How Addictive Is Weed Compared To Other Drugs? COMPARE.EDU.VN explores the complexities of marijuana addiction versus other substances, offering valuable insights into dependence potential and comparative harm. This comprehensive analysis examines the scientific evidence, addiction rates, and treatment approaches, helping you understand the nuances of substance dependence. Explore addiction potential, withdrawal symptoms, and dependence levels.
1. Understanding Weed Addiction
1.1. Defining Addiction
Addiction is a complex condition characterized by compulsive engagement in a behavior, despite harmful consequences. This behavior, often involving substance use, becomes central to a person’s life, overriding other priorities and responsibilities. According to the National Institute on Drug Abuse (NIDA), addiction is a chronic, relapsing brain disease.
1.2. Marijuana Use Disorder
Marijuana use disorder (MUD), as defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), involves problematic use of cannabis leading to clinically significant impairment or distress. Symptoms include using more marijuana than intended, persistent unsuccessful efforts to cut down, craving, and continued use despite negative consequences.
1.3. Prevalence of Marijuana Use Disorder
While marijuana is often perceived as less addictive than other drugs, MUD is a real and growing concern. The Substance Abuse and Mental Health Services Administration (SAMHSA) reports that millions of Americans meet the criteria for MUD each year, highlighting the importance of understanding its addictive potential. The key is to understand cannabis dependence and cannabis abuse.
2. How Addictive Is Weed Compared to Other Drugs?
2.1. Addiction Rates
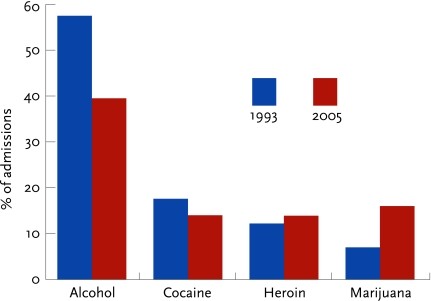
When assessing “how addictive is weed compared to other drugs”, it’s crucial to look at addiction rates. These rates show the percentage of people who try a substance and develop a dependence. According to NIDA, about 9% of marijuana users become addicted, compared to 15% for cocaine and 24% for heroin.
2.2. Comparing Addiction Potentials
| Drug | Addiction Rate (Approximate) |
|---|---|
| Marijuana | 9% |
| Alcohol | 15% |
| Cocaine | 15% |
| Heroin | 24% |
| Nicotine | 32% |
This table shows that while marijuana is less addictive than some drugs like heroin and nicotine, it is still addictive, and more so than commonly perceived. This comparison is crucial for understanding the relative dangers of substance use and informing public health strategies.
2.3. Factors Influencing Addiction Potential
Several factors influence how addictive a substance is:
-
Route of Administration: Smoking or injecting drugs leads to faster absorption and a quicker, more intense high, increasing addiction potential.
-
Frequency of Use: More frequent use increases the risk of developing dependence.
-
Potency: Higher potency substances can lead to quicker dependence.
-
Individual Vulnerability: Genetic factors, mental health conditions, and environmental factors can make some individuals more prone to addiction.
-
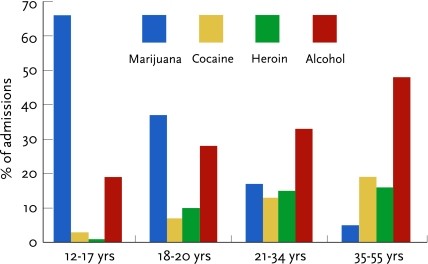
Age of First Use: Starting substance use at a younger age increases the risk of addiction.
Understanding these factors is essential in assessing the risk of addiction and tailoring prevention and treatment efforts.
3. Weed vs. Other Drugs: A Detailed Comparison
3.1. Weed vs. Alcohol
Alcohol is a legal and widely used substance with a significant addiction potential.
| Feature | Weed | Alcohol |
|---|---|---|
| Addiction Rate | ~9% | ~15% |
| Withdrawal Symptoms | Irritability, anxiety, sleep disturbances, decreased appetite, cravings | Anxiety, tremors, seizures, hallucinations, delirium tremens (DTs) |
| Health Risks | Respiratory problems, cognitive impairment, mental health issues | Liver damage, heart disease, neurological damage, increased risk of cancer |
| Social Impact | Legal restrictions in some areas, potential impact on relationships and work | Socially acceptable in many cultures, but can lead to impaired judgment, aggression, and risky behaviors |
While alcohol has a higher addiction rate, both substances pose significant health and social risks. The social acceptability of alcohol often makes it more difficult to recognize and address alcohol use disorders.
