Has behavioral addiction been compared to chemical dependency by some psychologists? Yes, behavioral addiction Has Been Compared To Chemical Dependency By Some Psychologists, highlighting the overlapping diagnostic symptoms. At COMPARE.EDU.VN, we delve into the similarities and differences between these conditions, offering a comprehensive understanding. Exploring addiction spectrum, compulsion loop, and reward system, our analysis provides clarity and insight.
1. Understanding Behavioral Addiction and Chemical Dependency
1.1 What is Behavioral Addiction?
Behavioral addiction refers to a compulsive engagement in non-substance-related behaviors, despite negative consequences. Psychologists have increasingly compared it to chemical dependency due to observed similarities in symptoms and neurological pathways. These behaviors can include gambling, excessive internet use, gaming, shopping, eating, and even work. The key characteristic is the individual’s inability to control the behavior, leading to distress and impairment in various life domains.
 Diagnostic criteria for behavioral addictions
Diagnostic criteria for behavioral addictions
1.2 What is Chemical Dependency?
Chemical dependency, also known as substance use disorder, involves the compulsive use of drugs or alcohol despite harmful consequences. It is characterized by physical and psychological dependence, tolerance, withdrawal symptoms, and a strong craving for the substance. The impact of chemical dependency extends to various aspects of life, including physical health, mental well-being, relationships, and occupational functioning.
1.3 How Do Psychologists Compare These Two?
Psychologists compare behavioral addiction to chemical dependency by examining shared diagnostic criteria, neurobiological mechanisms, and psychological processes. Both types of addiction involve:
- Compulsive Behavior: An overwhelming urge to engage in the behavior or use the substance.
- Loss of Control: Inability to regulate or stop the behavior despite attempts to do so.
- Tolerance: The need to increase the intensity or frequency of the behavior or substance use to achieve the desired effect.
- Withdrawal Symptoms: Experiencing physical or psychological symptoms when the behavior or substance use is reduced or stopped.
- Continued Use Despite Consequences: Persisting with the behavior or substance use despite awareness of negative consequences.
- Craving: Intense desire or urge to engage in the behavior or use the substance.
2. Diagnostic Criteria for Behavioral Addictions
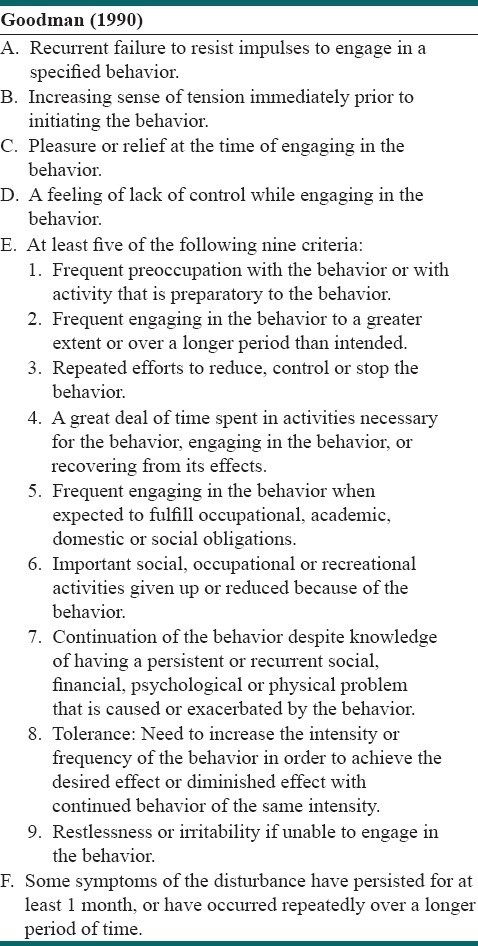
2.1 Goodman’s Criteria for Behavioral Addictions
Goodman’s criteria, outlined in Table 1, offer a structured approach to diagnosing behavioral addictions. These criteria help clinicians assess the severity and impact of the addictive behavior on an individual’s life.
