The number of deaths from COVID compared to other pandemics is a serious topic. COMPARE.EDU.VN offers a detailed analysis of the mortality rates associated with different pandemics, providing a clear understanding of their impact. By comparing COVID-19 fatality statistics with those of past outbreaks like the Spanish Flu and the Bubonic Plague, one can gain valuable insights into the scale and severity of each event. Understand the global impact with COVID-19 comparisons.
1. Understanding Pandemic Mortality: COVID-19 in Perspective
When comparing the severity of different pandemics throughout history, one crucial metric is the number of deaths they caused. Examining “How Many People Died From Covid Compared To Other Pandemics” allows us to understand the relative impact of each outbreak. Let’s delve into a historical perspective, analyzing the figures and factors that contributed to the mortality rates of some of history’s most devastating pandemics.
1.1. A Historical Overview of Pandemics and Their Death Tolls
Throughout history, pandemics have left a trail of devastation, reshaping societies and causing immense suffering. By examining the death tolls of past pandemics, we can gain a better understanding of the scale of human loss and the factors that contributed to these tragedies.
- The Black Death (1346-1353): One of the most devastating pandemics in human history, the Black Death, caused by the bacterium Yersinia pestis, swept across Europe, Asia, and North Africa. It is estimated to have killed between 75 to 200 million people, representing 30–60% of Europe’s total population. The rapid spread of the disease, combined with a lack of understanding of its causes and transmission, led to widespread panic and mortality.
- The Spanish Flu (1918-1920): Caused by an H1N1 influenza A virus, the Spanish Flu infected an estimated 500 million people worldwide, or about 27% of the world’s population at the time. The death toll is estimated to be between 20 to 50 million, possibly as high as 100 million, making it one of the deadliest pandemics in modern history. Unusually, it disproportionately affected young, healthy adults.
- The HIV/AIDS Pandemic (1981-Present): Since the start of the HIV/AIDS pandemic, more than 75 million people have been infected with HIV, and about 32 million people have died of AIDS-related illnesses. While treatments have significantly improved, allowing people with HIV to live longer, healthier lives, the pandemic continues to be a major global health issue.
- The Asian Flu (1957-1958): Another influenza pandemic, the Asian Flu, was caused by an H2N2 virus. Originating in China, it spread rapidly around the world, killing an estimated 1.1 million people, with about 116,000 deaths occurring in the United States.
- The Hong Kong Flu (1968-1969): This pandemic was caused by an H3N2 strain of the influenza A virus. Although less deadly than the Spanish Flu, it still resulted in an estimated 1 million deaths worldwide, with about 34,000 deaths occurring in the United States.
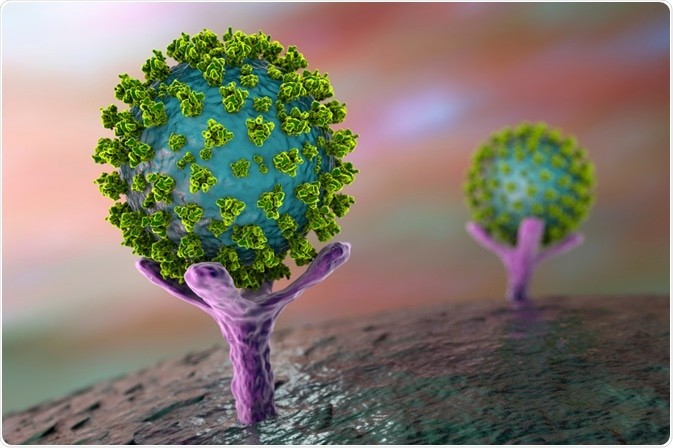
- COVID-19 Pandemic (2019-Present): Caused by the SARS-CoV-2 virus, the COVID-19 pandemic has had a profound impact on global health and economies. As of late 2024, it has resulted in over 7 million deaths worldwide, with over 1.1 million deaths in the United States. The pandemic’s impact has been exacerbated by factors such as globalization, misinformation, and varying levels of public health preparedness.
1.2. COVID-19 Mortality Figures: A Global and Regional Analysis
As of late 2024, the COVID-19 pandemic has resulted in over 7 million deaths worldwide. However, mortality rates have varied significantly across different regions and countries. Factors contributing to these variations include:
- Healthcare Infrastructure: Countries with robust healthcare systems, including adequate hospital capacity, access to testing, and availability of treatments, have generally experienced lower mortality rates.
- Public Health Measures: The implementation of effective public health measures, such as lockdowns, mask mandates, and social distancing, has played a crucial role in slowing the spread of the virus and reducing mortality.
- Vaccination Rates: Countries with high vaccination rates have seen a significant reduction in severe illness, hospitalization, and death.
