Does PCI reduce mortality in diabetic patients compared with medical therapy? Percutaneous coronary intervention (PCI) is a common procedure, but its effectiveness in reducing mortality for diabetic patients compared to medical therapy has been a topic of debate, which COMPARE.EDU.VN will shed light on. Understanding the nuances of these approaches is crucial for informed decision-making. Optimize medical treatment, coronary revascularization, and appropriate revascularization strategies.
1. What is Percutaneous Coronary Intervention (PCI) and How Does it Work?
Percutaneous coronary intervention (PCI) is a minimally invasive procedure used to open blocked or narrowed coronary arteries, improving blood flow to the heart. A catheter with a balloon on the end is inserted into an artery (usually in the groin or wrist) and guided to the blocked artery in the heart. The balloon is then inflated to compress the plaque against the artery walls, widening the artery. A stent, which is a small mesh tube, is often placed in the artery to help keep it open. PCI aims to alleviate symptoms like chest pain (angina) and reduce the risk of heart attack. This interventional cardiology technique can significantly improve quality of life.
2. What is Optimal Medical Therapy (OMT) for Diabetic Patients with CAD?
Optimal Medical Therapy (OMT) for diabetic patients with coronary artery disease (CAD) involves a comprehensive approach to managing risk factors and symptoms. OMT typically includes medications such as:
- Antiplatelet drugs: Aspirin or clopidogrel to prevent blood clots.
- Statins: To lower cholesterol levels.
- ACE inhibitors or ARBs: To control blood pressure and protect the kidneys.
- Beta-blockers: To reduce heart rate and blood pressure.
- Nitrates: To relieve angina symptoms.
- Diabetes medications: To control blood sugar levels.
Lifestyle modifications, such as diet, exercise, and smoking cessation, are also crucial components of OMT. The goal of OMT is to stabilize the disease, reduce symptoms, and prevent future cardiovascular events. Glycemic control is a central element of this strategy.
3. What Do Studies Say About PCI vs. OMT for Diabetic Patients?
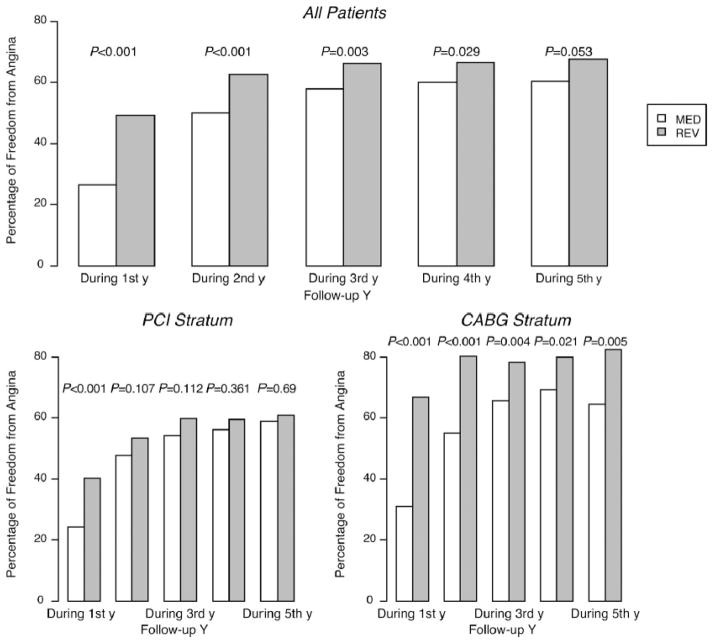
Studies comparing PCI and OMT for diabetic patients with CAD have shown mixed results. Some studies suggest that PCI may provide better symptom relief and reduce the need for further interventions compared to OMT alone. However, other studies have not found a significant difference in mortality rates between the two approaches. The BARI 2D trial, for example, found no significant difference in mortality between PCI and OMT in stable CAD patients with diabetes, although CABG (coronary artery bypass grafting) showed some benefits. The FREEDOM trial indicated that CABG was superior to PCI in reducing mortality and myocardial infarction in diabetic patients with multivessel CAD.
