Can You Directly Compare Smrs? No, you cannot directly compare Standardized Mortality Ratios (SMRs) unless they are calculated using the same standard population. COMPARE.EDU.VN provides detailed comparisons and analyses to help you understand the nuances of SMRs and their applications. This comprehensive guide explores the intricacies of SMRs, their calculation, interpretation, and limitations, offering valuable insights for healthcare professionals and researchers seeking to evaluate mortality data effectively. Understand how to utilize comparative metrics, risk adjustment, and outcome evaluation with the resources available at COMPARE.EDU.VN.
1. Understanding Standardized Mortality Ratio (SMR)
The Standardized Mortality Ratio (SMR) is a crucial metric in healthcare, used to compare the mortality rate of a specific population with that of a standard or reference population. It’s essentially a ratio of observed deaths to expected deaths.
1.1. What is SMR?
The Standardized Mortality Ratio (SMR) assesses whether a particular group, like patients in a hospital, experiences higher, lower, or similar mortality rates compared to a standard population, such as all patients in UK hospitals (1). The SMR is a vital tool for comparing mortality outcomes across different populations while accounting for variations in age and sex distribution.
1.2. Why Standardize?
Crude death rates don’t account for age distribution. Populations with more elderly people will naturally have higher death rates. It’s fairer to compare hospitals or mortality trends over time by considering the population’s age structure (1, 2). Standardization provides a single comparable figure, simplifying the analysis of death rates across populations with different age distributions, although it does involve some loss of detailed information (2).
1.3. Direct vs. Indirect Standardization
Mortality data can be standardized using direct or indirect methods (3). Direct standardization requires age-sex-specific rates for the study population and the age-sex structure of the standard population. Indirect standardization, used to calculate the SMR, is employed when age-specific rates for the study population are unavailable. This method compares observed deaths in the study population with expected deaths based on the standard population’s age distribution (4). To minimize bias, the standard population’s age distribution should closely match the study population’s (5). SMR offers lower variance than direct standardization, providing more precise estimates, especially useful in hospitals with small numbers of deaths (5).
2. How to Calculate the Standardized Mortality Ratio
Calculating the SMR involves a series of steps that take into account age- and sex-specific categories. Let’s break down the process with a clear formula and detailed instructions.
2.1. SMR Formula
The SMR is calculated as follows:
SMR = Number of Observed Deaths / Number of Expected Deaths
2.2. Calculating Expected Deaths
To calculate the number of expected deaths, follow these steps:
A. Obtain Standard Population Death Rates: Gather age- and sex-specific death rates for the standard population. These rates may be per 1,000, per 10,000, or per 100,000.
B. Estimate Population Size: Determine the number of people in each age-sex category for both the standard and the study populations.
C. Calculate Expected Deaths per Category: Multiply the age-sex-specific death rates in the standard population (Step A) by the number of people in each category of the study population (Step B).
D. Sum Expected Deaths: Add all the age- and sex-specific expected deaths to obtain the total expected number of deaths for the entire study population.
2.3. Final Calculation
Divide the observed number of deaths by the expected number of deaths to get the SMR.
3. Interpreting the SMR Value
The SMR value provides insight into the mortality experience of the study population relative to the standard population. Understanding what different SMR values indicate is crucial for drawing meaningful conclusions.
3.1. SMR Interpretation
- SMR = 1.0: The number of observed deaths equals the number of expected deaths in the study population.
- SMR > 1.0: There were more deaths than expected in the study population (excess deaths).
- SMR < 1.0: There were fewer deaths than expected in the study population.
When the SMR is expressed after multiplying by 100:
- SMR = 100: Observed deaths equal expected deaths.
- SMR > 100: There were excess deaths.
- SMR < 100: There were fewer deaths than expected.