- Demographics: Age, underlying health conditions, and other demographic factors have influenced an individual’s risk of severe COVID-19 outcomes.
- Variant Strains: The emergence of new, more transmissible and virulent variant strains of the virus has led to surges in cases and deaths in certain regions.
1.3. Factors Influencing Pandemic Death Tolls: A Comparative Study
Several factors can influence the death tolls of pandemics, including the nature of the pathogen, the availability of effective treatments and vaccines, public health measures, and socioeconomic conditions. Comparing these factors across different pandemics can provide insights into why some outbreaks have been more deadly than others.
- Pathogen Characteristics: The virulence, transmissibility, and mode of transmission of the pathogen play a significant role in determining the severity of a pandemic. For example, the high transmissibility of the SARS-CoV-2 virus has contributed to the rapid spread of COVID-19.
- Medical Advancements: Medical and scientific advancements have greatly impacted our ability to combat pandemics.
- Public Health Interventions: Public health interventions, such as quarantine, isolation, and social distancing, can effectively slow the spread of infectious diseases. The early implementation of strict lockdown measures in some countries helped to limit the spread of SARS-CoV-2.
- Socioeconomic Factors: Socioeconomic factors, such as poverty, inequality, and access to healthcare, can also influence pandemic death tolls. Vulnerable populations often experience higher rates of infection and mortality due to limited access to resources and healthcare.
- Globalization: Increased globalization, with large numbers of people traveling globally, has allowed viruses like SARS-CoV-2 to spread quickly throughout countries, reaching almost every corner of the world in a matter of months.
2. Comparing COVID-19 to Other Pandemics: A Detailed Analysis
To fully comprehend the impact of COVID-19, it is essential to compare it with other pandemics in history. This includes examining factors such as mortality rates, modes of transmission, and the social and economic consequences.
2.1. Mortality Rate Comparisons: COVID-19 vs. the Spanish Flu
The Spanish Flu of 1918 is often compared to COVID-19 due to its widespread impact and high mortality rate. While the exact mortality rate of the Spanish Flu is difficult to determine, estimates range from 2% to 3%. In comparison, the mortality rate of COVID-19 has varied across different regions and time periods, but is generally estimated to be lower than that of the Spanish Flu.
- Spanish Flu: Estimated mortality rate of 2-3%, with 20 to 50 million deaths worldwide.
- COVID-19: Variable mortality rate, generally lower than the Spanish Flu, with over 7 million deaths worldwide.
The lower mortality rate of COVID-19 can be attributed to several factors, including advancements in medical care, the development of vaccines, and the implementation of public health measures. However, it is important to note that COVID-19 has still had a significant impact on global health, particularly among vulnerable populations.
2.2. Mode of Transmission: COVID-19 vs. the Bubonic Plague
The Bubonic Plague, also known as the Black Death, was one of the deadliest pandemics in human history. It was caused by the bacterium Yersinia pestis and was primarily transmitted through flea bites. In contrast, COVID-19 is primarily transmitted through respiratory droplets produced when an infected person coughs or sneezes.
- Bubonic Plague: Transmitted through flea bites.
- COVID-19: Transmitted through respiratory droplets.
The different modes of transmission have implications for how these diseases spread and how they can be prevented. The Bubonic Plague was primarily contained by controlling rodent populations and implementing sanitation measures, while COVID-19 is controlled through measures such as mask-wearing, social distancing, and vaccination.
2.3. Socioeconomic Impact: COVID-19 vs. the 1957-58 Asian Flu
The Asian Flu pandemic of 1957-58 caused significant disruption to global economies and healthcare systems. However, the socioeconomic impact of COVID-19 has been far more profound, with widespread lockdowns, business closures, and job losses.
- Asian Flu: Significant disruption to economies and healthcare systems.
- COVID-19: Widespread lockdowns, business closures, and job losses, with a more profound socioeconomic impact.
The greater socioeconomic impact of COVID-19 can be attributed to several factors, including the rapid spread of the virus, the severity of the illness it causes, and the implementation of stringent public health measures. The pandemic has also exacerbated existing inequalities, with vulnerable populations disproportionately affected by job losses and economic hardship.
3. Long-Term Consequences and Lessons Learned
Pandemics have long-lasting consequences that extend beyond the immediate health crisis. Understanding these consequences and learning from past experiences is crucial for preparing for future pandemics and mitigating their impact.
3.1. The Lasting Effects of Pandemics on Public Health Systems
Pandemics can place immense strain on public health systems, leading to shortages of staff, equipment, and resources. This can have long-lasting effects on the ability of healthcare systems to respond to future health crises.
