Uncover accurate insights into COVID-19 mortality rates among vaccinated and unvaccinated individuals at COMPARE.EDU.VN. We provide a detailed analysis, addressing the base rate fallacy and offering clear comparisons. Explore incidence rates and mortality ratios to understand the impact of vaccination, including booster shots, on reducing COVID-19 death rates, providing the insight you need to make well-informed decisions.
1. What Factors Influence COVID-19 Death Rates in Vaccinated and Unvaccinated People?
Several factors influence COVID-19 death rates in both vaccinated and unvaccinated individuals, including vaccination status, age, and the prevalence of underlying health conditions. According to data from the U.S. Centers for Disease Control and Prevention (CDC), unvaccinated individuals face a significantly higher risk of COVID-19-associated deaths compared to those who are vaccinated. This risk is further mitigated by receiving booster doses. Understanding these factors is crucial for assessing the effectiveness of vaccination in reducing mortality.
1.1 How Does Vaccination Status Affect COVID-19 Death Rates?
Vaccination status is a primary factor affecting COVID-19 death rates, with unvaccinated individuals experiencing substantially higher mortality rates. The CDC’s data from geographically representative state and local health departments indicates that unvaccinated individuals have a significantly greater risk of dying from COVID-19 compared to vaccinated individuals. This discrepancy underscores the protective effect of vaccines.
1.2 How Does Age Impact COVID-19 Mortality Rates?
Age plays a significant role in COVID-19 mortality rates, with older adults being more vulnerable to severe outcomes. According to the CDC, the risk of severe COVID-19 increases with age due to the weakening of the immune system. Consequently, older individuals are both more likely to be vaccinated and more likely to die from COVID-19, making it essential to consider age-specific data when comparing death rates.
1.3 How Do Underlying Health Conditions Influence COVID-19 Outcomes?
Underlying health conditions significantly influence COVID-19 outcomes, increasing the risk of severe illness and death. Individuals with chronic diseases such as diabetes, heart disease, and respiratory conditions are more likely to experience complications from COVID-19. Therefore, it is important to consider the prevalence of these conditions when comparing COVID-19 death rates across different populations.
