Do lab mice tests compare to humans? Yes, but with nuances. This comprehensive analysis from COMPARE.EDU.VN explores the complexities of using laboratory mice in research and their relevance to human health, offering solutions for understanding translational value. Explore model fidelity and clinical relevance for informed decision-making.
Table of Contents:
- Mouse Natural History
- Mice in Biomedical Research: The Good, the Bad, and the Ugly
- SPF Mouse Husbandry
- Getting More from the Mouse Model
- Conclusions
- FAQ Section
1. What is the Mouse Natural History?
The house mouse, Mus musculus, stands as a crucial in vivo mammalian model in modern biomedical research. The name “Mus” originates from the Sanskrit term for thief, reflecting the intricate relationship between mice and humans. These mice boast the widest geographical distribution among mammals, excluding humans. Mus musculus emerged in central Asia and traveled across the world with humans via land and sea. While house mice have evolved to thrive in varied climates, they frequently struggle in the wild against other mouse species, relying on civilization for survival. They’re closer relatives to humans than canines, sharing a common ancestor roughly 65-75 million years ago.
Mus musculus comprises different subspecies: M. m. domesticus colonized Western Europe, Africa, the Near East, the Americas, and Australia. M. m. musculus spread into central and Eastern Europe and China. M. m. castaneus moved into Southeast Asia, and M. m. Molossinus into Japan. Their widespread distribution is due to their adaptability to living near humans. Their breeding strategy, resulting in small populations that adapt to their surroundings, also contributes to their success. They inhabit social groups called demes, consisting of a dominant breeding male, a hierarchy of females, subordinate males, and juveniles. High inbreeding, along with high mutation rates, enables quick adaptation to environmental changes. Mice are omnivorous, nocturnal, and adaptable to temperature extremes, making them adept at exploiting human food sources.
1.1. How Mice Became a Pest Species
Mice are seen as pests due to their consumption and contamination of food stores. However, enthusiasts began breeding and selling mice with unique coat colors and behaviors, leading to the creation of the laboratory mouse.
2. How Are Mice Used in Biomedical Research: The Good, the Bad, and the Ugly?
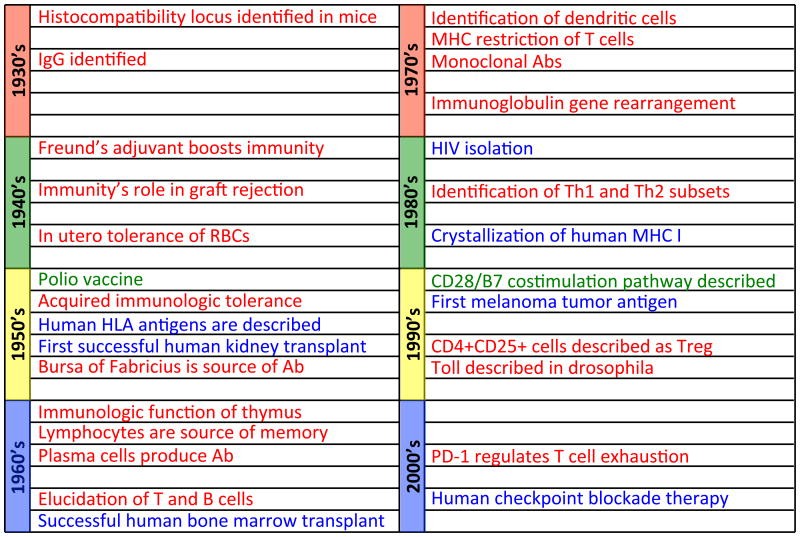
The use of mice in laboratories started with genetics studies in the early 20th century. Mendelian inheritance was demonstrated in mice by Lucien Cuenot in 1902 and Clarence Cook Little in 1910. Little created the first inbred mouse strains to aid in tumor studies and, with Ernest Tyzzer, established basic principles of tissue transplantation. Questions about human cancer genetics spurred the creation of other inbred strains with different tumor susceptibility levels. During the mid-20th century, mice became increasingly important in immunology research. Mouse models were critical for understanding antibody-antigen interaction, lymphoid differentiation, and responses to infectious agents. The use of inbred, congenic, and recombinant congenic mice revealed how polymorphic MHC genes regulate the mammalian immune system.
2.1. What Advances Have Mice Enabled?
Many key advances in biomedicine and immunology may not have been possible without the study of mice. Genetic linkage mapping, genome sequencing, sophisticated gene manipulation strategies, and the ability to transfer cells from one inbred mouse to another without immunological rejection accelerated the application of mice for investigating human diseases and immunology. Mice and humans share over 90 percent of the same genes. Gene discovery in humans can often be predicted in mice and vice versa. Mice develop spontaneous mutations, and there is now the ability to control genetics through breeding and manipulation of the genome via conditional and inducible transgenic and gene knockout strains, allowing the study of complex genetic diseases. Mice are small, easy to handle and transport, and can be maintained in a laboratory setting. They are prolific breeders and have a short generation time, allowing access to large numbers of animals quickly. With short lifespans, their entire life cycle and disease processes can be studied over only two years, versus decades in humans.
