How do COVID deaths compare to other pandemics? COMPARE.EDU.VN provides an in-depth analysis, juxtaposing the mortality rates and impacts of COVID-19 with those of historical pandemics to clarify its severity. Understanding these comparisons offers critical insights into pandemic management, healthcare responses, and global preparedness.
1. What Factors Influence COVID-19 Death Rates Compared to Previous Pandemics?
COVID-19 death rates, when compared to previous pandemics, are influenced by a multitude of factors, including advancements in medical science, public health measures, and the demographics of affected populations. While the raw numbers might seem alarming, understanding these nuances is critical.
1.1. Medical Advancements and Healthcare Infrastructure
Modern medicine possesses diagnostic tools, treatments, and supportive care strategies that were unavailable during previous pandemics. For example, during the 1918 Spanish Flu pandemic, supportive care was limited, and antibiotics were not yet available to treat secondary bacterial infections, a major cause of death. Today, sophisticated intensive care units (ICUs), antiviral medications, and treatments like dexamethasone have significantly improved survival rates for severely ill COVID-19 patients. According to a study by the University of Oxford in June 2021, dexamethasone reduced deaths by up to one-third in hospitalized patients with severe respiratory complications.
1.2. Public Health Measures
The implementation of public health measures such as mask-wearing, social distancing, and vaccination campaigns has played a crucial role in mitigating the spread and severity of COVID-19. In contrast, during the 1918 pandemic, public health interventions were often limited and less coordinated. The rapid development and deployment of COVID-19 vaccines represent a significant advancement. Studies have shown that vaccines are highly effective in preventing severe disease, hospitalization, and death. Data from the CDC indicates that unvaccinated individuals are significantly more likely to be hospitalized or die from COVID-19 compared to vaccinated individuals.
1.3. Demographic and Socioeconomic Factors
Demographic factors such as age, underlying health conditions, and access to healthcare also significantly influence COVID-19 death rates. Older adults and individuals with comorbidities such as diabetes, heart disease, and obesity are at higher risk of severe illness and death. Socioeconomic disparities, including limited access to healthcare, crowded living conditions, and occupational exposures, can exacerbate the impact of the pandemic on vulnerable populations. A study published in The Lancet in March 2021 highlighted the disproportionate impact of COVID-19 on minority communities in the United States, attributing this to systemic inequalities in healthcare access and socioeconomic factors.
1.4. Viral Characteristics and Variants
The evolution of SARS-CoV-2 into various variants, such as Alpha, Delta, and Omicron, has also influenced death rates. Some variants, like Delta, were associated with increased transmissibility and disease severity, leading to surges in hospitalizations and deaths. The emergence of Omicron, while highly transmissible, has generally been associated with less severe disease, particularly in vaccinated individuals. Genetic mutations in these variants affect how the virus interacts with the human immune system and the effectiveness of existing treatments.
1.5. Data Collection and Reporting
Differences in data collection and reporting methodologies across countries and over time can also impact comparisons of death rates. Variations in testing strategies, case definitions, and mortality reporting practices can introduce biases and inconsistencies. For example, some countries may only report deaths directly attributed to COVID-19, while others may include deaths where COVID-19 was a contributing factor. Accurate and consistent data are essential for understanding the true impact of the pandemic and informing public health policies.
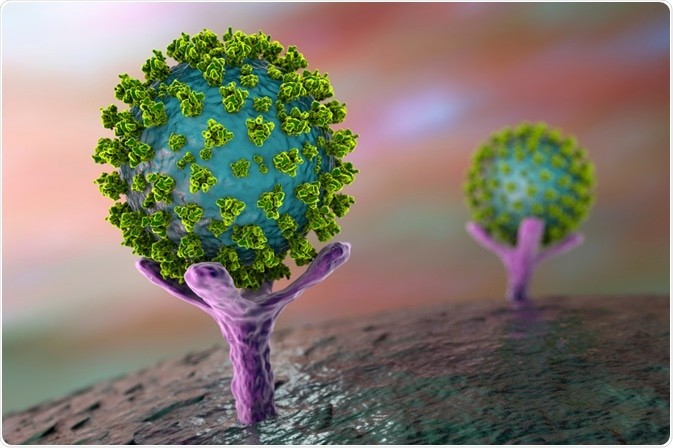
SARS-CoV-2, the virus causing COVID-19, under microscopic view.