2. Why Is It Important to Consider Base Rates When Comparing COVID-19 Deaths?
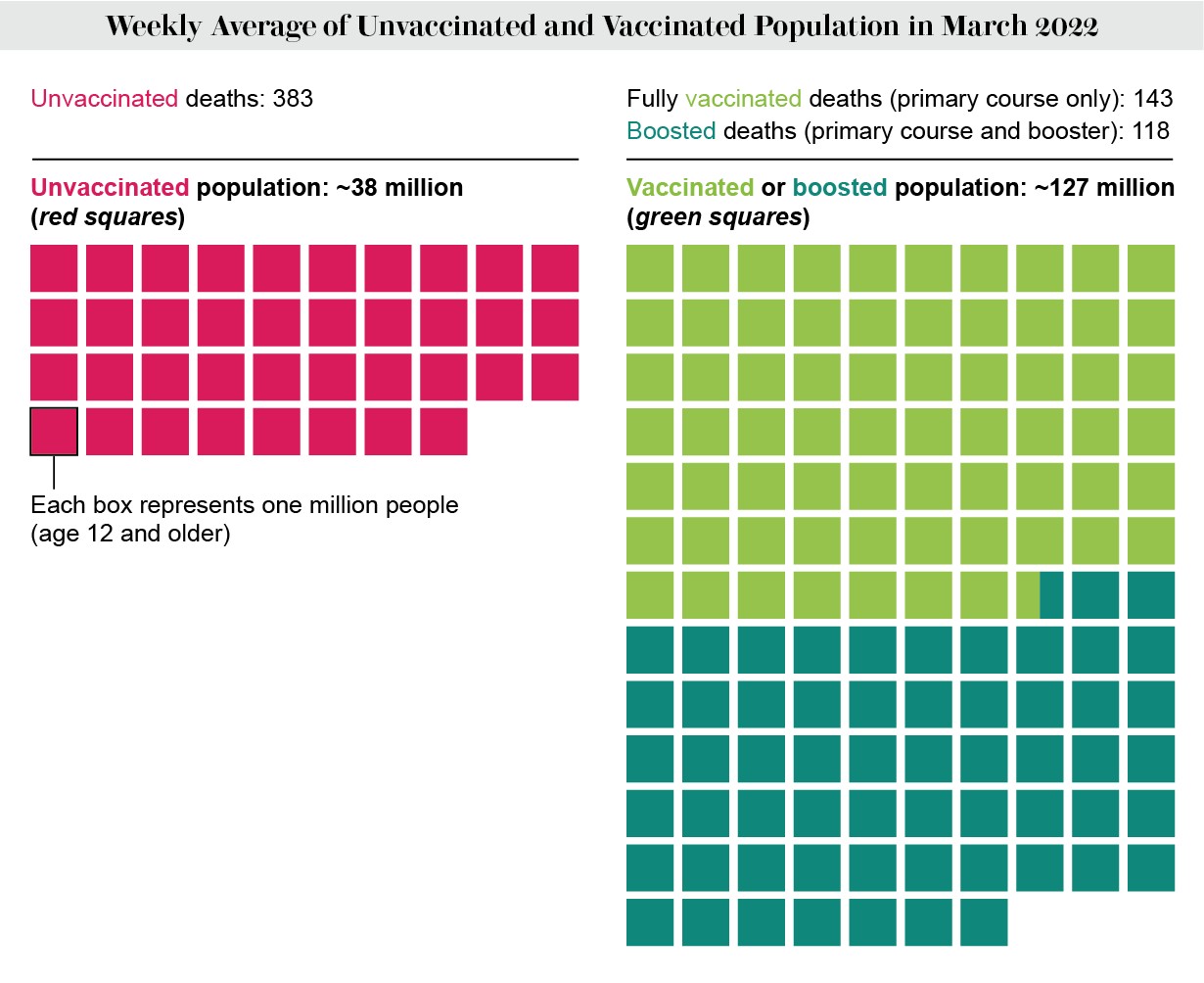
Considering base rates is crucial when comparing COVID-19 deaths to avoid the base rate fallacy, which can lead to misinterpretations of the data. The base rate fallacy occurs when the size of the vaccinated and unvaccinated populations is not taken into account. Given that the majority of the U.S. population has been vaccinated, even a small fraction of vaccinated individuals dying from COVID-19 can result in a significant number of deaths.
2.1 What Is the Base Rate Fallacy in COVID-19 Data Analysis?
The base rate fallacy in COVID-19 data analysis involves neglecting the underlying proportions of vaccinated and unvaccinated individuals when interpreting death statistics. For example, if a significant proportion of COVID-19 deaths occur in vaccinated individuals, it might seem that vaccines are ineffective. However, this conclusion ignores the fact that the vaccinated population is much larger than the unvaccinated population.
2.2 How Does Population Size Affect the Interpretation of COVID-19 Death Statistics?
Population size significantly affects the interpretation of COVID-19 death statistics. If a larger proportion of the population is vaccinated, even a small death rate among vaccinated individuals can result in a considerable number of deaths. Conversely, a higher death rate among unvaccinated individuals might not translate into a large number of deaths if the unvaccinated population is small. Therefore, it is essential to consider population sizes to draw accurate conclusions about vaccine effectiveness.
2.3 What Is the Role of Incidence Rates in COVID-19 Death Comparisons?
Incidence rates, expressed as the number of deaths per 100,000 people, play a crucial role in providing a standardized comparison of COVID-19 death rates. By standardizing the denominator across all groups, incidence rates offer a more accurate picture of the relative risk of death for vaccinated and unvaccinated individuals, mitigating the impact of varying population sizes.
