How Much Worse Is Covid Compared To The Flu? COMPARE.EDU.VN provides a comprehensive comparison between COVID-19 and influenza, exploring their symptoms, severity, and impact to help you understand the differences. This comparison sheds light on the health risks, recovery timelines, and long-term effects of each illness.
Table of Contents
- Understanding COVID-19 and Flu: An Overview
- Transmission and Spread: How Contagious Are They?
- Symptom Comparison: Key Differences to Look For
- Severity and Complications: Who Is Most at Risk?
- Mortality Rates: A Critical Examination
- Long-Term Effects: What to Expect After Recovery
- Prevention and Vaccination: Staying Safe and Protected
- Treatment Options: What Works Best for Each Virus?
- Impact on Healthcare Systems: Strain and Resource Allocation
- Economic Consequences: Costs and Productivity Losses
- Public Health Measures: Effectiveness and Impact
- Psychological Effects: Mental Health and Well-being
- The Role of Variants: How They Change the Game
- Future Outlook: What’s Next for COVID-19 and Flu?
- Expert Opinions: Insights from Medical Professionals
- Personal Experiences: Stories from Those Affected
- COMPARE.EDU.VN: Your Resource for Informed Decisions
- Frequently Asked Questions (FAQ)
1. Understanding COVID-19 and Flu: An Overview
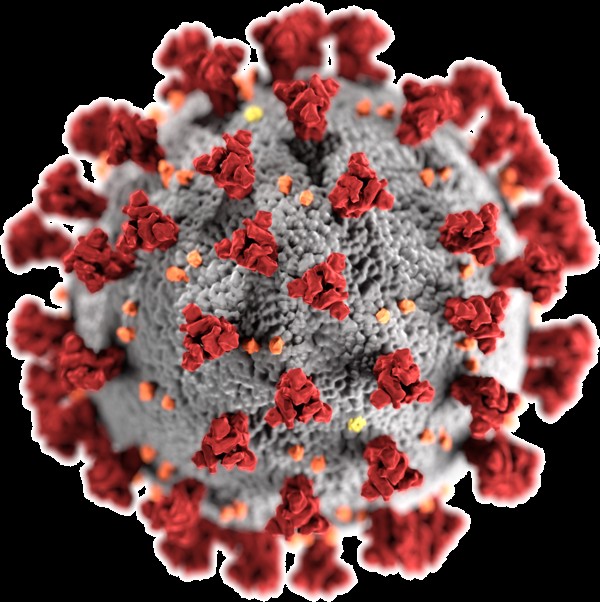
COVID-19, short for Coronavirus Disease 2019, is caused by the SARS-CoV-2 virus, a novel coronavirus that emerged in late 2019. The flu, or influenza, is caused by influenza viruses, which have been circulating for centuries. Both are respiratory illnesses, but they are caused by different viruses. Understanding these fundamental differences is crucial for assessing how much worse COVID-19 is compared to the flu.
COVID-19 has a broader range of symptoms and can lead to more severe complications than the flu. The SARS-CoV-2 virus can affect multiple organ systems, leading to long-term health issues. In contrast, influenza primarily targets the respiratory system.
Influenza viruses are categorized into types A, B, C, and D, with types A and B causing seasonal epidemics in humans. The flu virus is highly contagious and spreads through respiratory droplets produced when infected people cough, sneeze, or talk. Symptoms typically include fever, cough, sore throat, muscle aches, and fatigue.
While both illnesses share similar symptoms, COVID-19 has been associated with a higher risk of severe illness, hospitalization, and death, particularly in the early stages of the pandemic. Additionally, COVID-19 can lead to long-term complications, often referred to as “long COVID,” which can affect multiple organ systems and significantly impact quality of life.
2. Transmission and Spread: How Contagious Are They?
Both COVID-19 and the flu are transmitted through respiratory droplets produced when an infected person coughs, sneezes, or talks. However, the contagiousness, or R0 (basic reproduction number), differs between the two viruses. COVID-19, particularly in its early variants, had a higher R0 compared to the flu, meaning it spread more rapidly through populations.
