Hydrocodone compared to oxycodone, both powerful pain relievers, are frequently prescribed opioids managing moderate to severe pain. At COMPARE.EDU.VN, we understand choosing the right pain management option is crucial, so we provide a comprehensive comparison of hydrocodone versus oxycodone, including efficacy, side effects, and potential risks. This guide offers a detailed look at opioid analgesics and prescription painkillers, helping you and your healthcare provider make informed decisions.
1. Understanding Opioid Pain Relievers
Opioid pain relievers are a class of medications that work by binding to opioid receptors in the brain, spinal cord, and other areas of the body. This process reduces the perception of pain. Hydrocodone and oxycodone are both derived from the opium poppy, although synthetic versions are also available. They are prescribed to alleviate pain following surgery, injuries, or chronic conditions.
1.1 How Opioids Work
Opioids work by mimicking the body’s natural pain-relieving chemicals, known as endorphins. When these drugs bind to opioid receptors, they not only reduce pain but can also produce feelings of euphoria. This effect is one reason why opioids can be addictive.
1.2 Common Uses for Hydrocodone and Oxycodone
Both hydrocodone and oxycodone are commonly prescribed for:
- Post-operative pain: Managing pain after surgical procedures.
- Injury-related pain: Alleviating pain from fractures, sprains, and other injuries.
- Chronic pain conditions: Helping manage chronic pain from conditions like arthritis, back pain, or cancer.
- Dental pain: Controlling pain after dental procedures.
1.3 Important Considerations
Before starting either medication, it’s essential to consider:
- Addiction risk: Opioids carry a significant risk of addiction and dependence.
- Side effects: Common side effects include constipation, nausea, drowsiness, and respiratory depression.
- Drug interactions: Opioids can interact with other medications, including alcohol, sedatives, and antidepressants.
- Individual health conditions: Certain medical conditions, such as liver or kidney disease, can affect how these drugs are metabolized.
2. Hydrocodone: A Closer Look
Hydrocodone is a semi-synthetic opioid analgesic synthesized from codeine, another opiate drug. It is often combined with other pain relievers, such as acetaminophen or ibuprofen, to enhance its effectiveness.
2.1 Common Formulations
Hydrocodone is available in various formulations, including:
- Hydrocodone/Acetaminophen (Vicodin, Norco): Combines hydrocodone with acetaminophen for pain relief and fever reduction.
- Hydrocodone/Ibuprofen (Vicoprofen): Combines hydrocodone with ibuprofen, an NSAID, to reduce pain and inflammation.
- Extended-release hydrocodone (Zohydro ER, Hysingla ER): Provides a longer-lasting effect for chronic pain management.
2.2 Dosage and Administration
The dosage of hydrocodone varies depending on the severity of pain, the patient’s medical history, and other medications they may be taking. It is typically taken orally, with or without food.
2.3 Side Effects of Hydrocodone
Common side effects of hydrocodone include:
- Constipation: A frequent side effect that can be managed with stool softeners or laxatives.
- Nausea and vomiting: Can be reduced by taking the medication with food.
- Drowsiness and dizziness: Patients should avoid driving or operating heavy machinery while taking hydrocodone.
- Respiratory depression: A serious side effect that can be life-threatening, especially at high doses or when combined with other sedatives.
- Itching: Some individuals may experience itching as a side effect.
2.4 Precautions and Contraindications
Hydrocodone should be used with caution in patients with:
- Respiratory problems: Such as asthma or COPD, due to the risk of respiratory depression.
- Liver or kidney disease: As these conditions can affect drug metabolism and elimination.
- History of substance abuse: Due to the risk of addiction and dependence.
- Head injuries or increased intracranial pressure: As opioids can mask neurological symptoms.
3. Oxycodone: A Detailed Examination
Oxycodone is a semi-synthetic opioid analgesic derived from thebaine, an opium alkaloid. Like hydrocodone, it is often combined with other pain relievers to increase its efficacy.
3.1 Common Formulations
Oxycodone is available in various formulations, including:
- Oxycodone/Acetaminophen (Percocet): Combines oxycodone with acetaminophen for pain relief and fever reduction.
- Oxycodone/Aspirin (Percodan): Combines oxycodone with aspirin to reduce pain and inflammation.
- Oxycodone (OxyContin, Roxicodone): Available as both immediate-release and extended-release formulations.
3.2 Dosage and Administration
The dosage of oxycodone depends on the severity of pain, the patient’s medical history, and other medications they may be taking. It is typically taken orally, with or without food.
3.3 Side Effects of Oxycodone
Common side effects of oxycodone include:
- Constipation: Similar to hydrocodone, constipation is a frequent side effect.
- Nausea and vomiting: Can be managed by taking the medication with food.
- Drowsiness and dizziness: Patients should avoid activities requiring alertness while taking oxycodone.