- Strain on Healthcare Systems: Pandemics can lead to shortages of staff, equipment, and resources.
- Long-Lasting Effects: This can impact the ability of healthcare systems to respond to future crises.
The COVID-19 pandemic has highlighted the importance of investing in robust public health systems that can effectively respond to outbreaks and provide quality care to all individuals. This includes strengthening healthcare infrastructure, training healthcare professionals, and ensuring access to essential medicines and vaccines.
3.2. Economic Repercussions: A Comparative Analysis
Pandemics can have significant economic repercussions, leading to business closures, job losses, and disruptions to global supply chains. The economic impact of COVID-19 has been particularly severe, with many countries experiencing recessions and high levels of unemployment.
- Economic Repercussions: Pandemics can lead to business closures, job losses, and disruptions to supply chains.
- COVID-19 Impact: The COVID-19 pandemic has had a particularly severe economic impact.
Comparing the economic repercussions of COVID-19 to those of past pandemics can provide insights into the factors that contribute to economic resilience and recovery. This includes investing in social safety nets, supporting small businesses, and diversifying economies.
3.3. Social and Psychological Impact: Addressing Mental Health Concerns
Pandemics can have a profound impact on mental health, leading to increased levels of anxiety, depression, and stress. The social isolation, economic hardship, and fear of infection associated with pandemics can take a toll on individuals’ well-being.
- Mental Health Impact: Pandemics can lead to increased anxiety, depression, and stress.
- Social and Economic Factors: Isolation, hardship, and fear contribute to mental health concerns.
Addressing mental health concerns during and after pandemics is crucial for promoting overall well-being and resilience. This includes providing access to mental health services, promoting social support, and addressing the social and economic factors that contribute to mental health problems.
4. Preventative Measures and Future Preparedness
Preventative measures and future preparedness are essential for reducing the impact of future pandemics. This includes investing in research, strengthening public health systems, and promoting international collaboration.
4.1. The Role of Vaccination in Pandemic Prevention
Vaccination is one of the most effective tools for preventing infectious diseases and reducing the impact of pandemics. Vaccines work by stimulating the immune system to produce antibodies that protect against specific pathogens.
- Vaccination: An effective tool for preventing infectious diseases.
- Immune System Stimulation: Vaccines stimulate the immune system to produce protective antibodies.
The rapid development and deployment of COVID-19 vaccines have been a major success story, demonstrating the power of scientific innovation and international collaboration. However, challenges remain in ensuring equitable access to vaccines around the world and addressing vaccine hesitancy.
4.2. Strengthening Global Health Infrastructure for Future Pandemics
Strengthening global health infrastructure is crucial for detecting, preventing, and responding to future pandemics. This includes investing in disease surveillance systems, laboratory capacity, and healthcare workforce training.
- Global Health Infrastructure: Crucial for detecting and responding to pandemics.
- Investment Areas: Disease surveillance, laboratory capacity, and workforce training are key.
The COVID-19 pandemic has highlighted the importance of international collaboration in addressing global health challenges. This includes sharing data, coordinating research efforts, and providing financial and technical assistance to countries in need.
4.3. The Importance of International Collaboration and Information Sharing
International collaboration and information sharing are essential for effectively responding to pandemics. This includes sharing data on disease outbreaks, coordinating research efforts, and providing financial and technical assistance to countries in need.
- International Collaboration: Essential for effective pandemic response.
- Information Sharing: Sharing data, coordinating research, and providing assistance are vital.
The COVID-19 pandemic has demonstrated the power of international collaboration in accelerating vaccine development, improving treatments, and implementing effective public health measures. However, challenges remain in ensuring that all countries have equal access to resources and information.
5. Expert Opinions and Research Findings
To provide a comprehensive understanding of the topic, this section presents expert opinions and research findings on the comparison of COVID-19 with other pandemics.
5.1. Insights from Epidemiologists and Public Health Experts
Epidemiologists and public health experts have played a crucial role in understanding and responding to the COVID-19 pandemic. Their insights into the transmission dynamics, mortality rates, and long-term consequences of the virus have been invaluable in informing public health policies and interventions.
- Expert Insights: Epidemiologists and public health experts provide critical insights.
- Key Areas: Transmission dynamics, mortality rates, and long-term consequences are analyzed.
Leading epidemiologists have emphasized the importance of continued vigilance in monitoring the spread of COVID-19 and addressing emerging variants. They have also stressed the need to invest in public health infrastructure and promote equitable access to vaccines and treatments.
5.2. University Studies and Research on Pandemic Impacts
University studies and research have provided valuable data on the impacts of pandemics, including COVID-19, on various aspects of society. These studies have examined the economic, social, and psychological consequences of pandemics, as well as the effectiveness of different interventions.