2.2. What Are the Drawbacks of Using Mice in Research?
Despite considerable homology, there are significant physiological and genetic differences that impede the development of mouse models that capture essential features of human disease. Some have proposed that the mouse transcriptional response to inflammatory perturbations poorly mimics that of humans. Complex human diseases are often tackled in mice with blunt approaches to hasten disease progression or induce diseases not naturally observed in mice. These strategies have a mixed track record for inspiring therapies that succeed in the clinic. For instance, atherosclerosis develops poorly in typical mouse strains without severe genetic defects, which is not a normal feature of afflicted humans. Cancer, a very complicated and multi-factorial spectrum of diseases, is an example of both the weaknesses and strengths of mouse models: over-reliance on transplantable tumor cell lines has missed critical characteristics of adaptations employed by slowly evolving human cancers.
Mouse studies on acute and chronic infectious diseases have proven valuable for understanding the foundations for protective immunity, and mouse models have helped understand ways in which pathogens take the upper hand. Still, species-specific idiosyncrasies of many important pathogens limit the ability of mouse models to recapitulate key aspects of human-pathogen interactions and highly evolved immune defense strategies. Differences in pathophysiology may arise even when mouse models can be established, such as the failure of MTb infection in mice to reproduce key features of human disease, including latency and highly organized granulomas.
2.3. How Can Mouse Models Misdirect Efforts?
Mouse models can misdirect efforts to cure un-physiologic diseases intrinsic only to the model and not the human condition. This has led to impressive mouse therapies that have failed to impact the actual disease in humans. This outcome could be blamed on strategic failures in designing experiments and model systems that minimize limitations while maximizing opportunities for clinical relevance. Nevertheless, the imperfections of current mouse models have led to a growing call to tilt limited immunology research resources away from animals and towards humans themselves. While human studies have and will continue to be essential to the overall immunology discovery program, the perceived advantages of human research must be balanced with its inherent limitations, the chief ones being limited opportunities to derive appropriate samples under suitably controlled conditions. For example, much of human immunology relies on studies of blood, which fails to capture local immune responses and characterize resident lymphocyte and innate immune system components.
2.4. How Does Environment Affect Mouse Models?
Differences between immune responses in mice and humans are attributed to genetics, lifespan, or species-pathogen relationships. However, environmental differences in laboratory mouse husbandry are also a contributing factor. While mice can forage over a broad temperature range, their nests are typically in a thermoneutral zone of 30-32°C, and there is growing concern that laboratory mice are chronically subjected to cold stress. This involves an increased “basal” metabolic rate, glucocorticoid production, and sustained activation of the sympathetic nervous system. This deviation has been reported to alter responsiveness to LPS, the febrile response, and markedly influences immunological endpoints including the response to infection and cancer. Simply increasing the temperature in the vivarium to what is most comfortable for mice could increase the translation value. Another aspect of the environment in which laboratory mice are raised is the impact of natural microbial exposure.
3. What is SPF Mouse Husbandry?
Early on in the use of laboratory mice, controlling the introduction of pathogens into colonies was difficult. Animals were often housed in wooden cages that were difficult to clean, and there were not effective means to identify pathogens. Starting in the mid-1900s, there has been an increasing focus on identifying strategies to control the spread of pathogens in laboratory animal facilities. It was not until the 1980s that modern filter-top microisolation cages became commercially available. These systems are still commonly used in animal facilities today.
As immunologists increased their use of inbred mice and developed strains with compromised or aberrant immune systems, the pressure grew to develop housing approaches that would allow reliable and reproducible ways to maintain these animals. Pathogens that might have only eliminated some unfortunate individuals in a wild mouse population could decimate a colony of inbred mice. Uncharacterized infections could unpredictably alter immune response properties, leading to misinterpretation of phenotype. Without implementation of containment and screening procedures, these genetically well-defined mouse strains might become more of a liability than an asset. The phrase Specific Pathogen Free (SPF) dates to the late 1950s, being used to describe the microbiological status of mouse colonies that are free from a defined list of pathogens that includes exogenous viruses, bacteria, and parasites. Use of such barrier housing criteria was in widespread use by the early 1970s.
3.1. What Does SPF Mean for Mice?
Although free from these pathogens, the complete microbiota of SPF colonies may not be known, and SPF mice were clearly recognized as being distinct from germ-free or axenic mice, which were first generated around the same time. The selection of excluded agents, and thus the definition of SPF, can vary considerably from institution to institution, but include many common pathogens that mice are routinely exposed to in the wild.
