Navigating the complexities of healthcare systems can be daunting, especially when trying to understand how the United States stacks up against other nations. COMPARE.EDU.VN provides a detailed comparison, offering insights into healthcare access, quality, and cost-effectiveness. By exploring these differences, you can gain a clearer perspective on the strengths and weaknesses of the U.S. healthcare model and potential areas for improvement. This analysis helps you in making informed decisions regarding healthcare options and policies, enhancing health and wellness awareness, and promoting better healthcare solutions through comparative effectiveness research and healthcare policy analysis.
1. What Are The Key Differences In Healthcare Systems Between The US And Other Developed Countries?
The U.S. healthcare system differs significantly from those in other developed countries in several key areas, including financing, access, and regulation. Unlike many developed nations that offer universal healthcare through single-payer systems or social insurance models, the U.S. relies on a mix of private and public insurance, leading to disparities in coverage and access.
1.1. Healthcare Coverage Models
Most developed countries operate under universal healthcare systems, ensuring all citizens have access to medical services. These systems are typically funded through taxes and managed by the government or quasi-governmental entities. In contrast, the U.S. employs a multi-payer system comprising private insurance (employer-sponsored and individual plans), government-funded programs like Medicare (for the elderly and disabled) and Medicaid (for low-income individuals), and out-of-pocket payments.
1.2. Access To Care
Universal healthcare systems generally offer broader access to care compared to the U.S. In countries like Canada and the United Kingdom, residents do not face financial barriers to essential medical services. The U.S., however, struggles with ensuring universal access due to high costs and coverage gaps. According to a 2020 study by the Organization for Economic Co-operation and Development (OECD), 26.8% of Americans reported skipping medical consultations due to cost, compared to an average of 7.0% in comparable countries.
1.3. Healthcare Financing
The U.S. spends significantly more on healthcare per capita than other developed countries, yet often achieves poorer health outcomes. In 2021, the U.S. spent approximately $12,914 per person on healthcare, while the average among OECD countries was around $5,671. This higher spending does not necessarily translate to better quality or access, highlighting inefficiencies within the U.S. system.
1.4. Regulation And Oversight
The level of government regulation in healthcare also varies widely. Countries with universal healthcare typically have strong regulatory frameworks to control costs and ensure quality. The U.S. system, characterized by a mix of private and public entities, faces challenges in achieving consistent standards and cost control.
2. How Does Healthcare Spending In The US Compare To Other Nations?
The United States consistently spends more on healthcare per capita than any other developed nation, yet its health outcomes often lag behind. This discrepancy raises questions about the efficiency and effectiveness of the U.S. healthcare spending.
2.1. Per Capita Spending
In 2021, the U.S. spent $12,914 per capita on healthcare, far exceeding the OECD average of $5,671. Countries like Switzerland ($7,037), Germany ($6,626), and the Netherlands ($6,132) also have high healthcare expenditures but remain significantly lower than the U.S.
2.2. Spending As A Percentage Of GDP
Healthcare spending in the U.S. accounts for a larger percentage of its Gross Domestic Product (GDP) compared to other developed countries. In 2021, healthcare spending represented 17.8% of the U.S. GDP, while the OECD average was 9.7%. This higher proportion indicates that healthcare consumes a larger share of the U.S. economy, potentially diverting resources from other sectors.
2.3. Factors Contributing To High Spending
Several factors contribute to the high healthcare spending in the U.S., including:
- Administrative Costs: The U.S. has higher administrative costs due to its complex multi-payer system. Dealing with multiple insurance companies and varying billing practices increases overhead expenses.
- Drug Prices: Prescription drug prices in the U.S. are significantly higher than in other countries. Unlike many nations, the U.S. government does not directly negotiate drug prices with manufacturers.
- Service Costs: The cost of medical services, such as doctor visits and hospital stays, is generally higher in the U.S. compared to other developed countries.
- Technology: The U.S. tends to adopt new medical technologies more quickly, which can drive up costs.
