A Comparative Cost Analysis Of Maxillofacial Trauma In Australia is a detailed study of the expenses associated with treating facial injuries, often revealing disparities linked to socioeconomic factors. COMPARE.EDU.VN offers in-depth comparisons to help understand these costs, focusing on injury mechanisms, fracture types, and surgical needs. By examining these elements, you can better grasp the financial implications and explore strategies for prevention and cost reduction in managing maxillofacial trauma.
1. Understanding Maxillofacial Trauma in Australia
Maxillofacial trauma refers to any physical injury to the face. These injuries can range from minor cuts and bruises to severe fractures involving the facial bones. In Australia, trauma remains a significant cause of morbidity and mortality, with facial injuries constituting a notable portion of these cases. Understanding the epidemiology and socioeconomic factors influencing these injuries is crucial for effective prevention and management.
1.1. What are the common causes of maxillofacial trauma?
The common causes of maxillofacial trauma include assaults, road traffic accidents (RTAs), falls, sports-related injuries, and workplace accidents. Assaults are a significant cause, particularly among individuals from disadvantaged socioeconomic backgrounds. RTAs, while decreasing due to safety measures, still contribute substantially. Falls are increasingly prevalent in the elderly population. The distribution of these causes varies with socioeconomic status, age, and gender.
1.2. How does socioeconomic status affect maxillofacial trauma?
Socioeconomic status significantly influences the causes and types of maxillofacial fractures. Studies show that individuals from disadvantaged socioeconomic backgrounds are more likely to sustain facial fractures due to assaults. In contrast, those from more affluent backgrounds may experience injuries from sports or recreational activities. This disparity highlights the impact of social determinants of health on injury patterns.
2. The Scope of a Comparative Cost Analysis
A comparative cost analysis of maxillofacial trauma examines all direct and indirect costs associated with these injuries. Direct costs include medical expenses such as hospitalization, surgery, medication, and rehabilitation. Indirect costs encompass lost productivity, travel expenses, and other related financial burdens. Comparing these costs across different patient groups and injury types provides valuable insights for healthcare planning and resource allocation.
2.1. What are the direct costs of treating maxillofacial trauma?
Direct costs of treating maxillofacial trauma involve expenses for hospitalization, surgical procedures, medications, imaging, and follow-up care. Hospitalization costs can vary widely depending on the severity of the injury and length of stay. Surgical interventions, such as open reduction and internal fixation (ORIF), contribute significantly to the overall cost. Medications for pain management and infection control also add to the expense.
2.2. What are the indirect costs associated with maxillofacial trauma?
Indirect costs related to maxillofacial trauma include lost wages, reduced productivity, and the economic impact on families and communities. Patients may require extended time off work to recover, leading to lost income. Additionally, there may be costs associated with travel to medical appointments, home care, and psychological support. These indirect costs can be substantial and often overlooked in traditional cost analyses.
3. Key Components of a Cost Analysis
A thorough cost analysis involves several key components, including data collection, cost identification, statistical analysis, and interpretation of results. Data on patient demographics, injury characteristics, treatment modalities, and outcomes are essential for accurate cost estimation. Statistical methods are used to compare costs across different groups and identify significant predictors of healthcare expenditure.
3.1. How is data collected for a cost analysis of maxillofacial trauma?
Data collection involves gathering information from medical records, hospital databases, insurance claims, and patient surveys. Key data points include patient demographics (age, gender, socioeconomic status), injury details (cause, type, severity), treatment interventions (surgical vs. non-surgical), length of stay, and complications. Accurate and comprehensive data collection is crucial for a reliable cost analysis.
3.2. What statistical methods are used in cost analysis?
Statistical methods used in cost analysis include descriptive statistics (means, medians, standard deviations) to summarize cost data, and inferential statistics (t-tests, ANOVA, regression analysis) to compare costs across different groups. Regression models can identify factors that significantly influence healthcare costs, such as socioeconomic status, injury severity, and comorbidities. These methods help to quantify the economic burden of maxillofacial trauma.
4. Socioeconomic Disparities in Maxillofacial Trauma Costs
Socioeconomic status is a critical factor influencing the costs associated with maxillofacial trauma. Studies consistently show that individuals from disadvantaged backgrounds face higher risks of injury and may experience longer hospital stays and increased complications. Understanding these disparities is essential for developing targeted interventions to reduce inequalities in healthcare access and outcomes.