Rigorous biocontainment is the most effective tool used to control the introduction of unwanted pathogens into mouse facilities. Mice in SPF colonies are generally housed under barrier conditions. While “barrier” can have many meanings, in many facilities, it denotes primary housing in microisolation cages (with filtered tops) or individually vented cages, both approaches used to prevent the introduction of pathogens into the cage from the environment. Additional steps include the use of aseptic technique when handling animals and appropriate disinfection or sterilization of cages, equipment, food, and water that comes in contact with the mice.
In order to protect existing SPF colony animals, many facilities will not accept direct import of animals from colonies or facilities that have tested positive for an agent on their exclusion list or will insist on a lengthy quarantine process or expensive rederivation prior to import. With the routine implementation of these practices, adherence to SPF colony management has become ingrained in the psyche of most cellular immunologists, and as a result, it is now difficult to appreciate that impact of these policies. The laudable goal of protecting vulnerable animals from life-threatening pathogens also means that these animals have a profoundly un-physiological infectious history, making them quite unlike mice – and humans – in the wild.
4. How Can We Get More from the Mouse Model?
Evidence that microbial experience impacts the immune response of laboratory mice is compelling. At its most extreme, the development of gnotobiotic, or germ-free, mice has revealed the profound impact of commensal organisms on everything from host metabolism to pathogen vulnerability. Gut microbiota correlates with obesity, health status, and metabolic and inflammatory diseases. Many experimentalists have noted that a key phenotype of a certain mouse strain is no longer reproducible upon changing lab locations or simply by housing their mice in a different room at the same institution. A noted example is the non-obese diabetic (NOD) mouse strain, which develops diabetes efficiently in very “clean” animal rooms but shows substantially less disease incidence when colonized by certain commensal microbes. Mice purchased from different vendors vary considerably in the presence of Th17 cells within the intestinal mucosa. Littman and colleagues pursued the basis for this discrepancy, elegantly demonstrating that the difference could be attributed to a single member of the gut microbiota.
4.1. How Does Pathogen Exposure Affect Mice?
Intentional pathogen experience in SPF mice resulted in unanticipated yet substantial effects on graft rejection, resistance to infection, and de novo adaptive immune responses. Studies comparing healthy monozygotic and dizygotic human twins revealed that variation in cell population frequencies, cytokine responses, and serum proteins were determined not only by genetics but also substantially a consequence of non-heritable factors, consistent with the interpretation that environmental and microbial exposure drives much of the immune system variation among individuals. Our immune systems have evolved to live in the microbial world we inhabit, and microbial experience profoundly influences steady-state immune function and development of de novo responses.
These observations raise many questions: What are we missing by conducting the majority of mouse experiments under SPF conditions? Are there practicable methods to return laboratory mice to a more physiologic level of microbial experience? If so, would such an endeavor have value?
4.2. What Are “Dirty” Mice?
In “dirty” mice, which have completely natural exposure to environmental pathogens, there is a dramatic increase in the frequency of memory-phenotype CD8+ T cells in both lymphoid and non-lymphoid tissues, resembling resident memory T cells. These characteristics are similar to what is observed in adult humans. Infectious agents drive these changes in immune populations. Co-housing pet store animals with lab mice led to acquisition of “dirty” characteristics by the latter group. Increased numbers of circulating and tissue-resident memory CD8 T cells accompanied colonization of the mice by diverse SPF-designated pathogens. These changes were not limited to CD8 T cells – differentiated CD4+ T cell subsets, ILC, and myeloid populations were increased in numbers within various lymphoid and non-lymphoid sites, and serum immunoglobulins (Igs) of diverse isotypes were significantly elevated. These characteristics are analogous to immunologically experienced adult humans.
4.3. What Gene Expression Patterns Distinguish Dirty Mice from SPF Mice?
Many gene expression patterns that distinguish adult from neonatal humans were the same as those that distinguished dirty mice from SPF mice. Most striking among these was a substantial elevation in the expression of genes regulated by Type-I IFNs in dirty mice and adult humans (compared to SPF mice and neonatal humans, respectively). These data suggested that co-housed inbred mice, by having a more physiological exposure to natural mouse pathogens, were a more accurate reflection of the adult human immune system – and hence would be more relevant to the translation of mouse immunology studies.
4.4. What Are the Challenges of Using Dirty Mice?
Use of dirty mice presents opportunities for new dimensions in immunology research, but the generation and maintenance of these mice is far from trivial. By definition, dirty mice harbor numerous pathogens that are excluded from modern SPF animal facilities, and contamination is a serious risk. Some pathogens, such as pinworm eggs, remain viable in the environment for long periods, and numerous SPF-excluded pathogens are notorious for efficient transmission. Hence, dirty mice must be isolated away from SPF colonies. Achieving this using an ABSL3 facility exceeds the safety level needed for personnel but provides highly effective containment. Other options may be to utilize a facility in which no other rodent colonies are housed, or in a quarantine area located away from regular housing rooms. In all cases, measures need to be in place to minimize the risk of pathogen spread by fomites and directional airflow to reduce airborne spread of pathogens.