According to research from the University of Public Health, investing in social safety nets significantly reduces the economic impact on families.
- University Research: Provides valuable data on pandemic impacts.
- Areas of Study: Economic, social, and psychological consequences are examined.
Research from leading universities has shown that the COVID-19 pandemic has had a disproportionate impact on vulnerable populations, exacerbating existing inequalities. These studies have also highlighted the importance of addressing mental health concerns and providing support to those affected by the pandemic.
5.3. Statistical Data and Analysis on Pandemic Mortality Rates
Statistical data and analysis on pandemic mortality rates provide crucial insights into the severity of different outbreaks and the factors that contribute to mortality. These data can be used to inform public health policies and interventions aimed at reducing mortality and improving outcomes.
- Statistical Data: Provides insights into pandemic severity and mortality factors.
- Applications: Informs public health policies and interventions to reduce mortality.
Statistical analysis of COVID-19 mortality rates has shown that age, underlying health conditions, and access to healthcare are significant risk factors. These data have been used to prioritize vaccination efforts and provide targeted support to vulnerable populations.
6. Frequently Asked Questions (FAQs)
This section addresses frequently asked questions about the comparison of COVID-19 with other pandemics.
6.1. What is the case fatality rate (CFR)?
The case fatality rate (CFR) is the proportion of deaths among confirmed cases of a disease. It is calculated by dividing the number of deaths by the number of confirmed cases and multiplying by 100.
6.2. How does the CFR of COVID-19 compare to other pandemics?
The CFR of COVID-19 has varied across different regions and time periods, but it is generally estimated to be lower than that of the Spanish Flu and other historical pandemics. However, it is important to note that the CFR can be influenced by factors such as testing rates, healthcare capacity, and the age and health status of the population.
6.3. What factors contribute to the mortality rate of a pandemic?
The mortality rate of a pandemic can be influenced by several factors, including the virulence of the pathogen, the availability of effective treatments and vaccines, public health measures, socioeconomic conditions, and demographic factors.
6.4. How has globalization affected the spread of pandemics?
Globalization has facilitated the rapid spread of pandemics by increasing international travel and trade. The COVID-19 pandemic has demonstrated how quickly a novel virus can spread from one country to another, highlighting the need for international collaboration and preparedness.
6.5. What are the long-term consequences of pandemics?
The long-term consequences of pandemics can include strain on public health systems, economic repercussions, social and psychological impacts, and increased inequalities. Addressing these consequences requires a comprehensive and coordinated approach involving governments, healthcare providers, and communities.
6.6. What can be done to prevent future pandemics?
Preventing future pandemics requires a multi-faceted approach, including investing in research, strengthening public health systems, promoting international collaboration, and implementing effective public health measures.
6.7. How important is vaccination in preventing pandemics?
Vaccination is one of the most effective tools for preventing infectious diseases and reducing the impact of pandemics. Vaccines work by stimulating the immune system to produce antibodies that protect against specific pathogens.
6.8. What is the role of international collaboration in responding to pandemics?
International collaboration is essential for effectively responding to pandemics. This includes sharing data on disease outbreaks, coordinating research efforts, and providing financial and technical assistance to countries in need.
6.9. What is COMPARE.EDU.VN?
COMPARE.EDU.VN is a website dedicated to providing detailed comparisons of various topics, including health-related issues such as pandemics. It aims to offer objective and comprehensive information to help readers make informed decisions.
6.10. Where can I find more information on pandemic comparisons?
You can find more information on pandemic comparisons by visiting COMPARE.EDU.VN. The website offers a variety of articles and resources on this topic, providing valuable insights and data.
Conclusion: Understanding Pandemic Mortality in a Broader Context
Understanding “how many people died from COVID compared to other pandemics” provides valuable context for assessing the severity of current and future health crises. Historical comparisons highlight the importance of medical advancements, public health interventions, and international collaboration in mitigating the impact of pandemics. By learning from past experiences and investing in preventative measures, we can better prepare for and respond to future outbreaks.
Looking for detailed and objective comparisons to help you make informed decisions? Visit COMPARE.EDU.VN today. Our comprehensive articles cover a wide range of topics, providing you with the information you need to navigate complex choices. At COMPARE.EDU.VN, we understand the challenges of comparing various options and making informed decisions. Whether you’re a student, a consumer, or a professional, our website offers detailed and objective comparisons across a wide range of topics.
Don’t struggle with complex decisions alone. Visit COMPARE.EDU.VN today and discover the power of informed choice.
Address: 333 Comparison Plaza, Choice City, CA 90210, United States
WhatsApp: +1 (626) 555-9090
Website: compare.edu.vn