The R0 of the original SARS-CoV-2 virus was estimated to be between 2 and 3, meaning each infected person could potentially infect 2 to 3 others in an unvaccinated population. The flu, on the other hand, typically has an R0 of around 1.3. This difference in contagiousness contributed to the rapid global spread of COVID-19.
Factors influencing transmission include viral load, duration of infectiousness, and the environment. COVID-19 has a longer incubation period (2-14 days) compared to the flu (1-4 days), which allows infected individuals to spread the virus for a longer period before showing symptoms. The Omicron variant of COVID-19 further increased its transmissibility, making it even more contagious than previous variants.
| Factor | COVID-19 | Flu |
|---|---|---|
| Transmission Route | Respiratory droplets | Respiratory droplets |
| R0 (Reproduction No.) | 2-3 (original), higher for variants | ~1.3 |
| Incubation Period | 2-14 days | 1-4 days |
| Infectious Period | Longer, even pre-symptomatic | Shorter, mostly symptomatic |






Public health measures, such as mask-wearing, social distancing, and hand hygiene, are effective in reducing the transmission of both viruses. However, the higher contagiousness of COVID-19 required more stringent measures to control its spread, especially during the initial phases of the pandemic.
3. Symptom Comparison: Key Differences to Look For
Both COVID-19 and the flu share several common symptoms, including fever, cough, sore throat, fatigue, and muscle aches. However, there are key differences that can help distinguish between the two illnesses. Loss of taste or smell (anosmia) is a hallmark symptom of COVID-19, which is less common in the flu. Shortness of breath and chest pain are also more frequently reported in COVID-19 cases.
| Symptom | COVID-19 | Flu |
|---|---|---|
| Fever | Common, can be high | Common, usually high |
| Cough | Common, can be dry or productive | Common, usually dry |
| Sore Throat | Common | Common |
| Fatigue | Common, often severe | Common |
| Muscle Aches | Common | Common |
| Loss of Taste/Smell | Common, distinctive symptom | Less common |
| Shortness of Breath | More common, can be severe | Less common |
| Chest Pain | More common | Less common |
| Headache | Common | Common |
| Nasal Congestion | Common | Common |
| Gastrointestinal Symptoms | Common (nausea, vomiting, diarrhea) | Less common, more typical in children |
Gastrointestinal symptoms, such as nausea, vomiting, and diarrhea, are more commonly reported in COVID-19 cases compared to the flu. While these symptoms can occur with the flu, they are more typical in children. The severity and duration of symptoms can also differ between the two illnesses. COVID-19 symptoms can persist for longer periods and may lead to long-term health issues.
It’s important to note that symptom presentation can vary depending on the individual, age, underlying health conditions, and the specific variant of the virus. Therefore, relying solely on symptoms to differentiate between COVID-19 and the flu is not always accurate. Diagnostic testing, such as PCR tests for COVID-19 and rapid antigen tests for both COVID-19 and the flu, is necessary for accurate diagnosis.
4. Severity and Complications: Who Is Most at Risk?
The severity of both COVID-19 and the flu can range from mild to severe, with some individuals experiencing asymptomatic infections. However, COVID-19 has been associated with a higher risk of severe complications, particularly in certain populations. Older adults, individuals with underlying health conditions (such as heart disease, diabetes, and chronic respiratory diseases), and those who are immunocompromised are at higher risk of severe outcomes from both COVID-19 and the flu.
Complications from COVID-19 can include pneumonia, acute respiratory distress syndrome (ARDS), blood clots, multisystem inflammatory syndrome in children (MIS-C), and long-term organ damage. The flu can also lead to pneumonia, bronchitis, sinus infections, and ear infections. However, the risk of ARDS and blood clots is generally higher with COVID-19.
Children under 5 years old are also at higher risk of complications from the flu. Pregnant women are at increased risk of severe illness from both COVID-19 and the flu, and vaccination is recommended to protect both the mother and the baby.