3.2. Weed vs. Cocaine
Cocaine is a powerful stimulant with a high addiction potential.
| Feature | Weed | Cocaine |
|---|---|---|
| Addiction Rate | ~9% | ~15% |
| Withdrawal Symptoms | Irritability, anxiety, sleep disturbances, decreased appetite, cravings | Depression, fatigue, increased appetite, anxiety, intense cravings |
| Health Risks | Respiratory problems, cognitive impairment, mental health issues | Heart attack, stroke, respiratory failure, nasal damage |
| Social Impact | Legal restrictions, potential impact on relationships and work | Illegal, significant impact on relationships, financial problems, involvement in criminal activity |
Cocaine’s intense euphoric effects and severe withdrawal symptoms contribute to its high addiction rate. The cardiovascular risks associated with cocaine use are particularly dangerous.
3.3. Weed vs. Heroin
Heroin is an opioid drug with a very high addiction potential.
| Feature | Weed | Heroin |
|---|---|---|
| Addiction Rate | ~9% | ~24% |
| Withdrawal Symptoms | Irritability, anxiety, sleep disturbances, decreased appetite, cravings | Muscle aches, nausea, vomiting, diarrhea, intense cravings |
| Health Risks | Respiratory problems, cognitive impairment, mental health issues | Respiratory depression, overdose, infectious diseases (HIV, hepatitis) |
| Social Impact | Legal restrictions, potential impact on relationships and work | Illegal, significant impact on relationships, financial problems, involvement in criminal activity |
Heroin’s powerful euphoric effects and severe withdrawal symptoms make it one of the most addictive drugs. The risk of overdose and infectious diseases associated with heroin use are significant public health concerns.
3.4. Weed vs. Nicotine
Nicotine, found in tobacco products, is one of the most addictive substances.
| Feature | Weed | Nicotine |
|---|---|---|
| Addiction Rate | ~9% | ~32% |
| Withdrawal Symptoms | Irritability, anxiety, sleep disturbances, decreased appetite, cravings | Irritability, anxiety, difficulty concentrating, increased appetite, cravings |
| Health Risks | Respiratory problems, cognitive impairment, mental health issues | Lung cancer, heart disease, respiratory diseases |
| Social Impact | Legal restrictions, potential impact on relationships and work | Socially acceptable in many contexts but increasingly restricted, significant health costs |
Nicotine’s high addiction rate is due to its rapid effects on the brain and the strong association with social routines. The long-term health risks of nicotine use, particularly lung cancer and heart disease, are well-documented.
4. The Science Behind Weed Addiction
4.1. The Endocannabinoid System
The endocannabinoid system (ECS) plays a crucial role in marijuana addiction. THC, the primary psychoactive compound in marijuana, binds to cannabinoid receptors in the brain, disrupting normal ECS function. This disruption can lead to dependence and withdrawal symptoms upon cessation.
4.2. Dopamine and Reward Pathways
Like other addictive drugs, marijuana affects dopamine levels in the brain’s reward pathways. Chronic marijuana use can lead to reduced sensitivity in these pathways, requiring more of the drug to achieve the same euphoric effects. This contributes to the development of tolerance and dependence.
4.3. Genetic and Environmental Factors
Genetic factors can influence an individual’s susceptibility to marijuana addiction. Environmental factors, such as exposure to drug use in the home or peer pressure, can also increase the risk. Understanding these factors can help identify individuals at higher risk and tailor prevention efforts accordingly.
5. Recognizing Marijuana Use Disorder
5.1. Symptoms of MUD
Recognizing the symptoms of marijuana use disorder is the first step in addressing the problem:
- Using more marijuana than intended
- Persistent unsuccessful efforts to cut down
- Craving marijuana
- Continued use despite negative consequences
- Tolerance
- Withdrawal symptoms upon cessation
5.2. Diagnostic Criteria
The DSM-5 outlines specific criteria for diagnosing MUD. Meeting two or more of these criteria within a 12-month period indicates the presence of a marijuana use disorder. Seeking professional evaluation is essential for accurate diagnosis and appropriate treatment planning.
5.3. Screening Tools
Several screening tools can help identify potential marijuana use disorders. These tools, such as the Cannabis Abuse Screening Test (CAST) and the Marijuana Use Disorder Identification Test (MUDIT), can be administered by healthcare professionals or used for self-assessment.