4.1. How do socioeconomic factors influence treatment costs?
Socioeconomic factors influence treatment costs through various mechanisms. Individuals from disadvantaged backgrounds may delay seeking medical care, leading to more severe injuries and higher treatment costs. They may also have limited access to preventive services, increasing their risk of trauma. Additionally, these patients may experience poorer outcomes due to comorbidities and lack of social support, resulting in prolonged hospital stays and increased expenses.
4.2. What is the impact of socioeconomic status on length of stay?
Research indicates that socioeconomic status can affect the length of hospital stay for patients with maxillofacial trauma. Disadvantaged individuals may have longer stays due to more severe injuries, complications, or lack of adequate post-discharge care. Factors such as unstable housing, food insecurity, and limited access to transportation can hinder recovery and increase the need for extended hospitalization.
5. Injury Mechanisms and Associated Costs
The mechanism of injury plays a significant role in determining the type and severity of maxillofacial trauma, and consequently, the associated costs. Injuries resulting from assaults tend to be more complex and require more intensive treatment compared to those from falls or sports-related incidents. Understanding the cost implications of different injury mechanisms is crucial for prevention efforts.
5.1. What are the cost differences between assault-related and RTA-related injuries?
Assault-related injuries often involve multiple fractures and soft tissue damage, leading to higher treatment costs compared to RTA-related injuries. Assault victims may also require additional services such as mental health support and legal assistance, further increasing the overall cost. While RTAs can cause severe trauma, advancements in vehicle safety have reduced the severity of facial injuries in some cases.
5.2. How do falls in the elderly contribute to maxillofacial trauma costs?
Falls in the elderly are a growing concern due to the aging population and increased risk of comorbidities. Maxillofacial fractures resulting from falls can lead to prolonged hospital stays, increased complications, and higher mortality rates. These patients often require extensive rehabilitation and long-term care, contributing significantly to healthcare costs. Prevention programs targeting falls in the elderly are essential for reducing this burden.
6. Types of Fractures and Their Cost Implications
Different types of maxillofacial fractures vary in complexity and treatment requirements, leading to differences in healthcare costs. Orbitozygomatic fractures, involving the cheekbone and eye socket, are common and often require surgical intervention. Mandibular fractures, affecting the jawbone, can result from various causes and may necessitate ORIF. Understanding the cost implications of each fracture type is important for resource planning.
6.1. What are the costs associated with orbitozygomatic fractures?
Orbitozygomatic fractures often require surgical reconstruction to restore facial symmetry and function. The costs associated with these fractures include preoperative imaging (CT scans), surgical fees, anesthesia, hospitalization, and postoperative care. Complications such as vision problems or nerve damage can further increase treatment costs. Early and appropriate management is crucial for minimizing these expenses.
6.2. How do mandibular fractures impact healthcare costs?
Mandibular fractures can result from assaults, RTAs, falls, and sports-related injuries. Treatment may involve closed reduction, ORIF, or intermaxillary fixation (IMF). The costs associated with mandibular fractures include emergency room visits, imaging, surgery, anesthesia, and follow-up appointments. Patients may also require dental care to address any associated tooth damage. Prevention strategies targeting high-risk groups can help reduce the incidence and cost of these fractures.
7. The Role of Surgical Interventions in Cost Management
Surgical interventions, such as ORIF, are often necessary for treating complex maxillofacial fractures. While surgery can be costly, it can also improve patient outcomes and reduce the risk of long-term complications. A careful assessment of the risks and benefits of surgical versus non-surgical management is essential for optimizing healthcare resource utilization.
7.1. How does ORIF contribute to the cost of maxillofacial trauma treatment?
Open reduction and internal fixation (ORIF) involves surgically exposing the fracture site and using plates and screws to stabilize the bones. This procedure can be expensive due to the need for specialized equipment, skilled surgeons, and anesthesia. However, ORIF can lead to better functional outcomes and reduced risk of malunion or nonunion, potentially lowering long-term costs.
7.2. What are the alternatives to surgical intervention and their cost implications?
Alternatives to surgical intervention include closed reduction and conservative management with pain control and observation. These approaches may be less costly initially but can result in suboptimal outcomes and increased risk of complications. Non-surgical management may be appropriate for certain types of fractures, but a careful assessment of the potential benefits and drawbacks is essential.
8. The Impact of Complications on Healthcare Costs
Complications following maxillofacial trauma, such as infections, malunion, nonunion, and nerve damage, can significantly increase healthcare costs. These complications often require additional treatment, prolonged hospital stays, and increased utilization of healthcare resources. Prevention strategies, such as meticulous surgical technique and appropriate antibiotic use, are crucial for minimizing complications and reducing costs.