The emergence of COVID-19 variants has further complicated the assessment of severity. Some variants, such as Delta, were associated with increased severity and higher hospitalization rates. While the Omicron variant was generally considered less severe than Delta, its high transmissibility led to a surge in cases and hospitalizations, particularly among unvaccinated individuals.
5. Mortality Rates: A Critical Examination
Mortality rates are a critical measure for comparing the impact of COVID-19 and the flu. The case fatality rate (CFR), which is the proportion of confirmed cases that result in death, has been significantly higher for COVID-19 compared to the flu, especially during the early stages of the pandemic.
The CFR for COVID-19 has varied depending on factors such as age, underlying health conditions, access to healthcare, and the specific variant of the virus. Early estimates placed the CFR for COVID-19 at around 3-4%, while the CFR for seasonal influenza is typically below 0.1%. This means that COVID-19 was initially estimated to be 30 to 40 times more deadly than the flu.
| Measure | COVID-19 (Early Pandemic) | Flu (Seasonal) |
|---|---|---|
| Case Fatality Rate (CFR) | 3-4% | <0.1% |
| Infection Fatality Rate (IFR) | Lower than CFR, varies by age | Very low |
However, it’s important to consider the infection fatality rate (IFR), which accounts for all infections, including asymptomatic and undiagnosed cases. The IFR is generally lower than the CFR and provides a more accurate estimate of the overall mortality risk. The IFR for COVID-19 has also decreased over time due to increased vaccination rates, improved treatments, and the emergence of less severe variants.
Despite the decrease in CFR and IFR, COVID-19 has still resulted in a significantly higher number of deaths globally compared to seasonal influenza. The World Health Organization (WHO) estimates that COVID-19 has caused millions of deaths worldwide, while seasonal influenza typically causes hundreds of thousands of deaths each year.
6. Long-Term Effects: What to Expect After Recovery
One of the distinguishing features of COVID-19 compared to the flu is the potential for long-term health effects, often referred to as “long COVID” or post-COVID-19 condition. Long COVID is characterized by a wide range of persistent symptoms that can last for weeks or months after the initial infection.
Common symptoms of long COVID include fatigue, shortness of breath, cognitive dysfunction (“brain fog”), chest pain, joint pain, headache, and loss of taste or smell. These symptoms can significantly impact daily functioning and quality of life. Studies have shown that a substantial proportion of individuals who have had COVID-19, including those with mild cases, can experience long COVID.
The underlying mechanisms of long COVID are still being investigated, but potential factors include persistent viral reservoirs, immune dysregulation, and damage to the cardiovascular and nervous systems. Long COVID can affect multiple organ systems, including the lungs, heart, brain, and kidneys.
While the flu can also cause post-viral symptoms, such as fatigue and cough, these are generally less severe and shorter in duration compared to long COVID. The long-term effects of COVID-19 have placed a significant burden on healthcare systems and have highlighted the need for specialized clinics and rehabilitation programs for individuals with long COVID.
7. Prevention and Vaccination: Staying Safe and Protected
Vaccination is a key strategy for preventing both COVID-19 and the flu. Vaccines work by stimulating the immune system to produce antibodies that protect against the virus. Both COVID-19 and influenza vaccines have been shown to be safe and effective in reducing the risk of infection, severe illness, hospitalization, and death.
COVID-19 vaccines were developed and deployed at an unprecedented speed, and several types of vaccines are now available, including mRNA vaccines (Pfizer-BioNTech and Moderna), viral vector vaccines (Johnson & Johnson/Janssen and AstraZeneca), and protein subunit vaccines (Novavax). These vaccines have demonstrated high efficacy in clinical trials and real-world studies.
Influenza vaccines are updated annually to match the circulating strains of the flu virus. These vaccines are available in various formulations, including inactivated influenza vaccines (IIV), recombinant influenza vaccines (RIV), and live attenuated influenza vaccines (LAIV). The Centers for Disease Control and Prevention (CDC) recommends that everyone 6 months and older receive an annual flu vaccine.