6. Marijuana Withdrawal Syndrome
6.1. Symptoms of Withdrawal
Marijuana withdrawal syndrome is characterized by a range of physical and psychological symptoms:
- Irritability
- Anxiety
- Sleep disturbances
- Decreased appetite
- Craving
- Restlessness
- Depression
6.2. Severity and Duration
The severity and duration of marijuana withdrawal symptoms vary depending on the individual and the extent of their marijuana use. Symptoms typically begin within 24 to 48 hours of abstinence, peak within 4 to 6 days, and last from 1 to 3 weeks.
6.3. Managing Withdrawal Symptoms
Managing marijuana withdrawal symptoms often involves supportive care:
- Hydration: Drinking plenty of fluids can help alleviate some physical symptoms.
- Nutrition: Eating a balanced diet can improve energy levels and mood.
- Exercise: Regular physical activity can reduce anxiety and improve sleep.
- Counseling: Therapy can help individuals cope with cravings and emotional symptoms.
In some cases, medications may be prescribed to manage specific symptoms, such as sleep disturbances or anxiety.
7. Treatment Options for Marijuana Addiction
7.1. Behavioral Therapies
Behavioral therapies are a cornerstone of marijuana addiction treatment:
- Cognitive Behavioral Therapy (CBT): CBT helps individuals identify and change negative thought patterns and behaviors associated with marijuana use.
- Motivational Enhancement Therapy (MET): MET focuses on increasing an individual’s motivation to change their marijuana use.
- Contingency Management (CM): CM involves providing rewards for achieving specific goals, such as abstinence from marijuana.
7.2. Support Groups
Support groups provide a safe and supportive environment for individuals to share their experiences and learn from others. Marijuana Anonymous (MA) is a 12-step program similar to Alcoholics Anonymous, offering peer support for individuals recovering from marijuana addiction.
7.3. Medication-Assisted Treatment (MAT)
While there are currently no FDA-approved medications specifically for marijuana addiction, some medications may be used to manage withdrawal symptoms or co-occurring mental health conditions. Research is ongoing to identify potential pharmacotherapies for marijuana addiction.
8. Addressing Co-Occurring Disorders
8.1. Mental Health Conditions
Marijuana addiction often co-occurs with mental health conditions such as anxiety, depression, and PTSD. Addressing these co-occurring disorders is essential for successful treatment outcomes. Integrated treatment approaches that address both the addiction and the mental health condition simultaneously are often the most effective.
8.2. Polysubstance Abuse
Many individuals with marijuana addiction also use other substances. Addressing polysubstance abuse requires a comprehensive treatment plan that targets all substances involved. This may involve detoxification, behavioral therapies, and medication-assisted treatment.
8.3. Trauma-Informed Care
Trauma can play a significant role in the development of addiction. Trauma-informed care recognizes the impact of trauma on an individual’s life and incorporates this understanding into treatment. This approach emphasizes safety, trust, and empowerment.
9. Prevention Strategies
9.1. Education Programs
Education programs are crucial for preventing marijuana addiction:
- School-Based Programs: Providing accurate information about the risks of marijuana use in schools can help prevent early initiation.
- Community Outreach: Reaching out to communities with education programs can raise awareness and reduce stigma associated with addiction.
- Parent Education: Educating parents about the signs of marijuana use and effective communication strategies can help prevent adolescent marijuana use.
9.2. Early Intervention
Early intervention programs can help identify individuals at risk of developing marijuana addiction and provide support and resources. These programs may involve screening, brief interventions, and referrals to treatment.
9.3. Policy and Regulation
Policies and regulations regarding marijuana use can also play a role in prevention. These may include restrictions on advertising, age limits for purchase, and regulations on potency.
10. Legalization and Addiction
10.1. Impact of Legalization
The legalization of marijuana has led to increased access and normalization of its use. While some argue that legalization reduces crime and generates tax revenue, others raise concerns about potential increases in addiction rates and associated health and social consequences.
10.2. Public Health Concerns
Public health concerns related to marijuana legalization include:
- Increased rates of marijuana use disorders
- Increased rates of impaired driving
- Increased access for adolescents
- Potential for increased rates of psychosis and other mental health conditions
Addressing these concerns requires comprehensive public health strategies, including education, prevention, and treatment.
10.3. Responsible Regulation
Responsible regulation of marijuana can help minimize potential harms:
- Age Limits: Restricting purchase and use to adults over the age of 21.
- Advertising Restrictions: Limiting advertising to prevent normalization of marijuana use among adolescents.
- Potency Limits: Regulating the potency of marijuana products to reduce the risk of addiction and adverse health effects.