2. How Does the Fatality Rate of COVID-19 Compare to the Spanish Flu?
The fatality rate of COVID-19 is generally lower than that of the Spanish Flu, but understanding the differences requires a nuanced approach. The Spanish Flu, which occurred from 1918 to 1920, had an estimated case fatality rate (CFR) of 2% to 3%, with some estimates going even higher. In contrast, the CFR for COVID-19 has varied across different regions and time periods but has generally been lower, often around 1% or less, according to the World Health Organization.
2.1. Historical Context of the Spanish Flu
The Spanish Flu pandemic occurred during World War I, which significantly impacted its spread and severity. Overcrowded military camps and troop movements facilitated the rapid transmission of the virus. Additionally, healthcare systems were overwhelmed by the war effort, and resources were scarce. The lack of effective treatments, antibiotics for secondary bacterial infections, and vaccines contributed to the high fatality rate. Malnutrition and poor living conditions further weakened immune systems, making individuals more susceptible to severe illness.
2.2. Advancements in Medical Care
One of the primary reasons for the lower CFR of COVID-19 is the significant advancement in medical care over the past century. Modern medicine has developed sophisticated diagnostic tools, antiviral medications, and supportive care strategies that were unavailable during the Spanish Flu. For instance, the use of ventilators, extracorporeal membrane oxygenation (ECMO), and other advanced respiratory support techniques has improved survival rates for critically ill COVID-19 patients.
2.3. Public Health Interventions
Public health interventions have also played a crucial role in mitigating the spread and severity of COVID-19. Measures such as mask-wearing, social distancing, and lockdowns have helped to slow transmission rates. The rapid development and deployment of COVID-19 vaccines represent a significant advancement compared to the Spanish Flu era. Vaccines have been highly effective in preventing severe disease, hospitalization, and death.
2.4. Demographic Factors
Demographic factors also contribute to the differences in fatality rates. The Spanish Flu disproportionately affected young adults, whereas COVID-19 has primarily impacted older adults and individuals with underlying health conditions. This difference in age distribution influences the overall CFR. Older adults are generally more vulnerable to severe illness and death from respiratory infections due to age-related declines in immune function.
2.5. Data and Reporting Differences
It’s essential to consider differences in data collection and reporting methodologies when comparing CFRs across pandemics. During the Spanish Flu, data collection was less systematic, and many cases and deaths may have gone uncounted. In contrast, COVID-19 has been tracked more closely, although variations in testing strategies and mortality reporting practices still exist across countries. Accurate and consistent data are crucial for understanding the true impact of each pandemic.
3. How Do COVID-19 Deaths Compare to the Bubonic Plague?
Comparing COVID-19 deaths to the bubonic plague requires understanding the vastly different contexts and characteristics of these two diseases. The bubonic plague, particularly the Black Death in the 14th century, was one of the deadliest pandemics in human history. The Black Death resulted in an estimated 75 to 200 million deaths in Eurasia, significantly reducing the world’s population. COVID-19, while having caused millions of deaths globally, has a comparatively lower mortality rate and impact due to modern medical advancements and public health measures.
3.1. Historical Context of the Bubonic Plague
The bubonic plague was caused by the bacterium Yersinia pestis, transmitted by fleas living on rodents. The conditions in medieval Europe, including poor sanitation, overcrowding, and a lack of understanding of disease transmission, facilitated the rapid spread of the plague. The lack of effective treatments and the high virulence of the bacterium led to extremely high mortality rates. Symptoms included swollen lymph nodes (buboes), fever, and septicemia, often leading to death within days.