- Defensive Medicine: Some healthcare providers may practice defensive medicine, ordering more tests and procedures to avoid potential lawsuits, further increasing expenses.
2.4. Impact On The Economy
High healthcare costs can strain the U.S. economy by reducing funds available for other public and private investments. They can also lead to higher insurance premiums, lower wages, and increased national debt. Additionally, high healthcare expenses can create financial hardships for individuals and families, leading to medical debt and delayed or forgone care.
3. What Are The Health Outcomes In The US Compared To Other Wealthy Countries?
Despite its high healthcare spending, the U.S. often lags behind other wealthy countries in key health outcomes, such as life expectancy, infant mortality, and chronic disease management.
3.1. Life Expectancy
Life expectancy in the U.S. is lower than in many other developed countries. In 2020, the average life expectancy in the U.S. was 77.3 years, compared to the OECD average of 80.7 years. Countries like Japan (84.8 years), Switzerland (84 years), and Australia (83.2 years) have significantly higher life expectancies.
3.2. Infant Mortality
The infant mortality rate in the U.S. is also higher than in most other wealthy nations. In 2020, the U.S. infant mortality rate was 5.4 deaths per 1,000 live births, while the OECD average was 4.1 deaths per 1,000 live births. Countries like Japan (1.9 deaths), Finland (2.1 deaths), and Slovenia (1.6 deaths) have much lower infant mortality rates.
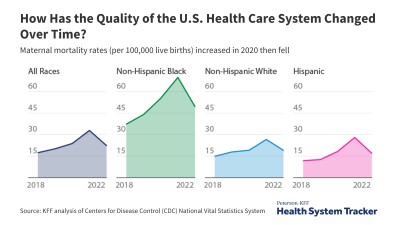
3.3. Maternal Mortality
The U.S. has a notably high maternal mortality rate compared to other developed countries. According to the Centers for Disease Control and Prevention (CDC), the maternal mortality rate in the U.S. was 23.8 deaths per 100,000 live births in 2020, while many European countries reported rates below 10 deaths per 100,000 live births.
3.4. Chronic Disease Management
The U.S. faces challenges in managing chronic diseases such as diabetes, heart disease, and asthma. While the U.S. has made advancements in medical technology and treatment options, these benefits are not consistently accessible to all segments of the population. Factors such as socioeconomic status, access to preventive care, and lifestyle choices can significantly impact the prevalence and management of chronic diseases.
3.5. Preventable Deaths
The U.S. has a higher rate of preventable deaths compared to other wealthy countries. Preventable deaths include those from conditions that could have been avoided with timely and effective medical care. According to a study by the Commonwealth Fund, the U.S. had a higher rate of deaths from preventable causes such as heart disease, stroke, and diabetes compared to countries like Canada, the United Kingdom, and Australia.
3.6. Factors Contributing To Poorer Outcomes
Several factors contribute to the poorer health outcomes in the U.S., including:
- Lack Of Universal Coverage: The absence of universal healthcare coverage results in many Americans lacking access to timely and appropriate medical care.
- High Costs: High healthcare costs can deter individuals from seeking medical care or adhering to prescribed treatments.
- Socioeconomic Disparities: Socioeconomic disparities, such as poverty and lack of education, can significantly impact health outcomes.
- Lifestyle Factors: Lifestyle factors such as diet, exercise, and smoking can contribute to poorer health outcomes.
4. How Does Access To Healthcare Differ In The US Compared To Countries With Universal Healthcare?
Access to healthcare is a significant point of divergence between the U.S. and countries with universal healthcare systems. Universal healthcare aims to ensure that all citizens have access to necessary medical services, regardless of their ability to pay. In contrast, the U.S. system faces challenges in providing equitable access to care.
4.1. Universal Coverage
Countries with universal healthcare systems, such as Canada, the United Kingdom, and Australia, provide coverage to all citizens through government-funded programs. These systems typically eliminate or minimize out-of-pocket costs for essential medical services, ensuring that financial barriers do not prevent people from seeking care.