In addition to vaccination, other preventive measures can help reduce the spread of both COVID-19 and the flu. These include:
- Wearing masks: Masks can help prevent the transmission of respiratory droplets.
- Social distancing: Maintaining physical distance from others can reduce the risk of infection.
- Hand hygiene: Frequent handwashing with soap and water or using hand sanitizer can kill viruses.
- Respiratory etiquette: Covering coughs and sneezes with a tissue or elbow can prevent the spread of droplets.
- Ventilation: Improving airflow in indoor spaces can reduce the concentration of airborne viruses.
8. Treatment Options: What Works Best for Each Virus?
Treatment options for COVID-19 and the flu vary depending on the severity of the illness and the individual’s risk factors. For mild to moderate cases, supportive care, such as rest, hydration, and over-the-counter medications to relieve symptoms, is often sufficient.
Antiviral medications are available for both COVID-19 and the flu. For COVID-19, antiviral medications such as Paxlovid (nirmatrelvir/ritonavir) and remdesivir can reduce the risk of hospitalization and death, particularly when administered early in the course of the illness. Monoclonal antibody treatments were also used during the pandemic, but their effectiveness has been limited against newer variants.
For the flu, antiviral medications such as oseltamivir (Tamiflu), zanamivir (Relenza), and baloxavir marboxil (Xofluza) can shorten the duration of symptoms and reduce the risk of complications, especially when started within 48 hours of symptom onset.
In severe cases of COVID-19, hospitalization may be required, and treatments such as oxygen therapy, mechanical ventilation, and corticosteroids may be necessary to support respiratory function and reduce inflammation. Patients with severe flu may also require hospitalization and similar supportive care.
| Treatment | COVID-19 | Flu |
|---|---|---|
| Supportive Care | Rest, hydration, over-the-counter medications | Rest, hydration, over-the-counter medications |
| Antiviral Medications | Paxlovid, Remdesivir | Oseltamivir (Tamiflu), Zanamivir (Relenza), Baloxavir Marboxil (Xofluza) |
| Hospitalization | Oxygen therapy, mechanical ventilation, corticosteroids | Oxygen therapy, mechanical ventilation |
It’s important to consult with a healthcare provider for appropriate diagnosis and treatment recommendations for both COVID-19 and the flu. Early treatment can help reduce the risk of severe outcomes and improve recovery.
9. Impact on Healthcare Systems: Strain and Resource Allocation
The COVID-19 pandemic placed an unprecedented strain on healthcare systems worldwide. The surge in cases and hospitalizations overwhelmed hospitals, intensive care units (ICUs), and healthcare personnel. The need for specialized equipment, such as ventilators and personal protective equipment (PPE), led to shortages and logistical challenges.
The pandemic also disrupted routine medical care and elective procedures, leading to delays in diagnosis and treatment for other health conditions. Healthcare workers faced immense pressure and burnout, which exacerbated staffing shortages.
Seasonal influenza also places a burden on healthcare systems each year, but the impact is generally less severe compared to the COVID-19 pandemic. Flu seasons can lead to increased hospitalizations and strain on emergency departments, but healthcare systems are typically better prepared to manage seasonal flu outbreaks.
The COVID-19 pandemic highlighted the need for increased investment in public health infrastructure, healthcare surge capacity, and preparedness for future pandemics. Strategies such as expanding telehealth services, improving data collection and surveillance, and strengthening the healthcare workforce are essential for mitigating the impact of future outbreaks.
10. Economic Consequences: Costs and Productivity Losses
Both COVID-19 and the flu have significant economic consequences due to healthcare costs, productivity losses, and disruptions to supply chains. The COVID-19 pandemic has had a far greater economic impact compared to seasonal influenza, due to the scale of the pandemic, the severity of illness, and the implementation of lockdowns and other public health measures.
The economic costs of COVID-19 include:
- Healthcare costs: Hospitalizations, treatments, and long-term care for COVID-19 patients.
