Is COVID-19 as deadly as previous pandemics? Compare.edu.vn offers a comprehensive comparison of COVID-19 with other historical pandemics, highlighting key factors like origin, transmission, and fatality rates. Discover how COVID-19 stacks up against other outbreaks and gain insights into pandemic comparison metrics and disease severity assessments.
1. What Factors Determine the Deadliness of a Pandemic?
The deadliness of a pandemic isn’t solely determined by the virus itself; several factors interplay to influence its impact. These factors include the virus’s transmissibility, the severity of the illness it causes, the availability of effective treatments, the population’s overall health, and public health measures implemented to control its spread. Therefore, comparing the deadliness of COVID-19 to other pandemics requires a nuanced approach.
- Transmissibility: How easily the virus spreads from person to person. Highly transmissible viruses can infect a larger population, leading to a higher number of deaths, even if the case fatality rate (CFR) is low.
- Virulence: The severity of the illness caused by the virus. Highly virulent viruses can cause severe symptoms, complications, and a higher risk of death.
- Availability of Treatments: The availability of effective treatments, such as antiviral drugs and supportive care, can significantly reduce the risk of death.
- Population Health: The overall health of the population, including age, pre-existing conditions, and access to healthcare, can influence the severity of the illness and the risk of death.
- Public Health Measures: Public health measures, such as lockdowns, mask mandates, and social distancing, can help to control the spread of the virus and reduce the number of deaths.
2. How Does COVID-19 Compare to the Spanish Flu in Terms of Mortality Rate?
While the Spanish Flu of 1918 had a CFR of 2-3%, resulting in an estimated 50 million deaths, early estimates for COVID-19 suggested a lower CFR. However, the exact CFR for COVID-19 is challenging to determine due to variations in testing rates and reporting practices across different regions. Furthermore, the impact of healthcare system strain on mortality rates during COVID-19 surges must be considered.
- Spanish Flu (1918):
- Estimated Deaths: 50 million
- Case Fatality Rate (CFR): 2-3%
- COVID-19:
- Global deaths (as of late 2024): Over 7 million
- Reported CFR: Varied significantly by region and time, but generally lower than the Spanish Flu.
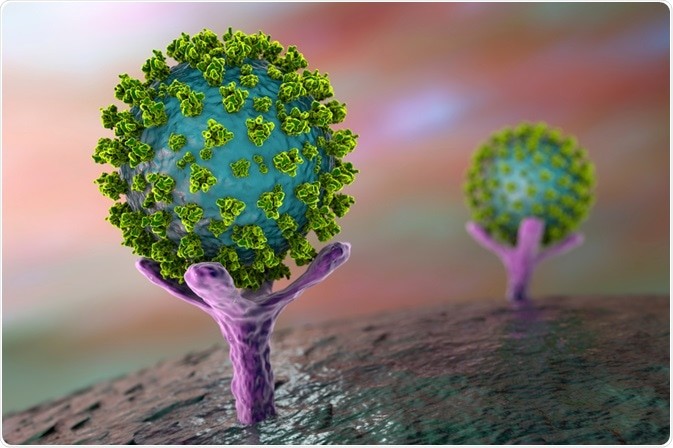
3. What Were the Origins of COVID-19, and How Did It Spread So Rapidly?
The origins of COVID-19 are traced back to Wuhan, China, with strong evidence suggesting a zoonotic origin, likely from bats, with an intermediate animal host possibly involved. The rapid global spread of COVID-19 can be attributed to several factors, including high transmissibility, asymptomatic transmission, global travel, and delayed implementation of effective public health measures.
- Zoonotic Origin: The virus likely jumped from animals to humans.
- High Transmissibility: The virus spreads easily through respiratory droplets.
- Asymptomatic Transmission: Infected individuals can spread the virus even without showing symptoms.
- Global Travel: International travel facilitated the rapid spread of the virus to almost every country.
- Delayed Public Health Measures: Delays in implementing effective public health measures, such as lockdowns and mask mandates, contributed to the rapid spread.
4. How Does the Transmission of COVID-19 Differ from Other Pandemics Like Ebola or the Bubonic Plague?
COVID-19 primarily spreads through respiratory droplets produced when an infected person coughs, sneezes, or talks. This contrasts with Ebola, which spreads through direct contact with infected bodily fluids, and the Bubonic Plague, which is transmitted through flea bites. The airborne nature of COVID-19 contributes to its higher transmissibility compared to diseases with contact-based transmission.
| Pandemic | Transmission Method |
|---|---|
| COVID-19 | Respiratory droplets |
| Ebola | Direct contact with infected bodily fluids |
| Bubonic Plague | Flea bites |

5. What Public Health Measures Were Implemented During the COVID-19 Pandemic?
A range of public health measures were implemented worldwide to mitigate the spread of COVID-19. These included lockdowns, social distancing, mask mandates, travel restrictions, enhanced hygiene practices, and vaccination campaigns. The effectiveness of these measures varied depending on the specific context and the level of adherence by the population.
- Lockdowns: Restricting movement and gatherings to reduce contact between people.
- Social Distancing: Maintaining physical distance from others to minimize the risk of transmission.