3.2. Modern Treatment and Prevention
In contrast to the bubonic plague, COVID-19 is caused by a virus and primarily spreads through respiratory droplets. Modern medicine has developed diagnostic tools, antiviral medications, and supportive care strategies to manage COVID-19. Antibiotics, which were unavailable during the bubonic plague pandemics, are highly effective in treating Yersinia pestis infections today. Improved sanitation and public health practices have also significantly reduced the risk of plague outbreaks.
3.3. Differences in Mortality Rates
The mortality rate of the bubonic plague during the Black Death was estimated to be between 30% and 60%, meaning that a large proportion of those infected died. The mortality rate of COVID-19, while varying across regions and time periods, has generally been much lower, often around 1% or less. This difference is primarily due to advancements in medical care, public health interventions, and differences in the biology of the pathogens.
3.4. Public Health Measures
Public health measures such as quarantine, isolation, and social distancing were practiced during the bubonic plague pandemics, but their effectiveness was limited due to a lack of understanding of disease transmission. In contrast, modern public health measures, including mask-wearing, hand hygiene, and vaccination campaigns, have been instrumental in controlling the spread of COVID-19.
3.5. Global Impact
While the bubonic plague significantly altered the course of human history, leading to massive social, economic, and demographic changes, the long-term impact of COVID-19 is still unfolding. The COVID-19 pandemic has disrupted global economies, healthcare systems, and daily life, but the overall mortality rate and societal impact are less severe compared to the bubonic plague. Ongoing research and vaccination efforts are crucial for mitigating the long-term effects of COVID-19.
A doctor during a plague pandemic.
4. What Lessons Can Be Learned From Comparing COVID-19 to the 1918 Flu Pandemic?
Comparing COVID-19 to the 1918 flu pandemic provides valuable lessons for pandemic preparedness, public health strategies, and societal resilience. Both pandemics caused significant global disruption, but understanding the differences in their impact and management can inform future responses.
4.1. Early Public Health Interventions
One of the key lessons from the 1918 flu pandemic is the importance of early and aggressive public health interventions. Cities that implemented measures such as school closures, bans on public gatherings, and mask mandates early in the pandemic experienced lower mortality rates. Similarly, early implementation of such measures during the COVID-19 pandemic helped to slow the spread of the virus. However, the effectiveness of these measures depends on public compliance and consistent enforcement.
4.2. The Role of Vaccines
The rapid development and deployment of COVID-19 vaccines represent a significant advancement compared to the 1918 flu pandemic, where vaccines were not available. Vaccines have proven highly effective in preventing severe disease, hospitalization, and death. The success of vaccination campaigns highlights the importance of investing in research and development of vaccines and ensuring equitable access to vaccines globally.
4.3. Healthcare Capacity and Surge Planning
Both pandemics highlighted the importance of healthcare capacity and surge planning. Overwhelmed hospitals and shortages of medical personnel and equipment can lead to increased mortality rates. Investing in healthcare infrastructure, training healthcare workers, and developing surge capacity plans are crucial for responding to future pandemics. During the COVID-19 pandemic, many countries struggled to provide adequate care due to overwhelmed healthcare systems, underscoring the need for better preparedness.
4.4. Communication and Public Trust
Effective communication and public trust are essential for implementing public health measures and ensuring public compliance. Misinformation and distrust in government and public health officials can undermine efforts to control the spread of the virus. Clear, consistent, and transparent communication is crucial for building public trust and promoting adherence to public health guidelines. The COVID-19 pandemic highlighted the challenges of combating misinformation and the importance of effective communication strategies.
4.5. Socioeconomic Impacts
Both pandemics had significant socioeconomic impacts, disproportionately affecting vulnerable populations. Addressing socioeconomic disparities and ensuring equitable access to healthcare, economic support, and social services are essential for mitigating the impact of pandemics on vulnerable communities. The COVID-19 pandemic revealed and exacerbated existing inequalities, underscoring the need for policies that promote social and economic equity.