- Productivity losses: Sick leave, reduced productivity due to illness, and premature mortality.
- Business closures: Lockdowns and reduced consumer spending led to business closures and job losses.
- Supply chain disruptions: The pandemic disrupted global supply chains, leading to shortages and increased prices.
- Government spending: Governments spent trillions of dollars on economic stimulus packages, unemployment benefits, and healthcare initiatives.
The economic costs of seasonal influenza include healthcare costs and productivity losses due to illness. However, the overall economic impact of the flu is generally lower compared to COVID-19.
Strategies for mitigating the economic impact of both COVID-19 and the flu include promoting vaccination, implementing preventive measures, providing economic support to businesses and individuals, and investing in public health infrastructure.
11. Public Health Measures: Effectiveness and Impact
Public health measures played a critical role in controlling the spread of both COVID-19 and the flu. These measures include:
- Mask-wearing: Masks can reduce the transmission of respiratory droplets.
- Social distancing: Maintaining physical distance from others can reduce the risk of infection.
- Hand hygiene: Frequent handwashing with soap and water or using hand sanitizer can kill viruses.
- Quarantine and isolation: Isolating infected individuals and quarantining close contacts can prevent further spread.
- Contact tracing: Identifying and notifying individuals who may have been exposed to the virus can help break chains of transmission.
- Travel restrictions: Limiting travel can prevent the spread of the virus across regions and countries.
- School and business closures: Closing schools and businesses can reduce social interactions and transmission.
The effectiveness of these measures depends on factors such as adherence, timing, and the specific characteristics of the virus. During the COVID-19 pandemic, stringent public health measures, such as lockdowns and mask mandates, were implemented to control the spread of the virus. These measures had a significant impact on reducing transmission but also had economic and social consequences.
For seasonal influenza, public health measures such as vaccination, hand hygiene, and staying home when sick are recommended to reduce transmission. School closures and other more stringent measures may be implemented during severe flu seasons.
12. Psychological Effects: Mental Health and Well-being
The COVID-19 pandemic has had a profound impact on mental health and well-being. The pandemic led to increased stress, anxiety, depression, and social isolation. Factors contributing to these psychological effects include:
- Fear of infection: Concerns about contracting the virus and transmitting it to loved ones.
- Social isolation: Lockdowns and social distancing measures led to reduced social interactions.
- Economic hardship: Job losses and financial insecurity caused stress and anxiety.
- Grief and loss: The death of loved ones and the loss of routines and social connections.
- Uncertainty: The unpredictable nature of the pandemic and the lack of clear information contributed to anxiety.
Studies have shown a significant increase in the prevalence of mental health disorders during the pandemic. Children and adolescents have also experienced psychological effects, such as increased anxiety and depression, due to school closures and social isolation.
Seasonal influenza can also have psychological effects, but these are generally less severe compared to the COVID-19 pandemic. Feeling unwell with the flu can lead to temporary mood changes and fatigue.
Strategies for promoting mental health and well-being during both COVID-19 and flu seasons include:
- Self-care: Engaging in activities that promote relaxation and well-being, such as exercise, meditation, and spending time in nature.
- Social connection: Maintaining social connections through phone calls, video chats, or safe in-person interactions.
- Seeking support: Reaching out to mental health professionals or support groups for help.
- Limiting exposure to negative news: Reducing exposure to stressful news and information can help reduce anxiety.
13. The Role of Variants: How They Change the Game
The emergence of variants of both COVID-19 and the flu has significantly impacted the course of the pandemic and seasonal flu seasons. Variants can differ in terms of transmissibility, severity, and immune evasion.
COVID-19 variants, such as Alpha, Beta, Delta, and Omicron, have emerged with different characteristics. The Delta variant was associated with increased severity and higher hospitalization rates, while the Omicron variant was highly transmissible but generally less severe. Variants can also evade immunity from prior infection or vaccination, leading to breakthrough infections.