4.2. Insurance Coverage In The US
In the U.S., health insurance coverage is primarily obtained through employer-sponsored plans, individual purchases, or government-funded programs like Medicare and Medicaid. However, a significant portion of the population remains uninsured or underinsured, leading to difficulties in accessing healthcare services.
4.3. Uninsured Rate
Despite the Affordable Care Act (ACA), a substantial number of Americans remain uninsured. In 2021, approximately 8.3% of the U.S. population, or 27.5 million people, were uninsured. This lack of coverage can result in delayed or forgone care, leading to poorer health outcomes and higher healthcare costs in the long run.
4.4. Underinsurance
Even among those with health insurance, many are underinsured, meaning their coverage may not adequately protect them from high out-of-pocket costs. High deductibles, co-payments, and co-insurance can deter individuals from seeking necessary medical care, especially for those with chronic conditions or complex health needs.
4.5. Impact Of Cost On Access
Cost is a major barrier to healthcare access in the U.S. Many Americans report skipping medical consultations, delaying treatment, or not filling prescriptions due to cost concerns. According to a study by the Kaiser Family Foundation, approximately 41% of adults reported delaying or forgoing medical care due to cost in 2022.
4.6. Health Disparities
Access to healthcare in the U.S. is also affected by health disparities, with certain populations facing greater challenges in obtaining necessary medical services. Racial and ethnic minorities, low-income individuals, and those living in rural areas often experience poorer access to care due to factors such as lack of insurance, transportation barriers, and limited availability of healthcare providers.
4.7. Timeliness Of Care
In countries with universal healthcare, patients may face longer wait times for certain elective procedures or specialist appointments. However, these systems generally ensure timely access to emergency and essential medical services. In the U.S., while access to emergency care is guaranteed, delays in obtaining preventive care, chronic disease management, and specialist consultations can occur due to insurance restrictions, provider availability, and administrative hurdles.
5. What Are The Strengths And Weaknesses Of The US Healthcare System?
The U.S. healthcare system has notable strengths, such as innovation and advanced medical technology, but also significant weaknesses, including high costs and unequal access.
5.1. Strengths Of The US Healthcare System
- Innovation: The U.S. is a leader in medical innovation, with substantial investments in research and development. This has led to groundbreaking discoveries, advanced treatments, and cutting-edge technologies that improve patient care.
- Specialized Care: The U.S. offers a wide range of specialized medical services and highly skilled healthcare professionals. Patients have access to experts in various fields, enabling them to receive advanced and tailored care.
- Choice: The U.S. system provides patients with greater choice in selecting their healthcare providers, hospitals, and insurance plans. This autonomy allows individuals to customize their healthcare experience to some extent.
- Emergency Care: The U.S. has a well-developed emergency care system, ensuring that individuals receive prompt medical attention in life-threatening situations. Emergency departments are equipped to handle a wide range of medical emergencies.
- Quality Of Care: In certain areas, the U.S. provides high-quality care, particularly for complex medical conditions and specialized treatments. Many U.S. hospitals and medical centers are renowned for their excellence and attract patients from around the world.
5.2. Weaknesses Of The US Healthcare System
- High Costs: The U.S. healthcare system is the most expensive in the world, placing a significant burden on individuals, families, and the economy. High costs can deter people from seeking necessary medical care and contribute to medical debt.
- Lack Of Universal Coverage: The absence of universal healthcare coverage results in many Americans lacking access to timely and appropriate medical care. This can lead to poorer health outcomes and increased healthcare costs in the long run.
- Administrative Complexity: The U.S. healthcare system is characterized by administrative complexity, with multiple insurance companies, billing practices, and regulatory requirements. This can lead to inefficiencies, increased costs, and confusion for patients and providers.
- Health Disparities: The U.S. faces significant health disparities, with certain populations experiencing poorer access to care and worse health outcomes. Racial and ethnic minorities, low-income individuals, and those living in rural areas are particularly affected.