3.2. Significance Testing
To determine if the SMR is significant, calculate the 95% Confidence Interval (CI):
95% CI = 1.96 x Standard Error of SMR
Standard Error of SMR = (Square Root of Observed Deaths) / Number of Expected Deaths
If the 95% confidence intervals do not cross 1.0, the SMR is significant.
4. Practical Example of SMR Calculation
Let’s walk through a detailed example to illustrate how the SMR is calculated and interpreted. This will help solidify your understanding of the process.
4.1. Scenario
Consider a hospital assessing the quality of care in its intensive care unit (ICU). Data is collected on admissions to the ICU over one year, categorized by age and sex. The hospital wants to compare its mortality rate to a standard population.
4.2. Data
The data includes:
- Standard population age- and sex-specific death rates.
- Hospital A’s ICU admissions by age and sex.
- Observed deaths in Hospital A’s ICU: 149.
4.3. Calculation
Using the data, the expected number of deaths in Hospital A’s ICU is calculated to be 119.8.
SMR = Number of Observed Deaths / Number of Expected Deaths
SMR = 149 / 119.8 = 1.24 (2 d.p.)
4.4. Interpretation
Since 1.24 > 1.0, there were excess deaths in Hospital A’s ICU. The number of excess deaths is approximately 149 – 120 = 29. Expressed as a percentage, the SMR is 124, which also indicates excess deaths.
4.5. Significance Testing
To determine if the SMR is significant:
Standard Error of SMR = (Square Root of 149) / 119.8 = 0.10189
95% CI = 1.96 x 0.10189 = 0.200
Upper Confidence Interval = 1.24 + 0.200 = 1.44
Lower Confidence Interval = 1.24 – 0.200 = 1.04
The 95% confidence interval (1.04 to 1.44) does not cross 1.0, so the SMR is significant.
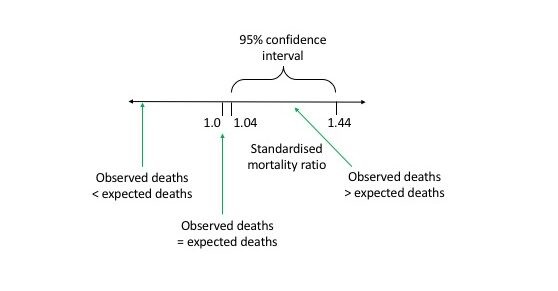 STandardized Mortality Ratio diagram
STandardized Mortality Ratio diagram
5. Next Steps After Calculating the SMR
An SMR figure is only the start. It is used for comparative purposes. SMRs are compared to upper and lower control limits; variations within these limits are due to random chance. Data points outside these limits suggest factors that warrant further examination (6). A high SMR doesn’t explain why there are excess deaths, but it indicates the need for investigation. Excess deaths may be avoidable, unexpected, or due to poor quality of care (7).
6. Factors Influencing Mortality Rates
Mortality rates are influenced by various factors beyond just age and sex. Including additional factors in standardized mortality ratios can provide a more nuanced understanding.
6.1. Additional Factors
Other factors often included are:
- Diagnosis
- Deprivation
- Co-morbidities
- Whether the patient is for palliative care
- The procedure the patient had
- Birthweight (when looking at infant mortality data) (8, 9)
6.2. Summary Hospital Mortality Indicator (SHMI)
For national reviews of hospital mortality, the Summary Hospital Mortality Indicator (SHMI) is used. Different variants exist, but common ones help provide a comprehensive overview.
7. Advantages and Limitations of SMR
Like any statistical tool, the SMR has its strengths and weaknesses. Being aware of these is crucial for proper application and interpretation.
7.1. Advantages
- Records are generally cheap and easy to obtain.
- The SMR is relatively simple to calculate.
- Trends can be mapped over time.
- Mortality is unambiguous, making comparisons between hospitals easier (6).
7.2. Limitations
- The SMR depends on the choice of standard population, making direct comparisons invalid if different standards are used.
- Without an illness severity scoring system, it’s hard to determine if deaths are among critically ill patients or those previously in good health.