4. Does PCI Reduce Mortality in Diabetic Patients Compared to Medical Therapy?
Whether PCI reduces mortality in diabetic patients compared to medical therapy is a complex question without a definitive answer suitable for all patients. Some studies have shown no significant difference in mortality between PCI and OMT in patients with stable CAD. For instance, the BARI 2D trial did not find a statistically significant difference in overall survival between patients treated with PCI or CABG plus OMT versus those treated with OMT alone. However, other trials, such as the FREEDOM trial, demonstrated that CABG significantly reduced mortality compared to PCI in diabetic patients with multivessel coronary artery disease. The decision on whether to pursue PCI should be individualized, considering the severity of CAD, the presence of symptoms, and other patient-specific factors.
5. What Factors Influence the Choice Between PCI and OMT for Diabetic Patients?
Several factors influence the choice between PCI and OMT for diabetic patients with CAD:
- Severity of CAD: Patients with severe multivessel disease or left main coronary artery disease may benefit more from CABG than PCI.
- Symptoms: Patients with persistent angina despite OMT may be candidates for PCI or CABG.
- Patient preference: Shared decision-making is essential, considering the patient’s values and preferences.
- Comorbidities: Other health conditions, such as kidney disease or heart failure, can influence the choice of treatment.
- Risk of complications: The risk of complications from PCI or CABG should be weighed against the potential benefits.
- Diabetes control: Well-managed diabetes is crucial for better outcomes with either PCI or OMT.
6. What Are the Risks and Benefits of PCI for Diabetic Patients?
The risks of PCI for diabetic patients include bleeding, infection, blood vessel damage, and allergic reactions to contrast dye. Stent thrombosis, a rare but serious complication, can also occur. The benefits of PCI include improved blood flow to the heart, relief from angina symptoms, and a reduced risk of heart attack. However, PCI may not always be effective in preventing future cardiovascular events, and repeat procedures may be necessary. Dual antiplatelet therapy (DAPT) is often required after PCI to prevent stent thrombosis, which can increase the risk of bleeding.
7. What Are the Risks and Benefits of OMT for Diabetic Patients?
The risks of OMT for diabetic patients are generally low, but side effects from medications can occur. Statins, for example, can cause muscle pain or liver problems. ACE inhibitors can cause cough or kidney problems. The benefits of OMT include a reduced risk of cardiovascular events, improved blood sugar control, and better management of other risk factors like high blood pressure and high cholesterol. OMT is a long-term strategy that requires adherence to medications and lifestyle modifications.
8. How Does Diabetes Affect Outcomes After PCI?
Diabetes can negatively affect outcomes after PCI. Diabetic patients are at higher risk of restenosis (re-narrowing of the artery after PCI) and stent thrombosis. They also tend to have more diffuse and complex CAD, making PCI more challenging. Poor glycemic control can increase the risk of complications after PCI. However, with the use of drug-eluting stents (DES) and aggressive medical management, outcomes after PCI in diabetic patients have improved over time.
9. What is the Role of Drug-Eluting Stents (DES) in PCI for Diabetic Patients?
Drug-eluting stents (DES) have significantly improved outcomes after PCI in diabetic patients. DES are coated with medication that is slowly released to prevent the growth of scar tissue and reduce the risk of restenosis. Studies have shown that DES are more effective than bare-metal stents (BMS) in reducing the need for repeat procedures in diabetic patients. However, DES are associated with a slightly higher risk of late stent thrombosis, so prolonged dual antiplatelet therapy (DAPT) may be necessary.
10. What is the Importance of a Heart Team Approach in Decision-Making?
A heart team approach involves a multidisciplinary team of healthcare professionals, including cardiologists, cardiac surgeons, and diabetologists, working together to determine the best treatment strategy for each patient. This approach ensures that all treatment options are considered and that the patient’s individual needs and preferences are taken into account. The heart team approach is particularly important for diabetic patients with CAD, as their treatment is often complex and requires careful consideration of multiple factors. Shared decision-making between the heart team and the patient is essential for optimal outcomes.
11. How Does Coronary Artery Bypass Grafting (CABG) Compare to PCI in Diabetic Patients?
Coronary Artery Bypass Grafting (CABG) is another revascularization option for patients with CAD. CABG involves taking a healthy blood vessel from another part of the body (usually the leg, arm, or chest) and using it to create a bypass around the blocked artery in the heart. Several studies have shown that CABG is superior to PCI in reducing mortality and major adverse cardiovascular events (MACE) in diabetic patients with multivessel CAD. The FREEDOM trial, for example, found that CABG significantly reduced mortality and myocardial infarction compared to PCI in diabetic patients. However, CABG is a more invasive procedure than PCI and is associated with a higher risk of complications, such as stroke.