- Focus On Treatment Rather Than Prevention: The U.S. healthcare system tends to prioritize treatment of illnesses over preventive care. This can result in delayed diagnoses, more advanced stages of disease, and higher healthcare costs.
6. How Does The US Perform In Terms Of Healthcare Quality And Patient Safety?
The U.S. healthcare system presents a mixed picture in terms of healthcare quality and patient safety. While it excels in certain areas, such as specialized care and medical technology, it lags behind other developed countries in key quality indicators and patient safety measures.
6.1. Quality Of Care Indicators
- Preventive Care: The U.S. performs relatively well in certain preventive care measures, such as vaccination rates and cancer screenings. However, disparities exist across different populations, with some groups experiencing lower rates of preventive care.
- Chronic Disease Management: The U.S. faces challenges in managing chronic diseases such as diabetes, heart disease, and asthma. While advanced treatments are available, access to comprehensive care, including education, lifestyle support, and regular monitoring, is not consistently provided.
- Acute Care: In certain areas of acute care, such as heart attack and stroke treatment, the U.S. performs favorably compared to other countries. However, variations in quality exist across different hospitals and regions.
- Patient Experience: Patient experience scores in the U.S. are mixed. While some patients report positive experiences with their healthcare providers, others express dissatisfaction with issues such as communication, coordination of care, and shared decision-making.
6.2. Patient Safety Measures
- Hospital-Acquired Infections: The U.S. has made progress in reducing hospital-acquired infections (HAIs), such as methicillin-resistant Staphylococcus aureus (MRSA) and Clostridium difficile (C. diff). However, HAIs remain a significant concern, and further efforts are needed to prevent their occurrence.
- Medical Errors: Medical errors, including medication errors, surgical errors, and diagnostic errors, are a persistent problem in the U.S. healthcare system. Efforts to improve patient safety include implementing standardized protocols, enhancing communication, and promoting a culture of safety.
- Adverse Events: Adverse events, such as falls, pressure ulcers, and preventable readmissions, can negatively impact patient outcomes and increase healthcare costs. Hospitals and healthcare systems are working to reduce adverse events through quality improvement initiatives and patient safety programs.
6.3. International Comparisons
When compared to other developed countries, the U.S. often lags behind in key quality indicators and patient safety measures. For example, the U.S. has higher rates of hospital readmissions, surgical complications, and medication errors compared to countries like Canada, the United Kingdom, and Australia.
6.4. Factors Affecting Quality And Safety
Several factors can affect healthcare quality and patient safety in the U.S., including:
- System Fragmentation: The U.S. healthcare system is fragmented, with multiple payers, providers, and regulatory agencies. This can lead to communication gaps, lack of coordination, and inconsistent standards of care.
- Inadequate Resources: Some healthcare facilities, particularly those serving underserved populations, may lack adequate resources, such as staffing, equipment, and technology. This can compromise the quality and safety of care.
- Workforce Issues: Workforce issues, such as nursing shortages and physician burnout, can impact patient safety and quality of care. Overworked and stressed healthcare professionals may be more prone to errors and less able to provide optimal care.
7. What Role Does Health Insurance Play In Healthcare Access And Quality In The US?
Health insurance plays a critical role in healthcare access and quality in the U.S. It determines whether individuals can afford necessary medical care, the types of services they can access, and the quality of care they receive.
7.1. Insurance Coverage And Access
- Uninsured Population: A significant portion of the U.S. population remains uninsured, which directly impacts their ability to access healthcare services. Uninsured individuals are more likely to delay or forgo medical care, leading to poorer health outcomes and higher healthcare costs in the long run.
- Underinsured Population: Many Americans are underinsured, meaning they have health insurance but face high deductibles, co-payments, and co-insurance. This can deter them from seeking necessary medical care, particularly for those with chronic conditions or complex health needs.
- Coverage Gaps: Gaps in insurance coverage, such as limited benefits, restrictive provider networks, and pre-existing condition exclusions, can also limit access to care. These coverage gaps can disproportionately affect vulnerable populations, such as low-income individuals and those with disabilities.