- Morbidity data is excluded; patients may survive but be in poor health afterward.
- Differing admission and discharge practices can influence the SMR (6).
8. Comprehensive Comparison Table
To summarize, here is a comparison table highlighting key aspects of SMR:
| Feature | Description |
|---|---|
| Definition | Ratio of observed to expected deaths, comparing a specific population to a standard population. |
| Purpose | To assess mortality rates while adjusting for differences in population distributions, such as age and sex. |
| Calculation | SMR = (Observed Deaths / Expected Deaths). Expected deaths are calculated using age-sex-specific rates from the standard population. |
| Interpretation | SMR = 1.0 (or 100) indicates observed deaths equal expected deaths. >1.0 (or >100) indicates excess deaths. <1.0 (or <100) indicates fewer deaths. |
| Significance | Determined by calculating the 95% Confidence Interval (CI). If the CI does not cross 1.0, the SMR is statistically significant. |
| Advantages | Simple to calculate, uses readily available data, and allows for trend mapping over time. |
| Limitations | Dependent on the choice of standard population, does not account for illness severity, and is influenced by admission/discharge practices. |
| Influencing Factors | Diagnosis, deprivation, co-morbidities, palliative care status, procedures, and birthweight (for infant mortality). |
9. How COMPARE.EDU.VN Can Help
Navigating the complexities of SMR and other statistical measures can be challenging. That’s where COMPARE.EDU.VN comes in. We provide detailed, user-friendly comparisons and analyses to help you make informed decisions.
9.1. What We Offer
At COMPARE.EDU.VN, you can find:
- In-depth articles and guides on statistical methods.
- Tools to compare different healthcare metrics.
- Expert analysis of healthcare data.
- Resources for understanding and interpreting statistical results.
9.2. Why Choose Us?
COMPARE.EDU.VN offers:
- Reliable and accurate information.
- Easy-to-understand explanations.
- Comprehensive comparisons.
- Support for informed decision-making.
10. Real-World Applications and Case Studies
Understanding how SMR is applied in real-world scenarios can further clarify its utility. Let’s explore some case studies.
10.1. Case Study 1: Hospital Performance Evaluation
A hospital uses SMR to compare its mortality rates with national averages. By stratifying data by age, sex, and diagnosis, the hospital identifies areas where its mortality rates are significantly higher than expected. This prompts further investigation into the quality of care and specific protocols.
10.2. Case Study 2: Public Health Intervention
A public health department uses SMR to assess the impact of a new intervention program. By comparing SMRs before and after the intervention, they determine whether the program has effectively reduced mortality rates in the targeted population.
10.3. Case Study 3: Comparing Healthcare Systems
Researchers use SMR to compare mortality outcomes across different healthcare systems. By standardizing for age, sex, and socioeconomic status, they can identify best practices and areas for improvement in each system.
11. Addressing Common Misconceptions About SMR
There are several misconceptions about SMR that can lead to misinterpretations. Let’s address some of the most common ones.
11.1. Misconception 1: Higher SMR Always Means Poor Performance
A higher SMR doesn’t always indicate poor performance. It could be due to factors like a higher proportion of high-risk patients or differences in data collection methods. Further investigation is needed to understand the underlying causes.
11.2. Misconception 2: SMR Can Be Directly Compared Across Different Standard Populations
As mentioned earlier, SMRs can only be directly compared if they use the same standard population. Comparing SMRs calculated with different standards can lead to inaccurate conclusions.
11.3. Misconception 3: SMR Captures All Aspects of Healthcare Quality
SMR focuses solely on mortality and doesn’t capture other important aspects of healthcare quality, such as morbidity, patient satisfaction, and efficiency. A comprehensive assessment requires considering multiple metrics.
12. The Role of SMR in Quality Improvement
SMR plays a crucial role in quality improvement initiatives in healthcare. By providing a standardized measure of mortality, it helps identify areas where improvements are needed.