3. How Do Incidence Rates Reveal the Impact of Vaccination on COVID-19 Deaths?
Incidence rates reveal the true impact of vaccination on COVID-19 deaths by providing a standardized measure that accounts for the different sizes of vaccinated and unvaccinated populations. By expressing deaths per 100,000 people, incidence rates offer a clear comparison of the risk of death in each group. This standardization helps to overcome the distortions caused by the base rate fallacy and provides a more accurate understanding of vaccine effectiveness.
3.1 What Do Incidence Rates Show About the Risk of Death for Unvaccinated People?
Incidence rates consistently demonstrate that unvaccinated individuals face a significantly higher risk of death from COVID-19 compared to vaccinated individuals. According to the CDC, unvaccinated people 12 years and older had 17 times the rate of COVID-associated deaths compared to people vaccinated with a primary series and a booster dose in March. This stark difference highlights the protective benefit of vaccination.
3.2 How Do Boosters Affect COVID-19 Death Rates According to Incidence Rates?
Boosters significantly reduce COVID-19 death rates, as evidenced by incidence rate comparisons. The CDC data indicates that individuals who received a primary vaccine series and a booster dose had substantially lower death rates compared to those who only had a primary series or were unvaccinated. This suggests that booster shots enhance immune protection and further reduce the risk of severe outcomes.
3.3 How Do Age-Specific Incidence Rates Help Understand COVID-19 Mortality?
Age-specific incidence rates provide a more nuanced understanding of COVID-19 mortality by accounting for the varying risk profiles of different age groups. Older adults, who are more likely to be vaccinated and more vulnerable to severe COVID-19, benefit significantly from vaccination and booster doses. Analyzing incidence rates within specific age groups clarifies the protective effect of vaccines across different demographics.
4. How Do Ratios of Death Rates Among Vaccinated and Unvaccinated People Provide Insight?
Comparing the ratios of death rates among vaccinated and unvaccinated individuals provides valuable insight into the protective effect of vaccination. These ratios quantify the relative risk of death for unvaccinated individuals compared to their vaccinated counterparts, offering a straightforward measure of vaccine effectiveness. By examining these ratios, public health officials and the public can better understand the benefits of vaccination in reducing mortality.
4.1 What Is the Ratio of COVID-19 Death Rates for Unvaccinated Vs. Vaccinated People?
The ratio of COVID-19 death rates for unvaccinated versus vaccinated people consistently shows a significant disparity. For example, in March, unvaccinated people 12 years and older had 17 times the rate of COVID-associated deaths compared to people vaccinated with a primary series and a booster dose. This ratio highlights the substantial protective effect of vaccination against severe outcomes.
4.2 How Do Boosters Influence the Ratio of Death Rates?
Boosters significantly influence the ratio of death rates, further reducing the risk for vaccinated individuals. The CDC data indicates that unvaccinated individuals had eight times the rate of death as compared to people who only had a primary series, suggesting that boosters increase the level of protection. This underscores the importance of booster doses in maintaining robust immunity.
4.3 Why Is Comparing Ratios More Informative Than Absolute Numbers?
Comparing ratios is more informative than absolute numbers because it accounts for the differing sizes of the vaccinated and unvaccinated populations. Absolute numbers can be misleading if a large proportion of the population is vaccinated, as even a small death rate among vaccinated individuals can result in a significant number of deaths. Ratios provide a standardized measure that reflects the true relative risk.
5. How Does Age Affect the Protection Offered by COVID-19 Vaccines?
Age significantly affects the protection offered by COVID-19 vaccines, with older adults experiencing both a higher risk of severe outcomes and a potentially weaker immune response to vaccination. As the immune system weakens with age, older individuals may not mount as strong an immune response to the primary vaccine series, making booster doses particularly important for this demographic. Understanding these age-related factors is crucial for tailoring vaccination strategies.
5.1 Why Are Older People More Likely to Be Vaccinated and Die of COVID-19?
Older people are more likely to be vaccinated because they are at higher risk of severe COVID-19 outcomes. However, they are also more likely to die of COVID-19 due to the weakening of the immune system with age. This combination of factors underscores the importance of vaccination and booster doses for older adults in reducing their risk of mortality.
