levels.
10.8. How can I use GMI to improve my diabetes management?
GMI can help you set personalized glucose targets and make real-time adjustments to your therapy.
10.9. Where can I find a GMI calculator?
You can find a GMI calculator at www.jaeb.org/gmi and www.AGPreport.org/agp/links.
10.10. Who should I talk to about my GMI and A1C results?
Discuss your GMI and A1C results with your healthcare team to develop a personalized diabetes management plan.
11. Practical Advice for Managing Glucose Levels
Managing glucose levels effectively involves a combination of lifestyle adjustments and medical interventions.
11.1. Lifestyle Changes
- Diet: Focus on a balanced diet with controlled carbohydrate intake.
- Exercise: Regular physical activity can improve insulin sensitivity and lower blood sugar levels.
- Stress Management: High stress levels can impact glucose levels; practice relaxation techniques.
11.2. Medical Interventions
- Medication: Follow your healthcare provider’s instructions regarding medication.
- Monitoring: Regularly monitor your glucose levels using a CGM or blood glucose meter.
- Consultations: Regular check-ups with your healthcare team are crucial for adjusting your management plan.
12. Real-World Examples
Understanding how GMI and A1C work in real-world scenarios can provide valuable insights.
12.1. Case Study 1: Newly Diagnosed Patient
A newly diagnosed patient starts using CGM and discovers a GMI of 7.5%. Their initial A1C test comes back at 7.2%. The healthcare team uses this information to fine-tune their diet and exercise plan, aiming for a lower GMI to reduce the risk of complications.
12.2. Case Study 2: Long-Term Diabetes Management
A patient with long-term diabetes consistently sees a GMI that is 0.5% higher than their A1C. After discussing this with their doctor, they adjust their insulin dosage slightly to better match their CGM trends and achieve more stable glucose levels.
13. Expert Opinions and Recommendations
Experts in the field emphasize the importance of using both A1C and GMI for comprehensive diabetes management.
13.1. Endocrine Society Recommendations
The Endocrine Society recommends using CGM data, including GMI, to inform real-time therapy adjustments and personalize A1C targets.
13.2. American Diabetes Association Guidelines
The American Diabetes Association highlights the value of CGM in improving time in range and reducing hypoglycemia, complementing A1C testing.
14. Tools and Resources for Diabetes Management
Utilize these tools and resources to enhance your diabetes management:
- CGM Systems: Continuous Glucose Monitoring systems for real-time glucose data.
- Blood Glucose Meters: Traditional meters for spot-checking glucose levels.
- Diabetes Apps: Mobile apps for tracking glucose, diet, and exercise.
- Educational Websites: Reliable websites like the American Diabetes Association and COMPARE.EDU.VN for information and support.
15. Testimonials
Hear from individuals who have benefited from using GMI in their diabetes management:
15.1. Patient A
“Using GMI has helped me understand my glucose trends better. I can now see how my diet and exercise affect my levels in real-time, which has made a big difference.”
15.2. Patient B
“I was confused about the difference between GMI and A1C, but my doctor explained it clearly. Now, I feel more in control of my diabetes.”
16. Call to Action: Optimize Your Diabetes Management with COMPARE.EDU.VN
Ready to take control of your diabetes management? Understanding the nuances between GMI and A1C is essential for achieving your health goals. At COMPARE.EDU.VN, we provide the tools and resources you need to make informed decisions and optimize your care plan.
16.1. Explore COMPARE.EDU.VN
Visit COMPARE.EDU.VN to find detailed comparisons, expert advice, and practical tips for managing your diabetes effectively.
16.2. Contact Us
For personalized support and guidance, reach out to us:
- Address: 333 Comparison Plaza, Choice City, CA 90210, United States
- WhatsApp: +1 (626) 555-9090
- Website: COMPARE.EDU.VN
Don’t wait—start your journey to better diabetes management today with COMPARE.EDU.VN!
17. Staying Updated with Diabetes Management Advances
Keeping up-to-date with the latest advancements in diabetes management is crucial for providing the best possible care.
17.1. Emerging Technologies
Stay informed about new technologies such as advanced CGM systems, automated insulin delivery devices, and novel glucose-monitoring techniques.
17.2. Clinical Trials and Research
Follow clinical trials and research studies to understand the efficacy and safety of new treatments and management strategies.
17.3. Professional Organizations
Engage with professional organizations such as the American Diabetes Association and the Endocrine Society to stay informed about the latest guidelines and recommendations.
18. Additional Resources
Explore these additional resources for more information on GMI, A1C, and diabetes management:
- American Diabetes Association (ADA): Offers comprehensive information, resources, and support for individuals with diabetes and healthcare professionals.
- Endocrine Society: Provides clinical practice guidelines and educational resources for endocrinologists and other healthcare providers.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Conducts research and provides information on diabetes and related conditions.
19. Final Thoughts: Empowering Your Diabetes Journey
Understanding the relationship between GMI and A1C is a key step in empowering your diabetes journey. By leveraging the insights provided by these metrics and the resources available at compare.edu.vn, you can take control of your health and live a fulfilling life.
Remember, effective diabetes management is a collaborative effort between you and your healthcare team. Stay informed, stay engaged, and prioritize your well-being.