- Respiratory depression: A serious side effect that requires careful monitoring.
- Headache: Some individuals may experience headaches.
3.4 Precautions and Contraindications
Oxycodone should be used with caution in patients with:
- Respiratory problems: Such as asthma or COPD.
- Liver or kidney disease: As these conditions can affect drug metabolism and elimination.
- History of substance abuse: Due to the risk of addiction and dependence.
- Head injuries or increased intracranial pressure: As opioids can mask neurological symptoms.
4. Hydrocodone vs. Oxycodone: Key Differences and Similarities
While hydrocodone and oxycodone are both opioid pain relievers, they have some key differences and similarities. Understanding these nuances can help healthcare providers make informed decisions about which medication is most appropriate for their patients.
4.1 Similarities Between Hydrocodone and Oxycodone
- Mechanism of Action: Both drugs work by binding to opioid receptors in the brain and spinal cord, reducing the perception of pain.
- Indications: Both are used to treat moderate to severe pain following surgery, injuries, or chronic conditions.
- Side Effects: Both share common side effects such as constipation, nausea, drowsiness, and respiratory depression.
- Addiction Potential: Both carry a significant risk of addiction and dependence.
4.2 Differences Between Hydrocodone and Oxycodone
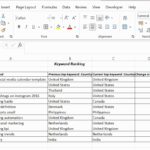
| Feature | Hydrocodone | Oxycodone |
|---|---|---|
| Potency | Generally considered less potent | Generally considered more potent |
| Formulations | Often combined with acetaminophen or ibuprofen | Available as single-ingredient and combination products |
| Availability | Available in various generic forms | Available in both generic and brand-name forms |
| Onset of Action | Similar onset of action | Similar onset of action |
| Duration of Action | Similar duration of action | Similar duration of action |
4.3 Potency
Oxycodone is generally considered more potent than hydrocodone. This means that a lower dose of oxycodone may provide the same level of pain relief as a higher dose of hydrocodone. However, individual responses to these medications can vary.
4.4 Formulations
Hydrocodone is often combined with other pain relievers, such as acetaminophen or ibuprofen, while oxycodone is available both as a single-ingredient product and in combination with other pain relievers.
4.5 Availability
Both hydrocodone and oxycodone are available in various generic forms, making them relatively accessible. However, certain formulations or brand-name versions may have specific availability considerations.
5. Efficacy and Effectiveness
Numerous studies have compared the efficacy and effectiveness of hydrocodone and oxycodone in managing pain. While individual results may vary, research suggests that both medications can be effective in relieving moderate to severe pain.
5.1 Comparative Studies
- Short-term pain relief: Studies have shown that both hydrocodone and oxycodone provide similar levels of pain relief in the short term, such as after surgery or injury.
- Chronic pain management: Some studies suggest that oxycodone may be slightly more effective in managing chronic pain, but more research is needed.
- Individual response: The effectiveness of each medication can vary depending on individual factors such as metabolism, pain tolerance, and other health conditions.
5.2 Patient Preferences
Patient preferences can also play a role in determining which medication is most effective. Some individuals may find that one medication works better for them than the other, even if studies show similar overall efficacy.
5.3 Expert Opinions
Medical experts generally agree that both hydrocodone and oxycodone can be effective pain relievers when used appropriately. However, they also emphasize the importance of considering individual patient factors and potential risks before prescribing either medication.
6. Side Effect Profiles
Understanding the side effect profiles of hydrocodone and oxycodone is crucial for managing patient expectations and minimizing potential adverse effects.
6.1 Common Side Effects
Both medications share common side effects such as:
- Constipation: A frequent side effect that can be managed with lifestyle changes or medications.
- Nausea and vomiting: Can be reduced by taking the medication with food or using antiemetic drugs.
- Drowsiness and dizziness: Patients should avoid activities requiring alertness while taking these medications.
- Respiratory depression: A serious side effect that requires careful monitoring, especially in high-risk patients.
- Itching: Some individuals may experience itching as a side effect.
6.2 Less Common Side Effects
Less common side effects of both medications include:
- Headache: Some individuals may experience headaches.
- Dry mouth: Can be managed with increased fluid intake or saliva substitutes.
- Sweating: Some individuals may experience excessive sweating.
- Anxiety: Opioids can sometimes cause anxiety or mood changes.
6.3 Managing Side Effects
Strategies for managing side effects include:
- Lifestyle changes: Such as increasing fiber intake and staying hydrated to manage constipation.
- Medications: Such as stool softeners, antiemetics, or antihistamines to relieve specific symptoms.
- Dosage adjustments: Reducing the dose of the medication may help minimize side effects.
- Alternative therapies: Such as acupuncture or physical therapy, may help manage pain and reduce the need for opioids.