5. How Has Globalization Affected the Spread of COVID-19 Compared to Past Pandemics?
Globalization has significantly affected the spread of COVID-19 compared to past pandemics. Increased international travel, trade, and interconnectedness have facilitated the rapid global transmission of the virus, leading to a pandemic of unprecedented scale.
5.1. Increased International Travel
The ease and frequency of international travel have played a crucial role in the rapid spread of COVID-19. In the past, pandemics were often confined to specific regions or countries due to limited travel and trade. However, with millions of people traveling internationally every day, the virus was able to spread quickly from its origin in Wuhan, China, to almost every country in the world. Travel restrictions and border closures were implemented in many countries to slow the spread of the virus, but their effectiveness was limited due to the extent of global interconnectedness.
5.2. Global Supply Chains
Global supply chains have also contributed to the spread of COVID-19. The virus was able to spread through international trade and transportation of goods. Disruptions to global supply chains also had significant economic impacts, leading to shortages of essential goods and increased prices. The pandemic highlighted the vulnerability of global supply chains to disruptions and the need for diversification and resilience.
5.3. Information Sharing and Collaboration
Globalization has also facilitated the rapid sharing of information and collaboration among scientists, researchers, and public health officials. International organizations such as the World Health Organization (WHO) played a crucial role in coordinating the global response to the pandemic, providing guidance, and facilitating the sharing of data and resources. The rapid development of COVID-19 vaccines was made possible by international collaboration and the sharing of scientific knowledge.
5.4. Social Media and Misinformation
The rise of social media has had both positive and negative effects on the spread of COVID-19. Social media platforms have facilitated the rapid dissemination of information and allowed people to stay connected during lockdowns and social distancing measures. However, social media has also been a breeding ground for misinformation and conspiracy theories, undermining public trust and hindering efforts to control the spread of the virus. Combating misinformation and promoting accurate information are crucial for managing pandemics in the age of social media.
5.5. Economic Interdependence
Economic interdependence has also influenced the spread and impact of COVID-19. The pandemic has caused significant economic disruption, leading to recessions and job losses in many countries. Governments have implemented economic stimulus measures to mitigate the impact of the pandemic, but the long-term economic consequences are still unfolding. The pandemic has highlighted the need for international cooperation to address global economic challenges.
6. How Have Hygiene Practices Impacted COVID-19 Compared to Earlier Pandemics?
Improved hygiene practices have significantly impacted the spread and severity of COVID-19 compared to earlier pandemics. Increased awareness of the importance of hand hygiene, respiratory etiquette, and environmental sanitation has helped to reduce transmission rates and protect vulnerable populations.
6.1. Hand Hygiene
Hand hygiene is one of the most effective ways to prevent the spread of respiratory infections. During the COVID-19 pandemic, public health campaigns emphasized the importance of frequent hand washing with soap and water or using hand sanitizer. Studies have shown that improved hand hygiene can reduce the transmission of respiratory viruses by up to 21%. In contrast, hygiene practices were less emphasized and less understood during earlier pandemics, such as the 1918 flu pandemic.
6.2. Respiratory Etiquette
Respiratory etiquette, including covering coughs and sneezes with a tissue or elbow, has also been promoted during the COVID-19 pandemic. This practice helps to prevent the spread of respiratory droplets containing the virus. Public health guidelines recommended wearing masks in public settings to further reduce the risk of transmission. These measures were less common or non-existent during earlier pandemics.
6.3. Environmental Sanitation
Environmental sanitation, including cleaning and disinfecting frequently touched surfaces, has also been emphasized during the COVID-19 pandemic. This practice helps to reduce the risk of transmission from contaminated surfaces. Public health guidelines recommended using disinfectants to clean surfaces such as doorknobs, countertops, and light switches. Improved sanitation practices in healthcare facilities and public spaces have also contributed to reducing the spread of the virus.