7.2. Insurance Type And Quality
- Private Insurance: Private health insurance plans, including employer-sponsored plans and individual market plans, offer varying levels of coverage and access to care. Some private plans provide comprehensive benefits, broad provider networks, and enhanced care coordination, while others offer more limited coverage.
- Public Insurance: Public health insurance programs, such as Medicare and Medicaid, provide coverage to specific populations, such as the elderly, disabled, and low-income individuals. These programs play a crucial role in ensuring access to care for vulnerable populations, but they may also have limitations, such as lower reimbursement rates and administrative challenges.
- Managed Care: Managed care plans, such as health maintenance organizations (HMOs) and preferred provider organizations (PPOs), aim to control costs and improve quality through various mechanisms, such as provider networks, utilization management, and quality improvement initiatives. However, managed care plans can also face criticism for restricting patient choice and limiting access to certain services.
7.3. Impact On Health Outcomes
- Preventive Care: Health insurance can facilitate access to preventive care services, such as vaccinations, screenings, and check-ups. Insured individuals are more likely to receive preventive care, which can help detect and manage health problems early, leading to better outcomes.
- Chronic Disease Management: Health insurance can support chronic disease management by providing coverage for medications, doctor visits, and other necessary services. Insured individuals are more likely to adhere to treatment plans and receive ongoing care, which can improve their health and quality of life.
- Hospital Care: Health insurance can ensure access to timely and appropriate hospital care in case of serious illness or injury. Insured individuals are more likely to receive necessary hospital services, such as surgery, diagnostic tests, and rehabilitation, leading to better recovery and reduced risk of complications.
7.4. Challenges And Reforms
The role of health insurance in the U.S. healthcare system is subject to ongoing debate and reform efforts. Challenges include high premiums, rising deductibles, coverage gaps, and administrative complexity. Policy proposals aimed at improving health insurance coverage and quality include expanding access to affordable coverage, strengthening consumer protections, and reforming payment models.
 Healthcare spending per capita among OECD countries
Healthcare spending per capita among OECD countries
8. What Are Some Common Criticisms Of The US Healthcare System?
The U.S. healthcare system faces numerous criticisms, ranging from high costs and lack of universal coverage to administrative complexity and health disparities.
8.1. High Costs
- Excessive Spending: The U.S. spends more on healthcare per capita than any other developed country, yet its health outcomes often lag behind. This raises questions about the efficiency and value of healthcare spending.
- Drug Prices: Prescription drug prices in the U.S. are significantly higher than in other countries, contributing to high healthcare costs.
- Administrative Costs: The U.S. healthcare system has high administrative costs due to its complex multi-payer system and regulatory requirements.
- Service Costs: The cost of medical services, such as doctor visits, hospital stays, and procedures, is generally higher in the U.S. compared to other developed countries.
8.2. Lack Of Universal Coverage
- Uninsured Population: A significant portion of the U.S. population remains uninsured, which limits their access to healthcare services and contributes to poorer health outcomes.
- Underinsured Population: Many Americans are underinsured, meaning they have health insurance but face high out-of-pocket costs, which can deter them from seeking necessary medical care.
- Coverage Gaps: Gaps in insurance coverage, such as limited benefits and pre-existing condition exclusions, can also limit access to care.
8.3. Administrative Complexity
- Multi-Payer System: The U.S. healthcare system is characterized by a complex multi-payer system, with multiple insurance companies, billing practices, and regulatory agencies.
- Bureaucracy: The administrative burden associated with insurance claims, paperwork, and compliance requirements can be overwhelming for patients, providers, and healthcare organizations.
- Lack Of Coordination: The fragmented nature of the U.S. healthcare system can lead to a lack of coordination among different providers and healthcare settings, resulting in inefficiencies and errors.
8.4. Health Disparities
- Socioeconomic Disparities: Socioeconomic factors, such as poverty, lack of education, and limited access to resources, can significantly impact health outcomes.