- Mask Mandates: Requiring individuals to wear masks in public settings to reduce the spread of respiratory droplets.
- Travel Restrictions: Limiting or banning travel to and from affected areas.
- Enhanced Hygiene Practices: Promoting frequent handwashing and sanitization.
- Vaccination Campaigns: Developing and distributing vaccines to provide immunity against the virus.
6. What Role Did Vaccines Play in Reducing the Severity of COVID-19?
The development and deployment of COVID-19 vaccines played a crucial role in reducing the severity of the disease. Vaccines have been shown to be highly effective in preventing severe illness, hospitalization, and death, particularly against the original strain and early variants of the virus. Widespread vaccination has significantly reduced the overall burden of COVID-19.
- Prevention of Severe Illness: Vaccines significantly reduce the risk of developing severe symptoms.
- Reduced Hospitalization: Vaccinated individuals are less likely to require hospitalization.
- Decreased Mortality: Vaccines have been proven to lower the risk of death from COVID-19.
- Protection Against Variants: While effectiveness may vary, vaccines offer protection against different variants of the virus.
- Reduced Burden on Healthcare Systems: By preventing severe cases, vaccines help to alleviate strain on healthcare systems.
7. How Did Pre-existing Conditions Affect COVID-19 Mortality Rates?
Individuals with pre-existing conditions, such as cardiovascular disease, diabetes, respiratory illnesses, and obesity, were found to be at higher risk of severe illness and death from COVID-19. These conditions can compromise the immune system and make individuals more vulnerable to the virus’s effects.
- Cardiovascular Disease: Increases the risk of severe complications and death.
- Diabetes: Impairs immune function and increases susceptibility to severe illness.
- Respiratory Illnesses: Compromise lung function and increase the risk of respiratory failure.
- Obesity: Associated with chronic inflammation and impaired immune response.
8. How Does the Availability of Healthcare Impact Pandemic Outcomes?
The availability and quality of healthcare services significantly impact pandemic outcomes. Countries with robust healthcare systems, adequate resources, and trained medical personnel are better equipped to manage surges in cases, provide timely treatment, and reduce mortality rates. Healthcare access disparities can exacerbate the impact of pandemics on vulnerable populations.
- Capacity to Manage Surges: Healthcare systems must be able to handle a sudden increase in patients.
- Timely Treatment: Prompt medical care is crucial for reducing the severity of the disease.
- Adequate Resources: Sufficient supplies of ventilators, PPE, and other medical equipment are essential.
- Trained Medical Personnel: Qualified healthcare professionals are needed to provide care and support.
- Equitable Access: Healthcare services should be accessible to all, regardless of socioeconomic status.
9. What Lessons Have Been Learned From COVID-19 That Can Help Prepare for Future Pandemics?
The COVID-19 pandemic has highlighted the importance of early detection, rapid response, robust public health infrastructure, international collaboration, and equitable access to healthcare. Investing in pandemic preparedness, strengthening healthcare systems, and promoting scientific research are crucial for mitigating the impact of future pandemics.
- Early Detection: Timely identification of outbreaks is critical for containing the spread.
- Rapid Response: Swift implementation of public health measures can help to slow transmission.
- Robust Public Health Infrastructure: Strong public health systems are essential for managing pandemics effectively.
- International Collaboration: Global cooperation is needed to share information, resources, and expertise.
- Equitable Access to Healthcare: Ensuring that everyone has access to quality medical care is crucial for reducing disparities in outcomes.
10. How Does COVID-19 Compare to MERS and SARS in Terms of Case Fatality Rate?
Compared to MERS and SARS, COVID-19 generally had a lower case fatality rate (CFR). MERS had a CFR of around 34%, SARS had a CFR of approximately 15%, while COVID-19’s CFR has varied but was often estimated to be around 1-3% early in the pandemic, although it fluctuated and differed by region. However, COVID-19’s higher transmissibility resulted in a greater number of overall deaths.
| Disease | Case Fatality Rate (CFR) |
|---|---|
| MERS | ~34% |
| SARS | ~15% |
| COVID-19 | ~1-3% (variable) |
11. What Specific Factors Made the 1918 Flu So Deadly?
Several factors contributed to the high mortality rate of the 1918 flu pandemic:
- Lack of Medical Knowledge: Limited understanding of viruses and how they spread.
- No Vaccines or Antivirals: Absence of effective medical interventions to prevent or treat the flu.
- World War I: Overcrowded conditions and troop movements facilitated the spread of the virus.
- Cytokine Storm: The virus triggered an excessive immune response (cytokine storm) in healthy young adults, leading to severe lung damage.
- Poor Sanitation: Inadequate hygiene practices contributed to the spread of the virus.
12. How Did Socioeconomic Factors Impact the Spread and Severity of COVID-19?
Socioeconomic factors played a significant role in the spread and severity of COVID-19. Lower-income communities and marginalized populations experienced higher rates of infection, hospitalization, and death due to factors such as:
- Overcrowded Housing: Increased risk of transmission in densely populated areas.
- Essential Work: Many low-income individuals were essential workers who could not work from home, increasing their exposure to the virus.