6.4. Public Awareness and Education
Increased public awareness and education about hygiene practices have played a crucial role in mitigating the spread of COVID-19. Public health campaigns have used various channels, including television, radio, social media, and print media, to promote hygiene practices and educate the public about the risks of respiratory infections. Schools, workplaces, and community organizations have also played a role in promoting hygiene practices.
6.5. Challenges and Limitations
Despite the emphasis on hygiene practices, challenges and limitations remain. Not everyone has access to clean water and soap, particularly in low-income countries. Adherence to hygiene practices can also vary depending on cultural norms and individual behaviors. Misinformation and distrust in public health officials can also undermine efforts to promote hygiene practices.
7. What Role Did Lockdown Measures Play in COVID-19 Compared to Previous Pandemics?
Lockdown measures played a significant role in controlling the spread of COVID-19, although their implementation and effectiveness varied compared to previous pandemics. Lockdowns, which involve restricting movement and closing non-essential businesses and schools, were implemented in many countries to slow transmission rates and prevent healthcare systems from being overwhelmed.
7.1. Impact on Transmission Rates
Studies have shown that lockdown measures were effective in reducing transmission rates of COVID-19. By limiting contact between people, lockdowns helped to slow the spread of the virus and reduce the number of new infections. The effectiveness of lockdowns depended on several factors, including the timing of implementation, the stringency of the measures, and public compliance.
7.2. Economic and Social Impacts
Lockdown measures had significant economic and social impacts. The closure of non-essential businesses led to job losses and economic disruption. School closures disrupted education and childcare. Social isolation and loneliness increased mental health problems. The economic and social impacts of lockdowns disproportionately affected vulnerable populations, including low-income workers, small business owners, and people with mental health conditions.
7.3. Comparisons to Previous Pandemics
Lockdown measures were less common during previous pandemics, such as the 1918 flu pandemic. In part, this was due to a lack of understanding of disease transmission and a lack of technology to support remote work and education. However, some cities and countries did implement quarantine measures and restrictions on public gatherings during previous pandemics. The scale and scope of lockdown measures during the COVID-19 pandemic were unprecedented.
7.4. Alternatives to Lockdowns
As the COVID-19 pandemic progressed, many countries explored alternatives to lockdowns, such as targeted interventions, mask mandates, and vaccination campaigns. Targeted interventions involve focusing on specific populations or settings that are at high risk of transmission. Mask mandates require people to wear masks in public settings. Vaccination campaigns aim to achieve herd immunity by vaccinating a large proportion of the population.
7.5. Ethical Considerations
Lockdown measures raised ethical considerations, including concerns about individual liberties, economic inequality, and the impact on vulnerable populations. Balancing the need to protect public health with the need to respect individual rights and freedoms was a complex challenge. Policymakers had to consider the potential harms and benefits of different interventions and make difficult decisions based on incomplete information.
8. How Did Testing Capabilities Influence COVID-19 Outcomes Compared to Earlier Pandemics?
Testing capabilities have significantly influenced COVID-19 outcomes compared to earlier pandemics. The rapid development and widespread availability of diagnostic tests for SARS-CoV-2 allowed for early detection of cases, contact tracing, and isolation of infected individuals, which helped to control the spread of the virus.
8.1. Early Detection and Isolation
Early detection of cases is crucial for preventing the spread of infectious diseases. During the COVID-19 pandemic, polymerase chain reaction (PCR) tests were used to detect the presence of the virus in respiratory samples. Rapid antigen tests were also developed, providing faster results but with lower sensitivity. Widespread testing allowed for the identification of asymptomatic cases, which played a significant role in transmission. In contrast, testing capabilities were limited or non-existent during earlier pandemics, such as the 1918 flu pandemic.
8.2. Contact Tracing
Contact tracing involves identifying and contacting individuals who may have been exposed to an infected person. This allows for the early detection of new cases and the prevention of further transmission. Contact tracing was used extensively during the COVID-19 pandemic, although its effectiveness varied depending on the availability of resources and public cooperation. Testing capabilities are essential for effective contact tracing.