Table 1: Goodman’s Diagnostic Criteria for Behavioral Addictions
| Criterion | Description |
|---|---|
| Preoccupation | A frequent and intense focus on the behavior, often dominating thoughts and planning. |
| Mood Modification | Engaging in the behavior to experience a change in mood, such as feeling pleasure, relief, or escape from negative emotions. |
| Tolerance | The need to increase the intensity or frequency of the behavior to achieve the desired mood-altering effect. |
| Withdrawal Symptoms | Experiencing negative physical or emotional symptoms when the behavior is reduced or stopped, such as irritability, anxiety, or restlessness. |
| Loss of Control | Inability to regulate or stop the behavior despite attempts to do so, often leading to engaging in the behavior more often or for longer periods than intended. |
| Conflict | Experiencing difficulties in relationships, work, or other important areas of life as a result of the behavior, often leading to feelings of guilt, shame, or regret. |
| Relapse | A tendency to return to the addictive behavior after periods of abstinence or control, often triggered by stress, cues, or environmental factors. |
2.2 Griffiths’ Criteria for Behavioral Addiction
Griffiths’ criteria, shown in Table 2, provide another framework for understanding and diagnosing behavioral addictions, emphasizing the psychological and behavioral aspects of the addiction.
Table 2: Griffiths’ Diagnostic Criteria for Behavioral Addiction
| Criterion | Description |
|---|---|
| Salience | The behavior becomes the most important activity in the person’s life, dominating their thoughts, feelings, and behavior. |
| Mood Modification | Engaging in the behavior leads to a subjective experience of feeling better or different, such as excitement, pleasure, or relief. |
| Tolerance | The need to increase the amount of the behavior to achieve the same mood-modifying effects as before. |
| Withdrawal Symptoms | Experiencing unpleasant feelings or physical effects when the behavior is discontinued or reduced. |
| Conflict | The behavior leads to conflicts with oneself (intrapsychic) or with others (interpersonal), such as arguments, dishonesty, or neglecting responsibilities. |
| Relapse | A tendency to repeatedly return to the behavior after attempts to stop or control it. |
3. Commonalities Between Behavioral and Chemical Addictions
3.1 Psychological Components
Both behavioral and chemical addictions share similar psychological components, including:
- Reinforcement: The behavior or substance use is initially rewarding, leading to repeated engagement.
- Compulsion: The urge to engage in the behavior or use the substance becomes overwhelming and difficult to resist.
- Craving: Intense desire or urge to engage in the behavior or use the substance, especially in response to cues or triggers.
- Loss of Control: Inability to regulate or stop the behavior or substance use despite attempts to do so.
- Negative Consequences: Experiencing adverse effects on physical health, mental well-being, relationships, and occupational functioning.
3.2 Neurobiological Similarities
Research indicates that both behavioral and chemical addictions affect similar brain regions and neurotransmitter systems, including:
- Reward System: The mesolimbic dopamine pathway is activated in both types of addiction, leading to feelings of pleasure and reinforcement.
- Prefrontal Cortex: The prefrontal cortex, responsible for executive functions such as decision-making and impulse control, is impaired in both types of addiction.
- Amygdala: The amygdala, involved in emotional processing, is implicated in the development of cravings and withdrawal symptoms in both types of addiction.
3.3 Risk Factors
Common risk factors contribute to the development of both behavioral and chemical addictions, including:
- Genetic Predisposition: Family history of addiction increases the risk of developing both types of addiction.
- Environmental Factors: Exposure to addictive behaviors or substances, as well as social and cultural norms, can influence the likelihood of developing addiction.
- Psychological Factors: Mental health conditions such as depression, anxiety, and trauma can increase the risk of developing addiction.
- Age of Onset: Starting addictive behaviors or substance use at a young age can increase the risk of developing addiction later in life.
4. Differences Between Behavioral and Chemical Addictions
4.1 Physical vs. Psychological Dependence
One key difference between behavioral and chemical addictions is the presence of physical dependence in chemical addictions. Physical dependence occurs when the body adapts to the presence of a substance, leading to withdrawal symptoms when the substance is reduced or stopped. Behavioral addictions primarily involve psychological dependence, characterized by emotional and mental reliance on the behavior.
4.2 Observable Signs
Chemical addictions often have more visible physical signs, such as changes in appearance, coordination, and vital signs. Behavioral addictions may be less apparent, with symptoms primarily manifesting as changes in behavior, mood, and social interactions.
4.3 Treatment Approaches
While some treatment approaches are similar for both types of addiction, such as cognitive-behavioral therapy (CBT) and support groups, chemical addictions often require medical interventions such as detoxification and medication-assisted treatment (MAT) to manage withdrawal symptoms and prevent relapse.
5. The Role of Neurotransmitters
5.1 Dopamine’s Role in Addiction
Dopamine, a neurotransmitter involved in reward and motivation, plays a crucial role in both behavioral and chemical addictions. Addictive behaviors and substances increase dopamine levels in the brain, leading to feelings of pleasure and reinforcement. Over time, the brain adapts to these elevated dopamine levels, leading to tolerance and the need for increased stimulation to achieve the same effect.