- Racial And Ethnic Disparities: Racial and ethnic minorities often experience poorer access to care and worse health outcomes compared to white individuals, due to factors such as discrimination, cultural barriers, and lack of insurance.
- Geographic Disparities: Individuals living in rural areas may face barriers to healthcare access, such as limited availability of healthcare providers, transportation challenges, and lack of specialized services.
8.5. Focus On Treatment Rather Than Prevention
- Reactive Care: The U.S. healthcare system tends to prioritize treatment of illnesses over preventive care, which can result in delayed diagnoses, more advanced stages of disease, and higher healthcare costs.
- Lack Of Emphasis On Wellness: There is a need for greater emphasis on promoting wellness, healthy lifestyles, and disease prevention through education, community-based programs, and policy initiatives.
9. What Are Some Potential Reforms Or Changes That Could Improve The US Healthcare System?
Numerous potential reforms and changes could improve the U.S. healthcare system, addressing issues such as high costs, lack of universal coverage, administrative complexity, and health disparities.
9.1. Universal Healthcare
- Single-Payer System: Implementing a single-payer healthcare system, similar to those in Canada and the United Kingdom, could ensure universal coverage and simplify administration.
- Public Option: Creating a public health insurance option that competes with private plans could increase access to affordable coverage and drive down costs.
- Medicaid Expansion: Expanding Medicaid eligibility to cover more low-income individuals could reduce the number of uninsured and improve access to care.
9.2. Cost Control Measures
- Drug Price Negotiation: Allowing the government to negotiate drug prices with pharmaceutical companies could lower prescription drug costs.
- Value-Based Care: Shifting from fee-for-service to value-based care models could incentivize providers to deliver high-quality, cost-effective care.
- Price Transparency: Requiring hospitals and providers to disclose prices for services could help consumers make informed decisions and promote competition.
9.3. Administrative Simplification
- Standardized Billing: Implementing standardized billing practices across different payers could reduce administrative costs and streamline the claims process.
- Electronic Health Records: Promoting the adoption and effective use of electronic health records could improve care coordination and reduce paperwork.
- Consolidated Insurance Market: Reducing the number of insurance companies and consolidating the insurance market could simplify administration and lower costs.
9.4. Health Disparities Reduction
- Targeted Interventions: Implementing targeted interventions to address the specific needs of vulnerable populations could reduce health disparities and improve outcomes.
- Community Health Programs: Investing in community health programs could promote wellness, prevent disease, and improve access to care in underserved areas.
- Cultural Competency Training: Providing cultural competency training for healthcare providers could improve communication and reduce cultural barriers to care.
9.5. Preventive Care Emphasis
- Wellness Programs: Encouraging the development and implementation of wellness programs could promote healthy lifestyles and prevent chronic diseases.
- Preventive Services Coverage: Ensuring comprehensive coverage for preventive services, such as vaccinations, screenings, and check-ups, could improve early detection and management of health problems.
- Public Health Investments: Increasing investments in public health infrastructure and initiatives could promote community health and prevent disease outbreaks.
10. Where Can I Find More Information To Compare Healthcare Systems?
For those seeking additional information to compare healthcare systems, several reputable organizations and resources offer comprehensive data and analysis.
10.1. Organization For Economic Co-Operation And Development (OECD)
The OECD provides extensive data and analysis on healthcare systems in its member countries, including the U.S. The OECD Health Statistics database offers detailed information on healthcare spending, utilization, quality, and outcomes.
10.2. The Commonwealth Fund
The Commonwealth Fund is a private foundation that conducts research and analysis on healthcare issues. Its website features numerous reports, articles, and interactive tools comparing healthcare systems in the U.S. and other countries.
10.3. The Kaiser Family Foundation (KFF)
KFF is a non-profit organization that provides information and analysis on health policy issues. Its website offers a wealth of data, reports, and policy briefs on healthcare spending, coverage, access, and quality.
10.4. The World Health Organization (WHO)
The WHO provides global health statistics and information on healthcare systems around the world. Its website features reports, publications, and data sets on health outcomes, healthcare financing, and health system performance.