12. What is the Role of Optimal Glycemic Control in Managing CAD in Diabetic Patients?
Optimal glycemic control is crucial in managing CAD in diabetic patients. Poorly controlled diabetes can accelerate the progression of atherosclerosis and increase the risk of cardiovascular events. Studies have shown that tight glycemic control can reduce the risk of microvascular complications, such as nephropathy and retinopathy, but the impact on macrovascular events, such as heart attack and stroke, is less clear. The ACCORD trial, for example, found that intensive glycemic control was associated with an increased risk of mortality. Therefore, the goal of glycemic control should be individualized, considering the patient’s age, comorbidities, and risk of hypoglycemia.
13. How Does Optimal Blood Pressure Control Affect Outcomes in Diabetic Patients with CAD?
Optimal blood pressure control is essential in diabetic patients with CAD. High blood pressure can increase the risk of heart attack, stroke, and kidney disease. Studies have shown that lowering blood pressure can reduce the risk of cardiovascular events in diabetic patients. The target blood pressure for diabetic patients with CAD is generally
14. What Lifestyle Modifications Are Recommended for Diabetic Patients with CAD?
Lifestyle modifications are a crucial part of managing CAD in diabetic patients. Recommended lifestyle modifications include:
- Healthy diet: A diet low in saturated and trans fats, cholesterol, and sodium.
- Regular exercise: At least 150 minutes of moderate-intensity aerobic exercise per week.
- Smoking cessation: Quitting smoking is one of the most important things a diabetic patient with CAD can do to improve their health.
- Weight management: Maintaining a healthy weight can help improve blood sugar control, blood pressure, and cholesterol levels.
- Stress management: Stress can increase blood pressure and blood sugar levels.
15. What is the Role of Statins in Preventing Cardiovascular Events in Diabetic Patients?
Statins are a cornerstone of lipid-lowering therapy in diabetic patients with CAD. Statins work by blocking the production of cholesterol in the liver, which can lower LDL cholesterol levels and reduce the risk of cardiovascular events. Studies have shown that statins are highly effective in preventing heart attack, stroke, and death in diabetic patients with CAD. The Cholesterol Treatment Trialists’ (CTT) Collaboration meta-analysis found that statin therapy reduced the risk of major vascular events by about a fifth per mmol/L reduction in LDL cholesterol.
16. How Does the Presence of Chronic Kidney Disease Affect Treatment Decisions?
The presence of chronic kidney disease (CKD) can significantly affect treatment decisions in diabetic patients with CAD. CKD is a common comorbidity in diabetic patients and is associated with an increased risk of cardiovascular events. Patients with CKD are at higher risk of complications from both PCI and CABG, such as contrast-induced nephropathy and bleeding. The choice of treatment should be individualized, considering the severity of CKD and the potential benefits and risks of each approach.
17. What is the Role of Antiplatelet Therapy After PCI in Diabetic Patients?
Antiplatelet therapy is essential after PCI in diabetic patients to prevent stent thrombosis. Dual antiplatelet therapy (DAPT) with aspirin and a P2Y12 inhibitor (such as clopidogrel, prasugrel, or ticagrelor) is typically recommended for at least 12 months after DES implantation. Studies have shown that DAPT significantly reduces the risk of stent thrombosis and cardiovascular events after PCI. However, DAPT is associated with an increased risk of bleeding, so the duration of therapy should be individualized, considering the patient’s risk of bleeding and ischemic events.
18. How Can COMPARE.EDU.VN Help Patients Make Informed Decisions About Treatment?
COMPARE.EDU.VN provides comprehensive and unbiased information to help patients make informed decisions about their health. We offer detailed comparisons of different treatment options, including PCI and OMT, and provide the latest research findings on the effectiveness and safety of these approaches. Our user-friendly website makes it easy for patients to compare different treatments side-by-side and to find the information they need to make the right choice for their individual situation. We understand that navigating the healthcare system can be confusing and overwhelming, and we are committed to providing patients with the knowledge and resources they need to take control of their health.