5.2 How Does Immune Protection from Vaccination Wane with Time, Especially in Older Adults?
Immune protection from vaccination wanes with time, especially in older adults, who may not maintain a robust immune response from the primary series alone. This waning immunity increases the risk of breakthrough infections and severe outcomes, highlighting the need for booster doses to maintain protection. Regular boosters can help older adults maintain a higher level of immunity and reduce their risk of hospitalization and death.
5.3 How Do Booster Doses Enhance Protection for Different Age Groups?
Booster doses enhance protection for all age groups, but they are particularly crucial for older adults. Boosters help to restore waning immunity and provide additional protection against emerging variants. By increasing antibody levels and enhancing immune responses, booster doses reduce the risk of severe COVID-19 outcomes across different age demographics.
6. What Role Does the Shrinking Unvaccinated Population Play in Death Statistics?
The shrinking unvaccinated population plays a significant role in death statistics, as the proportion of unvaccinated individuals decreases due to both vaccination efforts and the disproportionate number of COVID-19 deaths among the unvaccinated. This leaves a comparatively larger vaccinated group, leading to an increase in total deaths among vaccinated individuals, even though the death rate is lower. This phenomenon further underscores the importance of considering population sizes when interpreting death statistics.
6.1 How Does the Unvaccinated Population Shrink Over Time?
The unvaccinated population shrinks over time due to two main factors: increasing vaccination rates and the disproportionate number of COVID-19 deaths among the unvaccinated. As more people get vaccinated, the unvaccinated population decreases. Additionally, because unvaccinated individuals are at a higher risk of severe COVID-19 outcomes, a larger proportion of them die from the virus, further reducing the size of the unvaccinated population.
6.2 Why Might Total Deaths Increase in Vaccinated Groups Despite Lower Death Rates?
Total deaths might increase in vaccinated groups despite lower death rates because the vaccinated population is much larger than the unvaccinated population. Even if the death rate among vaccinated individuals is low, the sheer size of the vaccinated population means that a significant number of deaths can still occur. This is a key factor in understanding why absolute numbers can be misleading.
6.3 What Does This Trend Imply About Vaccine Effectiveness?
This trend does not imply that vaccines are ineffective. On the contrary, it highlights the importance of vaccination in reducing the overall risk of severe outcomes. While no vaccine is 100 percent effective, immunization substantially reduces the risk of dying from COVID-19. The increase in total deaths among vaccinated individuals is primarily a result of the larger vaccinated population size, not a failure of the vaccines.
7. What Are the Limitations of Using Absolute Numbers to Compare COVID-19 Deaths?
Using absolute numbers to compare COVID-19 deaths has several limitations, primarily because it fails to account for the varying sizes of vaccinated and unvaccinated populations. Absolute numbers can be misleading, especially when a large proportion of the population is vaccinated, as even a small death rate among vaccinated individuals can result in a significant number of deaths. To accurately assess vaccine effectiveness, it is essential to use standardized measures such as incidence rates and ratios.
7.1 How Can Absolute Numbers Mislead Public Perception of Vaccine Effectiveness?
Absolute numbers can mislead public perception of vaccine effectiveness by suggesting that vaccines are ineffective if a significant proportion of COVID-19 deaths occur in vaccinated individuals. This misinterpretation arises because absolute numbers do not account for the fact that the vaccinated population is much larger than the unvaccinated population. To avoid this fallacy, it is crucial to consider relative measures that account for population sizes.
7.2 What Alternative Metrics Provide a More Accurate Comparison?
Alternative metrics that provide a more accurate comparison include incidence rates, ratios of death rates, and age-specific analyses. Incidence rates standardize the denominator across all groups, allowing for a direct comparison of risk. Ratios of death rates quantify the relative risk for unvaccinated individuals compared to vaccinated individuals. Age-specific analyses account for the varying risk profiles of different age groups, providing a more nuanced understanding of vaccine effectiveness.