10.5. Government Agencies
Several U.S. government agencies offer data and information on healthcare, including the Centers for Medicare & Medicaid Services (CMS), the Centers for Disease Control and Prevention (CDC), and the National Institutes of Health (NIH). These agencies provide data on healthcare spending, utilization, quality, and outcomes, as well as research and policy analysis.
10.6. Academic Institutions
Many academic institutions conduct research on healthcare systems and policy. Universities such as Harvard, Yale, and Johns Hopkins have centers and departments dedicated to studying healthcare issues. These institutions often publish research papers, reports, and policy briefs on healthcare topics.
10.7. COMPARE.EDU.VN
COMPARE.EDU.VN offers comprehensive comparisons and insights into various aspects of healthcare. Our platform provides detailed analyses, expert opinions, and user reviews to help you make informed decisions about healthcare options.
By consulting these resources, individuals can gain a deeper understanding of the strengths and weaknesses of the U.S. healthcare system and how it compares to those in other developed countries. This knowledge can inform policy debates, improve healthcare decision-making, and promote better health outcomes for all.
Want to delve deeper into the nuances of healthcare comparisons? Visit COMPARE.EDU.VN today for detailed analyses, user reviews, and expert opinions that help you make informed decisions. Compare healthcare plans, assess treatment options, and understand the latest healthcare trends. Empower your health choices with COMPARE.EDU.VN!
Address: 333 Comparison Plaza, Choice City, CA 90210, United States
Whatsapp: +1 (626) 555-9090
Website: COMPARE.EDU.VN
FAQ: Comparing US Healthcare to Other Countries
1. Why is healthcare so expensive in the US compared to other countries?
The high cost of healthcare in the U.S. is due to several factors, including high administrative costs from a multi-payer system, inflated drug prices, higher service costs, rapid adoption of new technologies, and defensive medicine practices.
2. How does the US healthcare system compare in terms of quality to other developed nations?
While the U.S. excels in specialized care and medical technology, it often lags behind other developed countries in key quality indicators, such as life expectancy, infant mortality, and preventable deaths.
3. What are the main differences between the US healthcare system and universal healthcare systems?
The U.S. relies on a mix of private and public insurance, leading to coverage disparities, while countries with universal healthcare provide coverage to all citizens through government-funded programs, ensuring broader access to care.
4. How does access to healthcare differ in the US compared to countries with universal healthcare?
In the U.S., access to healthcare is often limited by cost and insurance coverage, resulting in many Americans delaying or forgoing necessary medical care. Universal healthcare systems aim to eliminate financial barriers, ensuring equitable access for all citizens.
5. What are some strengths of the US healthcare system?
Strengths of the U.S. healthcare system include its innovation in medical technology, specialized care, patient choice, emergency care system, and high quality of care in certain areas.
6. What are some weaknesses of the US healthcare system?
Weaknesses include high costs, lack of universal coverage, administrative complexity, health disparities, and a focus on treatment rather than prevention.
7. How does health insurance affect healthcare access and quality in the US?
Health insurance plays a critical role in healthcare access and quality in the U.S., determining whether individuals can afford necessary medical care, the types of services they can access, and the quality of care they receive.
8. What are the common criticisms of the US healthcare system?
Common criticisms include high costs, lack of universal coverage, administrative complexity, health disparities, and a focus on treatment rather than prevention.
9. What potential reforms could improve the US healthcare system?
Potential reforms include implementing universal healthcare through a single-payer system or public option, controlling costs through drug price negotiation and value-based care models, simplifying administration, reducing health disparities through targeted interventions, and emphasizing preventive care.
10. Where can I find more detailed comparisons of healthcare systems?
You can find more detailed comparisons from organizations like the OECD, The Commonwealth Fund, Kaiser Family Foundation (KFF), the World Health Organization (WHO), government agencies like CMS and CDC, and academic institutions. Also, visit compare.edu.vn for comprehensive analyses and expert opinions.