4.5. How Can a Dirty Mouse Colony Be Created?
Creating a dirty mouse colony can be done in several ways. Mice obtained from pet stores or captured in the wild are often exposed to multiple bacterial, viral, and parasitic pathogens. Many of these pathogens establish persistent infections that can be spread to inbred mice by co-housing, and some can be transmitted from contaminated bedding. This approach introduces immunological experience to lab mice with known genetics and is compatible with genetic-dependent experimental approaches such as gene knockout mice. Whether or not an animal will seroconvert upon exposure depends on dose, agent and age, immune status, and genetic composition of the infected animal. Accordingly, not all dirty mice will have the same infection profile, and utilizing these methods may result in significant variation between mice. Alternatively, dirty mice can be generated by deliberate infection of SPF mice with a selected series of pathogens.
Selecting the pathogens that best model naturally acquired infections in mice is not simple – some microbes that might be assumed to be prevalent in wild or pet store mice (such as MCMV) may be infrequent, and the only microbes that matter for immunological experience may not be those that are on the SPF excluded list. Hence, there are good reasons to advocate for use of both the natural transmission and deliberate infection models of generating dirty mice.
4.6. How Does This Affect Experimental Reproducibility?
The issue of experimental reproducibility is a concern when dirty mice are generated by natural transmission between animals, since this invites heterogeneity in the timing and nature of infections. The immune system in SPF mice can be quite dramatically perturbed by changes in the microbiota. These effects may be magnified because SPF mice have such modest immunological experience, and perhaps more diverse pathogen exposure would induce more stability to these phenotypes.
If the end goal is to robustly model phenomena observed in humans, most of whom have diverse microbial experience, shouldn’t our mouse models be similarly diverse? Before moving to an expensive clinical trial, it might be reassuring to validate therapeutics in both SPF and dirty mouse models, in order to filter out modalities that are highly sensitive to unique environmental perturbations. In these ways, the dirty mouse model may be seen as a complement rather than any kind of replacement for current studies of the immune system in SPF mice and humans.
5. What Conclusions Can Be Drawn?
While expanding studies on human cells and tissues is a laudable objective for immunology research, the considerable benefits offered by the mouse model should secure its place in future work on the basic underpinnings of the immune system. Normalizing the immunological experience of laboratory mice comprises one step towards this goal but should be viewed as an element in the larger progression to improve the value of mice as a model for the human immune system.
6. FAQ Section
6.1. What are the main differences between SPF and dirty mice?
SPF mice are raised in pathogen-free environments, while dirty mice are exposed to various pathogens found in natural environments.
6.2. Why are SPF mice commonly used in research?
SPF mice are commonly used because they provide a controlled environment that reduces variability and allows for more reproducible results.
6.3. What are the potential benefits of using dirty mice in research?
Dirty mice may better mimic the human immune system, potentially leading to more translatable research findings.
6.4. What are the challenges of maintaining a dirty mouse colony?
Maintaining a dirty mouse colony requires strict isolation and containment measures to prevent contamination of SPF colonies.
6.5. How does the temperature in a vivarium affect mouse physiology?
Chronically cold temperatures in a vivarium can cause stress, altering metabolic rates and immune responses in mice.
6.6. What is the role of gut microbiota in mouse models?
Gut microbiota plays a significant role in metabolism, immune function, and susceptibility to diseases in mouse models.
6.7. Can environmental factors influence the reproducibility of mouse experiments?
Yes, environmental factors such as temperature, microbial exposure, and housing conditions can significantly impact experimental reproducibility.
6.8. How do mouse models help in understanding human diseases?
Mouse models help in understanding the genetic and immunological mechanisms underlying human diseases.
6.9. What is the importance of genetic similarity between mice and humans?
The genetic similarity between mice and humans allows for the study of human genes and diseases in a controlled laboratory setting.
6.10. What steps can be taken to improve the translatability of mouse research to human health?
Steps include normalizing immunological experience, using appropriate housing conditions, and validating findings in both SPF and dirty mouse models.
Making informed decisions based on comprehensive comparisons is now easier than ever with COMPARE.EDU.VN. If you’re grappling with choices and seeking clarity, COMPARE.EDU.VN offers detailed, objective comparisons to help you decide.
Find us at 333 Comparison Plaza, Choice City, CA 90210, United States. Or contact us on Whatsapp: +1 (626) 555-9090. Explore more at compare.edu.vn today. Let us help you make confident choices.