- Limited Access to Healthcare: Lack of access to affordable healthcare and testing.
- Food Insecurity: Poor nutrition can weaken the immune system and increase vulnerability to infection.
- Discrimination: Systemic inequalities and discrimination can contribute to poorer health outcomes.
13. What Strategies Proved Most Effective in Containing COVID-19?
Several strategies proved effective in containing COVID-19:
- Early and Aggressive Testing: Identifying and isolating cases early in the outbreak.
- Contact Tracing: Tracking down and quarantining individuals who had been in contact with infected persons.
- Mask Wearing: Reducing the spread of respiratory droplets.
- Social Distancing: Minimizing close contact between people.
- Vaccination: Providing immunity against the virus.
14. How Can Individuals Protect Themselves From Future Pandemics?
Individuals can take several steps to protect themselves from future pandemics:
- Practice Good Hygiene: Wash hands frequently, cover coughs and sneezes.
- Get Vaccinated: Stay up-to-date on recommended vaccinations.
- Maintain a Healthy Lifestyle: Eat a balanced diet, exercise regularly, and get enough sleep.
- Stay Informed: Follow reputable sources of information about public health recommendations.
- Advocate for Public Health Measures: Support policies that promote public health and pandemic preparedness.
15. What Global Organizations Are Involved in Pandemic Preparedness?
Several global organizations play a critical role in pandemic preparedness:
- World Health Organization (WHO): Provides global leadership on public health issues, including pandemic preparedness and response.
- Centers for Disease Control and Prevention (CDC): Conducts research and provides guidance on disease prevention and control.
- Global Fund: Invests in programs to fight AIDS, tuberculosis, and malaria, and strengthens health systems.
- Gavi, the Vaccine Alliance: Works to improve access to vaccines in low-income countries.
16. How Does Our Understanding of Viruses Impact Pandemic Response Today?
Our advanced understanding of viruses has revolutionized pandemic response:
- Rapid Identification: Quickly identifying new viruses and their characteristics.
- Diagnostic Testing: Developing accurate and rapid diagnostic tests.
- Vaccine Development: Expediting the development and production of vaccines.
- Antiviral Treatments: Creating antiviral drugs to treat viral infections.
- Epidemiological Modeling: Using data and models to predict the spread of viruses and inform public health interventions.
17. What Are the Long-Term Health Effects of COVID-19?
Many individuals who have recovered from COVID-19 experience long-term health effects, often referred to as “long COVID.” These effects can include:
- Fatigue: Persistent tiredness and lack of energy.
- Shortness of Breath: Difficulty breathing or feeling breathless.
- Cognitive Dysfunction: Problems with memory, concentration, and thinking.
- Muscle Pain: Aches and pains in the muscles and joints.
- Cardiovascular Issues: Heart palpitations, chest pain, and other heart-related problems.
18. How Did Misinformation and Disinformation Affect the COVID-19 Pandemic?
Misinformation and disinformation significantly impacted the COVID-19 pandemic by:
- Undermining Public Trust: Eroding trust in science, public health officials, and government institutions.
- Promoting False Cures: Encouraging the use of unproven and potentially harmful treatments.
- Discouraging Vaccination: Spreading false claims about vaccine safety and effectiveness.
- Fueling Conspiracy Theories: Promoting baseless and harmful conspiracy theories about the origins and nature of the virus.
- Hindering Public Health Efforts: Making it more difficult to implement effective public health measures.
19. What Are the Ethical Considerations During a Pandemic?
Pandemics raise complex ethical considerations, including:
- Resource Allocation: How to fairly distribute scarce resources, such as ventilators and vaccines.
- Individual Liberty vs. Public Health: Balancing individual freedoms with the need to protect public health.
- Privacy vs. Surveillance: Protecting privacy while using surveillance technologies to track the spread of the virus.
- Equity: Ensuring that all individuals have equal access to healthcare and other resources, regardless of socioeconomic status.
- Informed Consent: Obtaining informed consent for medical interventions, such as vaccination and treatment.
20. How Can We Improve Global Pandemic Preparedness?
To improve global pandemic preparedness, we need to:
- Invest in Public Health Infrastructure: Strengthen public health systems in all countries.
- Enhance Disease Surveillance: Improve the ability to detect and monitor emerging infectious diseases.
- Promote International Collaboration: Foster global cooperation in research, data sharing, and resource mobilization.
- Develop Rapid Response Capabilities: Establish mechanisms for quickly deploying medical personnel and resources to affected areas.
- Address Social Determinants of Health: Reduce health disparities and improve the overall health of vulnerable populations.
The COVID-19 pandemic has underscored the importance of understanding and comparing different pandemics to better prepare for future outbreaks. Factors like transmission methods, fatality rates, and the availability of vaccines all play a role in determining the severity of a pandemic. Stay informed and make informed decisions with the help of resources like COMPARE.EDU.VN.
For more comprehensive comparisons and detailed analysis, visit compare.edu.vn at 333 Comparison Plaza, Choice City, CA 90210, United States. You can also reach us via WhatsApp at +1 (626) 555-9090.