7.3 Why Is Context Important When Interpreting COVID-19 Death Statistics?
Context is crucial when interpreting COVID-19 death statistics because it involves considering various factors such as vaccination rates, population sizes, age demographics, and the prevalence of underlying health conditions. Without this context, it is easy to draw incorrect conclusions about vaccine effectiveness and the overall impact of the pandemic. A comprehensive understanding of these factors is essential for making informed decisions.
8. How Do COVID-19 Variants Affect Death Rates in Vaccinated and Unvaccinated People?
COVID-19 variants can affect death rates in both vaccinated and unvaccinated people, with some variants being more virulent and capable of causing severe illness. While vaccines have generally been effective against most variants, their effectiveness can vary depending on the specific variant and an individual’s immune status. Monitoring the impact of variants on death rates is essential for adjusting vaccination strategies and public health measures.
8.1 How Do Variants Influence the Severity of COVID-19 Infections?
Variants influence the severity of COVID-19 infections by exhibiting different levels of transmissibility and virulence. Some variants, such as Delta, have been associated with more severe illness and higher hospitalization rates compared to the original strain. Understanding the characteristics of each variant is crucial for assessing its potential impact on death rates and overall public health.
8.2 Do Vaccines Offer the Same Protection Against All Variants?
Vaccines do not offer the same level of protection against all variants, although they generally provide significant protection against severe outcomes. The effectiveness of vaccines can vary depending on the specific variant and the individual’s immune response. Booster doses have been shown to enhance protection against emerging variants, underscoring their importance in maintaining immunity.
8.3 How Can Public Health Measures Adapt to Emerging Variants?
Public health measures can adapt to emerging variants by monitoring their spread, assessing their impact on disease severity, and adjusting vaccination strategies accordingly. This includes developing and deploying variant-specific vaccines, recommending booster doses, and implementing non-pharmaceutical interventions such as mask-wearing and social distancing. A flexible and adaptive approach is essential for mitigating the impact of new variants.
9. What Long-Term Trends Can Be Observed in COVID-19 Death Data?
Long-term trends in COVID-19 death data reveal a decline in mortality rates over time, largely due to increasing vaccination rates, improved treatments, and a better understanding of the virus. However, periodic surges driven by new variants can disrupt this trend, highlighting the ongoing need for vigilance and adaptive public health measures. Monitoring these trends is crucial for predicting future outbreaks and preparing for potential challenges.
9.1 How Have Death Rates Changed Since the Beginning of the Pandemic?
Death rates have generally decreased since the beginning of the pandemic, thanks to widespread vaccination campaigns and advancements in medical treatments. Initially, the lack of effective treatments and limited vaccine availability resulted in higher mortality rates. Over time, as vaccination rates increased and treatments improved, death rates declined significantly.
9.2 What Role Do Improved Treatments Play in Reducing Mortality?
Improved treatments play a crucial role in reducing mortality by mitigating the severity of COVID-19 infections and preventing complications. Antiviral medications, monoclonal antibodies, and supportive care measures have all contributed to reducing the risk of severe outcomes and death. Continued research and development of new treatments are essential for further improving patient outcomes.
9.3 How Do Seasonal Patterns Affect COVID-19 Death Rates?
Seasonal patterns can affect COVID-19 death rates, with some studies suggesting that respiratory virus infections tend to increase during the colder months. This may be due to factors such as increased indoor gatherings and reduced humidity, which can facilitate virus transmission. Understanding these seasonal patterns can help inform public health recommendations and vaccination strategies.
10. What Are Some Common Misconceptions About COVID-19 Death Statistics?
Several common misconceptions about COVID-19 death statistics can lead to misunderstandings and misinterpretations of the data. These misconceptions include the belief that vaccines are ineffective if vaccinated individuals die from COVID-19, the neglect of base rates when comparing death rates, and the failure to account for the impact of age and underlying health conditions. Addressing these misconceptions is essential for promoting informed decision-making and building public trust.