5.2 Other Neurotransmitters Involved
In addition to dopamine, other neurotransmitters such as serotonin, norepinephrine, and GABA are also implicated in addiction. These neurotransmitters play roles in mood regulation, stress response, and impulse control, and their dysregulation can contribute to the development and maintenance of addiction.
6. Co-occurring Disorders
6.1 Mental Health Conditions
Individuals with behavioral or chemical addictions often have co-occurring mental health conditions, such as depression, anxiety, ADHD, and trauma. These co-occurring disorders can complicate the treatment process and increase the risk of relapse. Addressing both the addiction and the underlying mental health condition is essential for successful recovery.
6.2 Substance Use Disorders
It is not uncommon for individuals with behavioral addictions to also have substance use disorders, and vice versa. The presence of both types of addiction can exacerbate the symptoms and consequences of each, making treatment more challenging. Integrated treatment approaches that address both addictions simultaneously are often the most effective.
7. Treatment Options
7.1 Cognitive-Behavioral Therapy (CBT)
Cognitive-behavioral therapy (CBT) is a widely used treatment approach for both behavioral and chemical addictions. CBT helps individuals identify and change negative thought patterns and behaviors that contribute to their addiction. Techniques used in CBT include cognitive restructuring, relapse prevention, and skills training.
7.2 Support Groups
Support groups, such as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA), provide a supportive and understanding environment for individuals recovering from addiction. Support groups offer peer support, encouragement, and guidance, and can help individuals develop coping skills and maintain sobriety.
7.3 Medication-Assisted Treatment (MAT)
Medication-assisted treatment (MAT) involves the use of medications, in combination with counseling and behavioral therapies, to treat substance use disorders. MAT can help reduce cravings, manage withdrawal symptoms, and prevent relapse. Medications used in MAT include methadone, buprenorphine, and naltrexone.
7.4 Lifestyle Changes
Making positive lifestyle changes, such as engaging in regular exercise, practicing mindfulness, and improving sleep hygiene, can also support recovery from addiction. These lifestyle changes can help reduce stress, improve mood, and enhance overall well-being.
8. Prevention Strategies
8.1 Education and Awareness
Education and awareness campaigns can help prevent the development of both behavioral and chemical addictions. These campaigns can educate individuals about the risks and consequences of addiction, as well as promote healthy coping strategies and lifestyle choices.
8.2 Early Intervention
Early intervention programs can help identify individuals at risk of developing addiction and provide them with support and resources to prevent the problem from escalating. These programs may involve screening, assessment, and brief interventions.
8.3 Promoting Healthy Alternatives
Promoting healthy alternatives to addictive behaviors and substances, such as engaging in hobbies, spending time with loved ones, and volunteering, can help reduce the risk of addiction. These activities can provide individuals with a sense of purpose, fulfillment, and connection.
9. Societal Impact
9.1 Economic Costs
Both behavioral and chemical addictions have significant economic costs, including healthcare expenses, lost productivity, and criminal justice costs. Investing in prevention and treatment programs can help reduce these economic costs and improve the overall health and well-being of society.
9.2 Social Consequences
Addiction can have devastating social consequences, including broken relationships, family dysfunction, and social isolation. Addressing addiction requires a comprehensive approach that involves individuals, families, communities, and policymakers.
10. Research and Future Directions
10.1 Advancements in Neuroscience
Advancements in neuroscience are providing new insights into the neurobiological mechanisms underlying addiction. These insights may lead to the development of more effective treatments and prevention strategies.
10.2 Personalized Treatment Approaches
Personalized treatment approaches that take into account individual differences in genetics, environment, and psychological factors may improve treatment outcomes. Research is needed to identify biomarkers and predictors of treatment response to guide personalized treatment planning.
11. Expert Opinions on the Comparison
11.1 Views of Leading Psychologists
Leading psychologists and addiction specialists have weighed in on the comparison between behavioral and chemical addictions, highlighting the importance of recognizing the similarities and differences between these conditions. Many experts argue that behavioral addictions should be recognized as legitimate mental health disorders, deserving of the same level of attention and resources as chemical addictions.
11.2 Case Studies and Examples
Numerous case studies and real-life examples illustrate the parallels between behavioral and chemical addictions. These examples demonstrate how individuals can develop compulsive engagement in behaviors such as gambling, gaming, or internet use, leading to similar consequences as those experienced by individuals with substance use disorders.