Influenza viruses also undergo frequent mutations, leading to the emergence of new strains each year. This is why influenza vaccines are updated annually to match the circulating strains. The process of antigenic drift allows influenza viruses to gradually change over time, while antigenic shift can lead to the emergence of novel strains that can cause pandemics.
Monitoring and tracking variants is essential for understanding their impact and developing appropriate public health responses. Genomic surveillance, which involves sequencing viral genomes, can help identify new variants and track their spread.
14. Future Outlook: What’s Next for COVID-19 and Flu?
The future outlook for COVID-19 and the flu involves ongoing challenges and uncertainties. COVID-19 is likely to become an endemic disease, meaning it will continue to circulate in the population, but at lower levels. Vaccination, antiviral treatments, and public health measures will continue to play a role in managing COVID-19.
The flu will continue to cause seasonal epidemics each year. The development of more effective influenza vaccines and antiviral treatments is an ongoing priority.
Preparedness for future pandemics is also essential. This includes investing in public health infrastructure, developing rapid diagnostics and vaccines, and strengthening healthcare systems.
15. Expert Opinions: Insights from Medical Professionals
Medical professionals offer valuable insights into the comparison between COVID-19 and the flu. Experts emphasize the importance of vaccination for both viruses, particularly for high-risk individuals. They also highlight the need for early diagnosis and treatment to reduce the risk of severe outcomes.
Experts caution against complacency, as both COVID-19 and the flu can cause serious illness and death. They recommend staying informed about the latest public health guidance and taking preventive measures to protect oneself and others.
16. Personal Experiences: Stories from Those Affected
Personal experiences provide a human perspective on the impact of COVID-19 and the flu. Stories from individuals who have had these illnesses can help illustrate the symptoms, severity, and long-term effects. Hearing from others can also provide support and encouragement.
17. COMPARE.EDU.VN: Your Resource for Informed Decisions
COMPARE.EDU.VN is dedicated to providing you with clear, objective comparisons to help you make informed decisions. Our detailed analysis of COVID-19 and the flu equips you with the knowledge to understand the differences and protect your health. We offer comprehensive comparisons across various topics, from product reviews to educational resources, empowering you to choose what’s best for your needs.
Feeling overwhelmed by the choices? Visit compare.edu.vn to explore detailed comparisons and make confident decisions. Contact us at 333 Comparison Plaza, Choice City, CA 90210, United States or Whatsapp: +1 (626) 555-9090.
18. Frequently Asked Questions (FAQ)
1. Is COVID-19 more dangerous than the flu?
Yes, especially during the early stages of the pandemic, COVID-19 was more dangerous due to higher mortality rates and potential for severe complications. However, with vaccination and less severe variants, the risk has decreased.
2. Can you get both COVID-19 and the flu at the same time?
Yes, co-infection is possible and can lead to more severe illness.
3. How can I tell if I have COVID-19 or the flu?
Symptoms can be similar, so diagnostic testing (PCR for COVID-19, rapid antigen tests for both) is necessary for accurate diagnosis.
4. What are the long-term effects of COVID-19?
Long COVID can include fatigue, shortness of breath, cognitive dysfunction, and organ damage.
5. How effective are the vaccines for COVID-19 and the flu?
Both vaccines are effective in reducing the risk of infection, severe illness, and death.
6. What are the treatment options for COVID-19?
Antiviral medications (Paxlovid, Remdesivir) and supportive care are used.
7. What are the treatment options for the flu?
Antiviral medications (Oseltamivir, Zanamivir, Baloxavir Marboxil) and supportive care are used.
8. How can I prevent the spread of COVID-19 and the flu?
Vaccination, mask-wearing, social distancing, and hand hygiene are effective measures.
9. Is there a difference in mortality rates between COVID-19 and the flu now?
The mortality rate for COVID-19 has decreased but can still be higher than the flu, depending on the variant and individual risk factors.
10. What should I do if I think I have COVID-19 or the flu?
Consult with a healthcare provider for diagnosis and treatment recommendations.