7. Risks of Addiction and Dependence
Both hydrocodone and oxycodone carry a significant risk of addiction and dependence. It is crucial to understand these risks and take steps to minimize them.
7.1 Understanding Addiction
Addiction is a chronic, relapsing brain disease characterized by compulsive drug seeking and use, despite harmful consequences. It is a complex condition influenced by genetic, environmental, and psychological factors.
7.2 Understanding Dependence
Dependence is a physiological adaptation to a drug, where the body becomes accustomed to its presence. When the drug is stopped abruptly, withdrawal symptoms can occur. Dependence is not the same as addiction, although it can be a component of addiction.
7.3 Risk Factors for Addiction
Risk factors for opioid addiction include:
- Personal or family history of substance abuse: Individuals with a history of substance abuse are at higher risk.
- Mental health disorders: Such as depression, anxiety, or PTSD.
- Young age: Adolescents and young adults are more vulnerable to addiction.
- Easy access to opioids: Such as through prescriptions or family members.
7.4 Minimizing the Risk of Addiction
Strategies for minimizing the risk of opioid addiction include:
- Using the lowest effective dose: Prescribing the lowest dose that provides adequate pain relief.
- Limiting the duration of use: Avoiding long-term opioid use whenever possible.
- Regular monitoring: Closely monitoring patients for signs of addiction or misuse.
- Patient education: Educating patients about the risks of addiction and the importance of following their doctor’s instructions.
- Alternative therapies: Exploring non-opioid pain management options whenever possible.
8. Drug Interactions
Hydrocodone and oxycodone can interact with other medications, potentially leading to serious side effects. It is crucial to inform your doctor about all the medications you are taking, including prescription drugs, over-the-counter medications, and herbal supplements.
8.1 Common Drug Interactions
Common drug interactions include:
- Alcohol: Combining opioids with alcohol can increase the risk of respiratory depression and overdose.
- Benzodiazepines: Such as diazepam or lorazepam, can also increase the risk of respiratory depression and overdose.
- Antidepressants: Such as SSRIs or MAOIs, can interact with opioids and cause serotonin syndrome.
- Antihistamines: Can increase drowsiness and dizziness.
- Muscle relaxants: Can increase the risk of respiratory depression.
8.2 Managing Drug Interactions
Strategies for managing drug interactions include:
- Avoiding certain combinations: Such as opioids with alcohol or benzodiazepines.
- Adjusting dosages: Reducing the dose of one or both medications.
- Monitoring for side effects: Closely monitoring patients for signs of adverse reactions.
- Alternative therapies: Exploring alternative pain management options that do not interact with other medications.
9. Special Populations
Certain populations, such as pregnant women, elderly individuals, and those with liver or kidney disease, require special considerations when using hydrocodone or oxycodone.
9.1 Pregnant Women
Opioid use during pregnancy can lead to neonatal abstinence syndrome (NAS) in newborns. NAS is a condition where the baby experiences withdrawal symptoms after birth. Pregnant women should only use opioids when the benefits outweigh the risks, and under close medical supervision.
9.2 Elderly Individuals
Elderly individuals are more sensitive to the effects of opioids and are at higher risk for side effects such as respiratory depression, confusion, and falls. Lower doses and careful monitoring are essential.
9.3 Liver and Kidney Disease
Liver and kidney disease can affect the metabolism and elimination of opioids, increasing the risk of side effects. Patients with these conditions may require lower doses or alternative pain management options.
10. Alternative Pain Management Options
Non-opioid pain management options can be effective for many individuals and can help reduce the reliance on opioids.
10.1 Non-Pharmacological Therapies
Non-pharmacological therapies include:
- Physical therapy: Can help improve strength, flexibility, and range of motion.
- Acupuncture: May help relieve pain by stimulating specific points on the body.
- Massage therapy: Can help reduce muscle tension and pain.
- Cognitive-behavioral therapy (CBT): Can help patients manage pain by changing their thoughts and behaviors.
- Yoga and meditation: Can help reduce stress and pain.
10.2 Non-Opioid Medications
Non-opioid medications include:
- Acetaminophen (Tylenol): Effective for mild to moderate pain.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Such as ibuprofen or naproxen, can reduce pain and inflammation.
- Antidepressants: Such as duloxetine or amitriptyline, can help manage chronic pain conditions.
- Anticonvulsants: Such as gabapentin or pregabalin, can help manage nerve pain.
11. Legal and Regulatory Considerations
Hydrocodone and oxycodone are controlled substances and are subject to strict legal and regulatory requirements.
11.1 Controlled Substance Classifications
- Hydrocodone: Typically classified as a Schedule II or Schedule III controlled substance, depending on the formulation.
- Oxycodone: Typically classified as a Schedule II controlled substance.
11.2 Prescription Requirements
Prescriptions for hydrocodone and oxycodone must be written by a licensed healthcare provider and are subject to strict regulations regarding refills and transfers.