8.3. Data Collection and Surveillance
Testing capabilities have also enabled the collection of data on the spread of the virus and the effectiveness of interventions. Data on case numbers, hospitalizations, and deaths were used to track the progress of the pandemic and inform public health policies. Genomic surveillance, which involves sequencing the genomes of virus samples, allowed for the identification of new variants and the monitoring of their spread.
8.4. Challenges and Limitations
Despite the advances in testing capabilities, challenges and limitations remain. Testing capacity was initially limited in many countries, leading to delays in diagnosis and contact tracing. The accuracy of tests can vary depending on the type of test and the timing of testing. False-negative results can lead to missed cases and continued transmission. The emergence of new variants can also affect the accuracy of tests.
8.5. Impact on Treatment and Outcomes
Early diagnosis through testing allowed for timely treatment of COVID-19, improving patient outcomes. Antiviral medications, such as remdesivir, and monoclonal antibodies were used to treat COVID-19, although their effectiveness varied. Testing also allowed for the identification of individuals who were at high risk of severe illness, allowing for targeted interventions and prioritization for vaccination.
9. How Did Hospital Capacity Affect COVID-19 Mortality Compared to Past Pandemics?
Hospital capacity significantly affected COVID-19 mortality compared to past pandemics. Overwhelmed healthcare systems and shortages of hospital beds, medical personnel, and equipment led to increased mortality rates during the COVID-19 pandemic.
9.1. Surge Capacity
Surge capacity refers to the ability of a healthcare system to rapidly expand its capacity to meet increased demand during a crisis. During the COVID-19 pandemic, many hospitals struggled to cope with the surge in patients, leading to shortages of beds, ventilators, and other essential resources. The lack of surge capacity resulted in delayed or inadequate care for some patients, contributing to increased mortality rates.
9.2. Medical Personnel
Shortages of medical personnel, including doctors, nurses, and respiratory therapists, also affected COVID-19 mortality. Healthcare workers were often overworked and stressed, leading to burnout and increased risk of errors. The lack of adequate staffing made it difficult to provide timely and effective care for all patients.
9.3. Comparisons to Previous Pandemics
Hospital capacity was also a limiting factor during previous pandemics, such as the 1918 flu pandemic. However, the scale and scope of the COVID-19 pandemic placed unprecedented strain on healthcare systems around the world. Advances in medical technology and treatments have improved outcomes for some patients, but these advances can be limited by a lack of hospital capacity.
9.4. Triage and Resource Allocation
In some situations, hospitals had to implement triage protocols, which involve prioritizing care for patients who are most likely to survive. This meant that some patients received less intensive care or were denied access to certain treatments. Triage decisions raised ethical concerns and highlighted the importance of ensuring adequate hospital capacity to meet the needs of all patients.
9.5. Long-Term Impacts
The COVID-19 pandemic has exposed vulnerabilities in healthcare systems around the world and highlighted the need for investments in hospital capacity, medical personnel, and public health infrastructure. Strengthening healthcare systems and improving surge capacity are essential for preparing for future pandemics and ensuring that all patients have access to timely and effective care.
10. How Has Misinformation Affected COVID-19 Outcomes Compared to Previous Pandemics?
Misinformation has significantly affected COVID-19 outcomes compared to previous pandemics. The rapid spread of false or misleading information through social media and other channels has undermined public trust, hindered efforts to control the spread of the virus, and contributed to increased morbidity and mortality.
10.1. Undermining Public Trust
Misinformation has undermined public trust in science, medicine, and public health officials. False claims about the safety and effectiveness of vaccines, the severity of the virus, and the efficacy of public health measures have led to confusion and distrust. This has made it more difficult to implement public health measures and ensure public compliance.
10.2. Hindering Public Health Efforts
Misinformation has hindered efforts to control the spread of the virus. False claims about the virus’s origins, transmission, and treatment have led people to take unnecessary risks or avoid seeking medical care. This has contributed to increased transmission rates, hospitalizations, and deaths.