8.1. How do infections increase the cost of treating maxillofacial trauma?
Infections following maxillofacial trauma can result from contamination of the wound site, inadequate wound care, or compromised immune function. Treatment involves antibiotics, wound debridement, and possibly additional surgery. Infections can prolong hospital stays and increase the risk of long-term complications, leading to higher healthcare costs.
8.2. What are the cost implications of malunion and nonunion?
Malunion and nonunion occur when fractures heal in an improper position or fail to heal altogether. These complications can lead to functional impairment, chronic pain, and the need for corrective surgery. Revision surgery is often more complex and costly than the initial procedure. Prevention strategies, such as early and appropriate fracture management, are essential for reducing the risk of malunion and nonunion.
9. Prevention Strategies and Their Economic Benefits
Prevention strategies play a crucial role in reducing the incidence and severity of maxillofacial trauma, leading to significant economic benefits. Public health initiatives, such as campaigns against drunk driving, violence prevention programs, and fall prevention strategies, can effectively reduce trauma rates and lower healthcare costs.
9.1. What public health initiatives can reduce maxillofacial trauma?
Public health initiatives aimed at reducing maxillofacial trauma include stricter enforcement of drunk driving laws, violence prevention programs targeting high-risk communities, and fall prevention strategies for the elderly. These initiatives can raise awareness, change behaviors, and create safer environments, leading to a decrease in trauma rates.
9.2. How do violence prevention programs lower healthcare costs?
Violence prevention programs address the root causes of violence, such as poverty, substance abuse, and lack of educational opportunities. By providing resources and support to vulnerable communities, these programs can reduce rates of assault and interpersonal violence, leading to fewer maxillofacial injuries and lower healthcare costs.
10. Utilizing Registries for Cost Analysis and Quality Improvement
Registries, such as trauma registries, play a vital role in collecting and analyzing data on maxillofacial trauma. These registries can provide valuable information for cost analysis, quality improvement, and outcome monitoring. By tracking patient demographics, injury characteristics, treatment interventions, and outcomes, registries can help identify areas for improvement and inform healthcare policy.
10.1. How do trauma registries aid in cost analysis?
Trauma registries collect detailed data on patient injuries, treatments, and outcomes. This data can be used to perform cost analysis and identify factors that influence healthcare expenditure. Registries can also track the costs associated with different types of injuries, treatment modalities, and complications, providing valuable insights for resource allocation and quality improvement.
10.2. What is the role of registries in improving outcomes for maxillofacial trauma patients?
Registries can be used to monitor outcomes for maxillofacial trauma patients and identify areas where care can be improved. By tracking complication rates, length of stay, and functional outcomes, registries can help healthcare providers identify best practices and implement strategies to enhance patient care. Registries can also facilitate research and collaboration among healthcare institutions, leading to advances in trauma management.
11. The Role of Multidisciplinary Care in Cost-Effectiveness
Multidisciplinary care, involving collaboration among surgeons, dentists, nurses, and other healthcare professionals, is essential for optimizing outcomes and reducing costs in maxillofacial trauma. A coordinated approach ensures that patients receive comprehensive care, addressing both the physical and psychological aspects of their injuries.
11.1. How does a multidisciplinary approach improve patient outcomes?
A multidisciplinary approach ensures that patients receive comprehensive and coordinated care, addressing all aspects of their injuries. Surgeons can address the physical trauma, while dentists can manage dental injuries and restore oral function. Nurses provide essential bedside care and monitor patients for complications. Psychologists can offer support to help patients cope with the emotional impact of their injuries.
11.2. What are the cost benefits of multidisciplinary care?
Multidisciplinary care can lead to improved patient outcomes, reduced complication rates, and shorter hospital stays, resulting in significant cost savings. A coordinated approach can also prevent duplication of services and ensure that patients receive the most appropriate and cost-effective treatment. By addressing all aspects of the patient’s needs, multidisciplinary care can enhance their overall well-being and reduce the long-term burden of their injuries.
12. Future Directions in Maxillofacial Trauma Cost Analysis
Future research should focus on developing more sophisticated cost analysis models that incorporate both direct and indirect costs. Studies should also explore the cost-effectiveness of different prevention and treatment strategies, providing evidence-based guidance for healthcare policy. Additionally, there is a need for more research on the impact of socioeconomic factors on maxillofacial trauma costs, informing targeted interventions to reduce inequalities.