10.1 Why Is It Incorrect to Assume Vaccines Are Ineffective If Vaccinated People Die?
It is incorrect to assume that vaccines are ineffective if vaccinated people die because vaccines are not 100 percent effective at preventing infection or death. However, they significantly reduce the risk of severe outcomes and death. The fact that some vaccinated individuals die from COVID-19 does not negate the overall protective benefit of vaccination.
10.2 How Can Misleading Statistics Impact Public Health Efforts?
Misleading statistics can negatively impact public health efforts by undermining public trust, promoting vaccine hesitancy, and hindering the implementation of effective public health measures. When the public is misinformed about the true risks and benefits of vaccination, they may be less likely to get vaccinated or follow public health recommendations, which can prolong the pandemic and increase morbidity and mortality.
10.3 What Strategies Can Help the Public Interpret COVID-19 Data More Accurately?
Several strategies can help the public interpret COVID-19 data more accurately, including using standardized metrics such as incidence rates and ratios, considering base rates and population sizes, and consulting reliable sources of information such as the CDC and WHO. Educating the public about these strategies can promote a more informed and evidence-based understanding of the pandemic.
COMPARE.EDU.VN: Your Trusted Source for Clear COVID-19 Data Analysis
Navigating the complexities of COVID-19 data can be challenging. At COMPARE.EDU.VN, we simplify the process by providing clear, objective comparisons of mortality rates among vaccinated and unvaccinated individuals. Our detailed analyses account for critical factors like age, population size, and vaccine status, giving you the insight you need to make informed decisions. Visit COMPARE.EDU.VN today to explore our comprehensive comparisons and stay ahead with reliable information. Our team of experts utilizes the latest data from reputable sources like the CDC to offer analyses that cut through the noise.
Ready to Make Informed Choices?
Don’t let confusing statistics cloud your judgment. Visit COMPARE.EDU.VN now and discover the clarity you need to understand COVID-19 data and make informed decisions.
Contact Us:
- Address: 333 Comparison Plaza, Choice City, CA 90210, United States
- WhatsApp: +1 (626) 555-9090
- Website: compare.edu.vn
FAQ: Comparing COVID-19 Death Rates
1. How are COVID-19 death rates calculated for vaccinated and unvaccinated people?
COVID-19 death rates are calculated by dividing the number of COVID-19 deaths in each group (vaccinated and unvaccinated) by the respective population size, often expressed as deaths per 100,000 people.
2. What is the base rate fallacy, and how does it affect COVID-19 data interpretation?
The base rate fallacy is neglecting the underlying proportions of vaccinated and unvaccinated individuals, leading to misinterpretations of death statistics.
3. Why do incidence rates provide a more accurate comparison of COVID-19 deaths?
Incidence rates standardize the denominator across all groups, offering a clearer comparison of the risk of death by accounting for population sizes.
4. How do booster doses affect COVID-19 death rates compared to the primary vaccine series?
Booster doses enhance immune protection, resulting in substantially lower death rates compared to those who only had a primary series or were unvaccinated.
5. How does age influence the protection offered by COVID-19 vaccines?
Age affects vaccine protection, with older adults experiencing higher risk and potentially weaker immune responses, making booster doses particularly important.
6. Why might total deaths increase in vaccinated groups despite lower death rates?
Total deaths might increase in vaccinated groups because the vaccinated population is much larger, even if their death rate is lower.
7. What are the limitations of using absolute numbers to compare COVID-19 deaths?
Absolute numbers don’t account for varying population sizes, which can be misleading; relative measures like incidence rates provide a more accurate comparison.
8. How do COVID-19 variants affect death rates in vaccinated and unvaccinated individuals?
Variants can influence severity, but vaccines generally offer significant protection against severe outcomes, though effectiveness can vary.
9. What long-term trends can be observed in COVID-19 death data?
Long-term trends show declining mortality due to increasing vaccination and improved treatments, though surges from new variants can disrupt this.
10. What are some common misconceptions about COVID-19 death statistics?
Misconceptions include assuming vaccines are ineffective if vaccinated people die and neglecting base rates, impacting public health efforts.
 COVID death rates by vaccination status and age
COVID death rates by vaccination status and age