10.3. Comparisons to Previous Pandemics
Misinformation has always been a challenge during pandemics, but the rise of social media has amplified its impact. In the past, false information spread more slowly and was often confined to specific communities. Today, misinformation can spread rapidly across the globe, reaching millions of people in a matter of hours. This makes it more difficult to combat misinformation and protect public health.
10.4. Impact on Vaccination Rates
Misinformation has had a particularly significant impact on vaccination rates. False claims about the safety and effectiveness of vaccines have led many people to hesitate or refuse vaccination. This has slowed the progress of vaccination campaigns and prolonged the pandemic. Combating misinformation and promoting accurate information about vaccines are essential for achieving herd immunity and protecting public health.
10.5. Strategies to Combat Misinformation
Combating misinformation requires a multi-faceted approach. This includes promoting media literacy, fact-checking, and debunking false claims. It also involves working with social media platforms to remove or flag misinformation and promote accurate information. Building public trust in science, medicine, and public health officials is also essential for countering the impact of misinformation.
For comprehensive and unbiased comparisons of health data and strategies, visit COMPARE.EDU.VN. Our platform provides detailed analyses to help you make informed decisions.
Lois Zoppi, B.A., one of the experts contributing to COMPARE.EDU.VN.
Ready to make informed decisions based on accurate comparisons? Visit COMPARE.EDU.VN today.
Compare.edu.vn
Address: 333 Comparison Plaza, Choice City, CA 90210, United States
Whatsapp: +1 (626) 555-9090
Website: COMPARE.EDU.VN
FAQ: Comparing COVID-19 to Other Pandemics
1. How does COVID-19’s mortality rate stack up against the Spanish Flu?
COVID-19 generally has a lower mortality rate compared to the Spanish Flu (1918-1920), largely due to advances in modern medicine, vaccines, and public health measures.
2. Was the Black Death deadlier than COVID-19?
Yes, the Black Death (bubonic plague) was significantly deadlier than COVID-19, with a mortality rate estimated between 30% and 60%, compared to COVID-19’s rate of around 1% or less.
3. How has globalization affected COVID-19’s spread compared to past pandemics?
Globalization has accelerated COVID-19’s spread due to increased international travel, trade, and interconnectedness, leading to a faster, wider global transmission than previous pandemics.
4. What role did hygiene practices play in mitigating COVID-19 compared to earlier outbreaks?
Improved hygiene practices like hand washing, mask-wearing, and sanitation have helped reduce COVID-19 transmission rates compared to times when such practices were less emphasized.
5. How effective were lockdown measures during COVID-19 compared to previous pandemics?
Lockdown measures were more extensive during COVID-19, aiming to slow transmission and prevent healthcare system overload, but they also had significant economic and social impacts.
6. Did testing capabilities influence COVID-19 outcomes differently than in prior pandemics?
Yes, widespread testing for COVID-19 allowed for early detection, contact tracing, and isolation, which were not possible in earlier pandemics.
7. How did hospital capacity affect COVID-19 mortality compared to past pandemics?
Overwhelmed hospital capacity during COVID-19 led to increased mortality rates, highlighting the importance of surge capacity, medical personnel, and resource allocation.
8. What impact has misinformation had on COVID-19 outcomes compared to previous pandemics?
Misinformation has significantly undermined public trust and hindered public health efforts during COVID-19, exacerbated by the rapid spread through social media.
9. What lessons can we learn by comparing COVID-19 to the 1918 Flu Pandemic?
Early public health interventions, vaccine development, healthcare capacity, communication, and addressing socioeconomic impacts are crucial lessons learned from comparing COVID-19 to the 1918 flu.
10. Are there reliable resources to compare COVID-19 with other pandemics?
Yes, compare.edu.vn provides detailed, unbiased analyses and comparisons of COVID-19 with other pandemics to help you make informed decisions.