19. What Are the Long-Term Outcomes of PCI vs. OMT in Diabetic Patients?
The long-term outcomes of PCI versus OMT in diabetic patients are variable and depend on several factors, including the severity of CAD, the presence of comorbidities, and the effectiveness of medical management. Some studies have shown that PCI can provide better symptom relief and reduce the need for further interventions in the short term, but the long-term benefits on mortality and cardiovascular events are less clear. Other studies have found that CABG is superior to PCI in reducing mortality and myocardial infarction in diabetic patients with multivessel CAD. Long-term follow-up is essential to assess the durability of treatment effects and to monitor for the development of new cardiovascular events.
20. How Can Patients Find a Qualified Heart Team to Guide Their Treatment?
Finding a qualified heart team is essential for diabetic patients with CAD. Patients can start by asking their primary care physician for a referral to a cardiologist who specializes in the treatment of CAD. It is also important to find a hospital or medical center that has a multidisciplinary heart team, including cardiologists, cardiac surgeons, and diabetologists. Patients should ask potential heart teams about their experience in treating diabetic patients with CAD and their approach to shared decision-making. The American Heart Association and the American College of Cardiology websites also have resources to help patients find qualified healthcare professionals.
21. What Are the Latest Advances in PCI Techniques for Diabetic Patients?
Several advances in PCI techniques have improved outcomes for diabetic patients:
- Drug-eluting stents (DES): DES have significantly reduced the risk of restenosis after PCI.
- Bioabsorbable stents: These stents dissolve over time, reducing the risk of long-term complications.
- Optical coherence tomography (OCT): OCT is an imaging technique that provides detailed views of the coronary arteries, allowing cardiologists to better assess the severity of CAD and guide PCI procedures.
- Fractional flow reserve (FFR): FFR is a technique used to measure the blood flow through a coronary artery, helping cardiologists determine whether a blockage is significant enough to warrant PCI.
22. How Can Patients Actively Participate in Their Treatment Decisions?
Patients can actively participate in their treatment decisions by:
- Educating themselves: Learning about CAD and the different treatment options.
- Asking questions: Asking their healthcare team questions about their condition and treatment options.
- Sharing their preferences: Letting their healthcare team know their values and preferences.
- Seeking a second opinion: Getting a second opinion from another healthcare professional.
- Participating in shared decision-making: Working with their healthcare team to make informed decisions about their treatment.
23. What Support Services Are Available for Diabetic Patients with CAD?
Several support services are available for diabetic patients with CAD:
- Cardiac rehabilitation: A supervised exercise and education program that helps patients recover from heart attack, PCI, or CABG.
- Diabetes education: Education programs that teach patients how to manage their diabetes.
- Support groups: Groups where patients can connect with others who have CAD or diabetes.
- Counseling: Counseling services to help patients cope with the emotional challenges of living with CAD or diabetes.
- Online resources: Websites and online communities that provide information and support for patients with CAD or diabetes.
24. How Important Is Medication Adherence in Managing CAD in Diabetic Patients?
Medication adherence is critically important in managing CAD in diabetic patients. Many of the medications used to treat CAD and diabetes, such as statins, antiplatelet drugs, and blood pressure medications, need to be taken regularly to be effective. Non-adherence to medications can increase the risk of cardiovascular events and other complications. Patients should work with their healthcare team to develop a medication plan that is easy to follow and to address any barriers to adherence.
25. What Emerging Therapies Show Promise for Treating CAD in Diabetic Patients?
Several emerging therapies show promise for treating CAD in diabetic patients:
- Regenerative medicine: Therapies that use stem cells or other biological materials to repair damaged heart tissue.
- Gene therapy: Therapies that use genes to treat or prevent disease.
- PCSK9 inhibitors: A new class of cholesterol-lowering drugs that can significantly lower LDL cholesterol levels.
- SGLT2 inhibitors: A class of diabetes medications that have been shown to reduce the risk of cardiovascular events in diabetic patients with CAD.
26. What Questions Should Patients Ask Their Doctor About PCI vs. OMT?
Patients should ask their doctor the following questions about PCI versus OMT:
- What are the potential benefits and risks of PCI and OMT for my specific situation?
- Which treatment option is most likely to improve my symptoms and quality of life?
- What are the long-term outcomes of PCI and OMT?
- What are the potential complications of each treatment option?
- How will diabetes affect my outcomes after PCI?
- What lifestyle modifications should I make to improve my health?
- What medications will I need to take after PCI or OMT?
- How often will I need to follow up with you after PCI or OMT?
- Is a heart team approach available at this hospital or medical center?
- What is your experience in treating diabetic patients with CAD?