12.1. Identifying Areas for Improvement
SMR helps identify specific areas or patient groups with higher-than-expected mortality rates. This allows healthcare providers to focus their efforts on improving care in those areas.
12.2. Monitoring the Impact of Interventions
SMR can be used to monitor the impact of quality improvement interventions. By comparing SMRs before and after the intervention, healthcare providers can assess whether the intervention has been effective.
12.3. Benchmarking Performance
SMR allows healthcare providers to benchmark their performance against national or regional averages. This helps them identify best practices and areas where they can learn from others.
13. Future Trends in SMR and Mortality Analysis
The field of mortality analysis is constantly evolving. Here are some future trends to watch for.
13.1. Advanced Statistical Methods
Advanced statistical methods, such as hierarchical modeling and Bayesian analysis, are being used to improve the accuracy and precision of SMR calculations.
13.2. Integration with Electronic Health Records
The integration of SMR with electronic health records (EHRs) allows for more timely and comprehensive mortality analysis.
13.3. Focus on Patient-Reported Outcomes
There is a growing emphasis on incorporating patient-reported outcomes into mortality analysis to provide a more holistic view of healthcare quality.
14. Frequently Asked Questions (FAQ)
Here are some frequently asked questions about SMR:
14.1. What is the difference between SMR and crude mortality rate?
Crude mortality rate is the total number of deaths in a population divided by the total population. SMR adjusts for differences in population characteristics, such as age and sex.
14.2. How do I choose the right standard population?
The standard population should be similar to the study population in terms of key characteristics, such as age, sex, and socioeconomic status.
14.3. What does it mean if the confidence interval for SMR includes 1?
If the confidence interval includes 1, the SMR is not statistically significant, meaning the observed difference in mortality could be due to random chance.
14.4. Can SMR be used to compare different hospitals?
Yes, but only if they use the same standard population and adjust for other relevant factors, such as patient risk profiles.
14.5. How often should SMR be calculated?
SMR should be calculated regularly to monitor trends and identify potential issues in a timely manner.
14.6. What are the limitations of using SMR in small populations?
In small populations, SMR can be unstable and subject to large fluctuations due to random variation.
14.7. How can I improve the accuracy of SMR calculations?
Improve accuracy by using reliable data sources, adjusting for relevant confounding factors, and using appropriate statistical methods.
14.8. What other metrics should I consider in addition to SMR?
Consider metrics such as morbidity rates, patient satisfaction scores, and readmission rates to get a comprehensive view of healthcare quality.
14.9. How can SMR be used to drive quality improvement initiatives?
SMR can be used to identify areas where mortality rates are higher than expected, allowing healthcare providers to focus their efforts on improving care in those areas.
14.10. What is the role of risk adjustment in SMR?
Risk adjustment accounts for differences in patient risk profiles, ensuring that comparisons are fair and accurate.
15. Conclusion: Making Informed Decisions with COMPARE.EDU.VN
The Standardized Mortality Ratio (SMR) is a valuable tool for comparing mortality rates across different populations, but it’s essential to understand its nuances and limitations. By using COMPARE.EDU.VN, you can access the resources and information you need to make informed decisions and improve healthcare outcomes. We provide detailed comparisons, expert analysis, and user-friendly guides to help you navigate the complexities of SMR and other statistical measures. Visit COMPARE.EDU.VN today to explore our comprehensive resources and enhance your understanding of mortality analysis.
Don’t struggle with complex comparisons. Visit COMPARE.EDU.VN for clear, comprehensive analyses that empower you to make informed decisions. Need help? Contact us at 333 Comparison Plaza, Choice City, CA 90210, United States, or reach out via Whatsapp at +1 (626) 555-9090. Let compare.edu.vn be your guide to better understanding and decision-making. Navigate comparative metrics, risk adjustment, and outcome evaluation today.