11.3 Legal Consequences of Misuse
Misuse, abuse, or illegal distribution of hydrocodone or oxycodone can result in serious legal consequences, including fines, imprisonment, and loss of professional licensure.
12. The Role of Healthcare Providers
Healthcare providers play a crucial role in managing pain and minimizing the risks associated with opioid use.
12.1 Patient Assessment
Healthcare providers should conduct a thorough patient assessment before prescribing hydrocodone or oxycodone, including:
- Medical history: Including any history of substance abuse, mental health disorders, or other medical conditions.
- Pain assessment: Evaluating the severity, location, and duration of pain.
- Risk assessment: Assessing the patient’s risk for addiction and misuse.
12.2 Patient Education
Healthcare providers should educate patients about:
- The risks and benefits of opioid use.
- The importance of following their doctor’s instructions.
- The potential side effects of the medication.
- The signs and symptoms of addiction.
- Safe storage and disposal of unused medications.
12.3 Monitoring and Follow-Up
Healthcare providers should regularly monitor patients who are taking hydrocodone or oxycodone, including:
- Assessing pain relief.
- Monitoring for side effects.
- Screening for signs of addiction or misuse.
- Adjusting dosages as needed.
13. Hydrocodone and Oxycodone: The Takeaway
Both hydrocodone and oxycodone are powerful pain medications used to treat moderate to severe pain. While they share similarities, such as their mechanism of action and common side effects, they also have differences in potency and formulations. It is crucial to work closely with your healthcare provider to determine which medication is most appropriate for your individual needs and to minimize the risks associated with opioid use.
13.1 Making Informed Decisions
When considering hydrocodone and oxycodone, it is essential to:
- Discuss your pain management options with your healthcare provider.
- Understand the risks and benefits of each medication.
- Consider alternative pain management options.
- Follow your doctor’s instructions carefully.
- Store and dispose of unused medications safely.
13.2 The Future of Pain Management
The field of pain management is constantly evolving, with new treatments and approaches being developed. As research continues, healthcare providers will have more tools to help patients manage pain effectively and safely.
14. Frequently Asked Questions (FAQ)
1. What is the main difference between hydrocodone and oxycodone?
Oxycodone is generally considered more potent than hydrocodone, meaning a lower dose may provide the same level of pain relief.
2. Which drug is stronger, hydrocodone or oxycodone?
Oxycodone is typically considered stronger than hydrocodone.
3. Can I switch between hydrocodone and oxycodone?
Switching medications should only be done under the guidance of a healthcare provider, as dosage adjustments may be necessary.
4. What are the common side effects of hydrocodone and oxycodone?
Common side effects include constipation, nausea, drowsiness, and respiratory depression.
5. Are hydrocodone and oxycodone addictive?
Yes, both medications carry a significant risk of addiction and dependence.
6. Can I take hydrocodone or oxycodone with alcohol?
No, combining opioids with alcohol can increase the risk of serious side effects, including respiratory depression and overdose.
7. What should I do if I experience side effects while taking hydrocodone or oxycodone?
Contact your healthcare provider if you experience any concerning side effects.
8. How should I store unused hydrocodone or oxycodone?
Store medications in a safe place, out of reach of children and pets. Follow your healthcare provider’s instructions for disposal.
9. Are there alternative pain management options to hydrocodone and oxycodone?
Yes, alternative options include physical therapy, acupuncture, non-opioid medications, and cognitive-behavioral therapy.
10. What should I do if I think someone is addicted to hydrocodone or oxycodone?
Seek professional help from a healthcare provider or addiction specialist.
Conclusion
Choosing the right pain management strategy involves careful consideration of various factors, including the type and severity of pain, individual health conditions, and potential risks and benefits of different medications. Hydrocodone and oxycodone are both effective options for managing moderate to severe pain, but they should be used judiciously and under close medical supervision. At COMPARE.EDU.VN, we strive to provide comprehensive and unbiased information to help you make informed decisions about your health.
Are you struggling to compare pain relief options? Do you need detailed, objective comparisons to help you decide? Visit compare.edu.vn today for comprehensive guides, user reviews, and expert analyses. Make the best choice for your health with the information you need at your fingertips. Contact us at 333 Comparison Plaza, Choice City, CA 90210, United States, or reach out via Whatsapp at +1 (626) 555-9090.
Hydrocodone and oxycodone tablets: a visual comparison showcasing differences in appearance and branding between the two opioid pain relievers.
A selection of pain relief medications displayed, illustrating the range of options available for managing different types and levels of pain.
A symbolic image representing opioid addiction treatment, emphasizing the importance of seeking help and support for recovery.
An illustration depicting various strategies for managing chronic pain, including medication, physical therapy, and lifestyle adjustments.