- Taxation: Using tax revenue to fund education, prevention, and treatment programs.
11. Current Research and Future Directions
11.1. Ongoing Studies
Ongoing research is essential for improving our understanding of marijuana addiction and developing more effective treatments. Current studies are exploring:
- The neurobiological mechanisms of marijuana addiction
- The effectiveness of different treatment approaches
- The long-term effects of marijuana use
- The impact of marijuana legalization on public health
11.2. Potential Pharmacotherapies
Research is ongoing to identify potential pharmacotherapies for marijuana addiction. This includes:
- Developing medications to manage withdrawal symptoms
- Developing medications to reduce cravings
- Developing medications to block the effects of THC
11.3. Personalized Treatment Approaches
Personalized treatment approaches that tailor interventions to individual needs and characteristics hold promise for improving outcomes. This may involve using genetic information, brain imaging, or other biomarkers to guide treatment decisions.
12. Seeking Help
12.1. Finding Treatment Centers
Finding a qualified treatment center is a crucial step in addressing marijuana addiction. Resources such as the SAMHSA Behavioral Health Treatment Services Locator can help individuals find treatment centers in their area.
12.2. Talking to a Healthcare Professional
Talking to a healthcare professional is essential for accurate diagnosis and appropriate treatment planning. Healthcare professionals can provide guidance, support, and referrals to specialized treatment services.
12.3. Supporting Loved Ones
Supporting loved ones struggling with marijuana addiction can be challenging. Education, empathy, and clear communication are essential. Encouraging loved ones to seek professional help and providing ongoing support can make a significant difference.
13. Conclusion
Understanding “how addictive is weed compared to other drugs” requires a nuanced approach. While marijuana may be less addictive than substances like heroin or nicotine, it still carries a risk of dependence and can lead to significant health and social consequences. Awareness, prevention, and effective treatment strategies are essential for addressing marijuana addiction and promoting public health. Whether you’re comparing addiction, abuse or dependence, COMPARE.EDU.VN, can assist in comparing facts objectively.
14. COMPARE.EDU.VN: Your Source for Objective Comparisons
At COMPARE.EDU.VN, we understand the importance of making informed decisions based on accurate and objective information. Our platform is designed to provide you with comprehensive comparisons across a wide range of topics, from educational resources to consumer products. We are committed to helping you navigate the complexities of various choices and empowering you to make the best decisions for your needs. We deliver details, ratings and reviews.
15. Call to Action
Are you looking for objective comparisons to help you make informed decisions? Visit COMPARE.EDU.VN today to explore our comprehensive resources and discover the information you need to make the right choices. Don’t navigate the complexities alone – let COMPARE.EDU.VN empower you with knowledge and clarity. COMPARE.EDU.VN – Empowering decisions through detailed comparisons. For assistance, contact us at 333 Comparison Plaza, Choice City, CA 90210, United States, Whatsapp: +1 (626) 555-9090.
16. Frequently Asked Questions (FAQ)
16.1. Is marijuana addictive?
Yes, marijuana can be addictive. About 9% of marijuana users develop a marijuana use disorder.
16.2. What are the symptoms of marijuana withdrawal?
Symptoms include irritability, anxiety, sleep disturbances, decreased appetite, and cravings.
16.3. How does marijuana addiction compare to other drugs?
Marijuana is generally less addictive than drugs like heroin, cocaine, and nicotine but more addictive than some perceive.
16.4. What are the treatment options for marijuana addiction?
Treatment options include behavioral therapies, support groups, and medication-assisted treatment.
16.5. Can marijuana addiction co-occur with other disorders?
Yes, marijuana addiction often co-occurs with mental health conditions and polysubstance abuse.
16.6. How does marijuana affect the brain?
Marijuana affects the endocannabinoid system and dopamine levels in the brain, leading to dependence.
16.7. What is the impact of marijuana legalization on addiction?
Legalization has led to increased access and normalization of marijuana use, raising concerns about potential increases in addiction rates.
16.8. What can parents do to prevent marijuana use among adolescents?
Parents can educate themselves about the signs of marijuana use, communicate effectively with their children, and support early intervention programs.
16.9. Are there medications for marijuana addiction?
Currently, there are no FDA-approved medications specifically for marijuana addiction, but some medications may be used to manage withdrawal symptoms or co-occurring mental health conditions.
16.10. Where can I find more information about marijuana addiction?
You can find more information on websites like compare.edu.vn, the National Institute on Drug Abuse (NIDA), and the Substance Abuse and Mental Health Services Administration (SAMHSA).