12. Overcoming Stigma
12.1 Addressing Misconceptions
One of the biggest challenges in addressing addiction is overcoming stigma and misconceptions. Many people view addiction as a moral failing or a lack of willpower, rather than a complex mental health disorder. Addressing these misconceptions through education and awareness campaigns can help reduce stigma and promote empathy and understanding.
12.2 Promoting Empathy and Understanding
Promoting empathy and understanding towards individuals struggling with addiction can help create a more supportive and compassionate society. Sharing personal stories and experiences can help humanize addiction and break down stereotypes.
13. Finding Support and Resources
13.1 Online Resources
Numerous online resources are available to individuals seeking support and information about addiction, including websites, forums, and online support groups. These resources can provide individuals with access to education, counseling, and peer support.
13.2 Local Support Groups
Local support groups, such as AA and NA, offer in-person support and connection for individuals recovering from addiction. These groups provide a safe and confidential environment for individuals to share their experiences and receive encouragement from others.
14. The Future of Addiction Treatment
14.1 Integration of Technology
The integration of technology into addiction treatment is transforming the way care is delivered. Telehealth, mobile apps, and wearable sensors are being used to provide remote monitoring, counseling, and support to individuals recovering from addiction.
14.2 Holistic Approaches
Holistic approaches to addiction treatment that address the physical, mental, and spiritual aspects of well-being are gaining popularity. These approaches may include mindfulness practices, yoga, acupuncture, and nutritional therapy.
15. Conclusion: A Balanced Perspective
15.1 Key Takeaways
In conclusion, behavioral addiction has been compared to chemical dependency by some psychologists due to overlapping diagnostic symptoms, neurobiological mechanisms, and psychological processes. While there are differences between the two types of addiction, recognizing the similarities can help improve prevention, treatment, and support efforts.
15.2 Final Thoughts
Understanding the complexities of addiction requires a balanced perspective that takes into account both the individual and societal factors that contribute to the problem. By promoting education, awareness, and empathy, we can create a more supportive and compassionate society for individuals struggling with addiction.
Are you grappling with making an informed decision amidst a sea of comparisons? At COMPARE.EDU.VN, we provide detailed and objective comparisons across diverse products, services, and ideas. We meticulously highlight pros and cons, analyze features, and present user reviews to simplify your decision-making process. Discover informed choices and confidently select what best fits your needs with us.
FAQ: Understanding Behavioral Addiction
1. What exactly is behavioral addiction?
Behavioral addiction involves compulsive engagement in activities like gambling, gaming, or internet use, mirroring substance addiction symptoms without substance use.
2. How does behavioral addiction affect the brain?
Similar to chemical dependency, behavioral addiction affects the brain’s reward system, releasing dopamine during the addictive behavior.
3. Can behavioral addictions be treated?
Yes, treatment options include cognitive-behavioral therapy (CBT), support groups, and lifestyle changes to manage and overcome behavioral addictions.
4. What are the risk factors for behavioral addiction?
Risk factors include genetic predisposition, environmental factors, psychological issues like depression or anxiety, and early exposure to addictive behaviors.
5. Is there a difference between habit and behavioral addiction?
Yes, a habit is a routine behavior, while behavioral addiction involves compulsion, loss of control, and negative consequences despite attempts to stop.
6. How do I know if I have a behavioral addiction?
Signs include preoccupation with the behavior, mood modification, tolerance, withdrawal symptoms, conflict in relationships, and relapse despite efforts to quit.
7. What is the role of dopamine in behavioral addiction?
Dopamine, a neurotransmitter involved in reward, is released during addictive behaviors, reinforcing the behavior and leading to compulsive engagement.
8. Can medication help treat behavioral addiction?
While not as common as in chemical dependency, some medications may help manage co-occurring mental health conditions and reduce cravings associated with behavioral addictions.
9. Are behavioral addictions recognized as mental health disorders?
Yes, many experts recognize behavioral addictions as legitimate mental health disorders, deserving attention and resources similar to chemical addictions.
10. Where can I find support for behavioral addiction?
Support is available through online resources, local support groups, counseling, and therapy to address the underlying issues and develop coping strategies.
Ready to make smarter choices? Visit COMPARE.EDU.VN today to explore our comprehensive comparison articles and discover the information you need to make confident decisions.
Contact Us:
- Address: 333 Comparison Plaza, Choice City, CA 90210, United States
- WhatsApp: +1 (626) 555-9090
- Website: compare.edu.vn