27. What Are the Potential Economic Considerations of PCI vs. OMT?
The economic considerations of PCI versus OMT can be significant. PCI is typically more expensive than OMT in the short term, but OMT can require long-term medication costs and frequent doctor visits. Studies have shown that the cost-effectiveness of PCI versus OMT depends on several factors, including the severity of CAD, the presence of symptoms, and the effectiveness of medical management. Patients should discuss the potential economic implications of each treatment option with their healthcare team and insurance provider.
28. How Does Age Influence the Decision-Making Process for PCI vs. OMT?
Age can significantly influence the decision-making process for PCI versus OMT. Older patients may be at higher risk of complications from PCI and CABG, such as stroke and bleeding. They may also have other comorbidities that can complicate treatment decisions. The potential benefits of PCI and CABG may be less pronounced in older patients due to their shorter life expectancy. The decision on whether to pursue PCI or OMT should be individualized, considering the patient’s age, overall health status, and preferences.
29. How Does Gender Impact Outcomes and Treatment Strategies?
Gender can impact outcomes and treatment strategies in diabetic patients with CAD. Women with diabetes tend to have worse cardiovascular outcomes compared to men. They may also have different risk factors and comorbidities that can influence treatment decisions. Studies have shown that women may be less likely to be referred for PCI or CABG compared to men, even when they have similar symptoms and disease severity. Healthcare providers should be aware of these gender differences and ensure that women receive equitable and appropriate treatment.
30. What Resources Does COMPARE.EDU.VN Provide to Help Patients Compare Treatment Options?
COMPARE.EDU.VN provides a variety of resources to help patients compare treatment options for CAD and diabetes. Our website includes:
- Detailed comparisons of PCI and OMT: Side-by-side comparisons of the benefits, risks, and costs of each treatment option.
- Articles on the latest research: Up-to-date information on the effectiveness and safety of different treatments.
- Patient stories: Real-life stories from patients who have undergone PCI or OMT.
- Expert opinions: Insights from leading cardiologists and diabetologists on the management of CAD in diabetic patients.
- Interactive tools: Tools to help patients assess their risk of cardiovascular events and make informed decisions about their treatment.
- Glossary of terms: Definitions of common medical terms related to CAD and diabetes.
At COMPARE.EDU.VN, we understand that making informed decisions about your health can be challenging. That’s why we strive to provide comprehensive and easy-to-understand information to empower you to take control of your healthcare journey.
Making informed decisions about your health is crucial, and COMPARE.EDU.VN is here to assist you every step of the way.
For comprehensive comparisons and detailed insights, visit COMPARE.EDU.VN today and make informed choices about your health. Our team at COMPARE.EDU.VN is dedicated to providing you with the resources and information you need to make the best decisions for your unique situation. For more information, please contact us at:
Address: 333 Comparison Plaza, Choice City, CA 90210, United States
WhatsApp: +1 (626) 555-9090
Website: compare.edu.vn
FAQ: PCI vs. Medical Therapy in Diabetic Patients
1. Is PCI always the best option for diabetic patients with heart disease?
No, PCI is not always the best option. The decision depends on factors like the severity of heart disease, symptoms, and overall health.
2. What are the main benefits of medical therapy over PCI?
Medical therapy avoids the risks of surgery and can effectively manage symptoms for some patients.
3. How does diabetes affect the success rate of PCI?
Diabetes can increase the risk of complications like restenosis and stent thrombosis.
4. Can lifestyle changes replace the need for PCI in diabetic patients?
Lifestyle changes are crucial but may not always be sufficient to manage severe blockages.
5. What is the role of new-generation stents in PCI for diabetics?
New-generation stents reduce the risk of restenosis compared to older stents.
6. Are there specific medications that improve outcomes after PCI in diabetics?
Yes, dual antiplatelet therapy (DAPT) and statins are commonly used to improve outcomes.
7. How does a heart team approach help in deciding between PCI and medical therapy?
A heart team provides a comprehensive evaluation and considers all treatment options.
8. What are the long-term survival rates for diabetics undergoing PCI versus medical therapy?
Long-term survival rates vary, and recent studies suggest CABG may be superior to PCI in certain cases.
9. How does age affect the choice between PCI and medical therapy?
Older patients may face higher risks with PCI, making medical therapy a more suitable option.
10. What is the role of regular follow-ups after PCI or starting medical therapy?
Regular follow-ups help monitor treatment effectiveness and manage any complications.