12.1. What are the emerging trends in cost analysis methodologies?
Emerging trends in cost analysis methodologies include the use of big data analytics, machine learning, and predictive modeling. These techniques can help identify patterns and predict outcomes, allowing healthcare providers to make more informed decisions about resource allocation. Additionally, there is a growing emphasis on incorporating patient-reported outcomes and quality-of-life measures into cost analysis.
12.2. How can technology improve cost analysis and management of maxillofacial trauma?
Technology can play a significant role in improving cost analysis and management of maxillofacial trauma. Electronic health records (EHRs) can facilitate data collection and analysis, while telemedicine can improve access to care and reduce travel costs. Additionally, 3D printing and virtual reality technologies can enhance surgical planning and training, leading to better outcomes and lower costs.
13. Accessing Resources and Support
Understanding the complexities of maxillofacial trauma costs can be daunting, but numerous resources are available to help. Websites like COMPARE.EDU.VN offer detailed comparisons and information to assist in making informed decisions. Support groups and community organizations provide valuable assistance to patients and families affected by these injuries.
13.1. Where can one find detailed cost comparisons?
Detailed cost comparisons can be found on websites like COMPARE.EDU.VN, which provides in-depth analyses of various healthcare costs, including those associated with maxillofacial trauma. These platforms offer valuable insights into the financial aspects of different treatment options, helping individuals and healthcare providers make informed decisions.
13.2. What support systems are available for maxillofacial trauma patients and their families?
Support systems for maxillofacial trauma patients and their families include patient advocacy groups, mental health services, and rehabilitation programs. These resources can provide emotional support, practical assistance, and guidance throughout the recovery process. Additionally, community organizations may offer financial assistance and other forms of support to help patients and families cope with the challenges of maxillofacial trauma.
14. Call to Action: Make Informed Decisions with COMPARE.EDU.VN
Navigating the costs associated with maxillofacial trauma in Australia requires a comprehensive understanding of the various factors involved. COMPARE.EDU.VN offers the detailed comparisons and insights needed to make informed decisions. Whether you are a healthcare provider, patient, or family member, take advantage of the resources available at COMPARE.EDU.VN to better manage and understand the financial aspects of maxillofacial trauma.
For further information and assistance, contact us at:
Address: 333 Comparison Plaza, Choice City, CA 90210, United States
Whatsapp: +1 (626) 555-9090
Website: COMPARE.EDU.VN
By understanding the comparative costs and available resources, you can take proactive steps towards better management and prevention of maxillofacial trauma.
15. Frequently Asked Questions (FAQs)
15.1. What is maxillofacial trauma?
Maxillofacial trauma refers to any physical injury to the face, including fractures, lacerations, and soft tissue damage. These injuries can result from various causes, such as assaults, RTAs, falls, and sports-related incidents.
15.2. What are the main causes of maxillofacial trauma in Australia?
The main causes of maxillofacial trauma in Australia include assaults, road traffic accidents (RTAs), falls, sports-related injuries, and workplace accidents.
15.3. How does socioeconomic status affect the risk of maxillofacial trauma?
Socioeconomic status significantly influences the risk of maxillofacial trauma. Individuals from disadvantaged backgrounds are more likely to sustain injuries from assaults, while those from affluent backgrounds may experience injuries from sports or recreational activities.
15.4. What are the direct costs of treating maxillofacial trauma?
Direct costs include expenses for hospitalization, surgical procedures, medications, imaging, and follow-up care.
15.5. What are the indirect costs associated with maxillofacial trauma?
Indirect costs include lost wages, reduced productivity, travel expenses, and psychological support.
15.6. How can violence prevention programs reduce maxillofacial trauma?
Violence prevention programs address the root causes of violence, reducing rates of assault and interpersonal violence, which in turn lowers the incidence of maxillofacial injuries.
15.7. What is ORIF and how does it contribute to treatment costs?
ORIF (Open Reduction and Internal Fixation) is a surgical procedure used to stabilize fractured bones. It contributes to treatment costs due to the need for specialized equipment, skilled surgeons, and anesthesia.
15.8. How do trauma registries help in analyzing costs associated with maxillofacial trauma?
Trauma registries collect detailed data on patient injuries, treatments, and outcomes, which can be used to perform cost analysis and identify factors influencing healthcare expenditure.
15.9. What is the role of multidisciplinary care in treating maxillofacial trauma?
Multidisciplinary care involves collaboration among surgeons, dentists, nurses, and psychologists to ensure comprehensive care, improving patient outcomes and reducing costs.
15.10. Where can I find more information on maxillofacial trauma costs?
More information can be found on websites like compare.edu.vn, which provides detailed comparisons and analyses of healthcare costs.
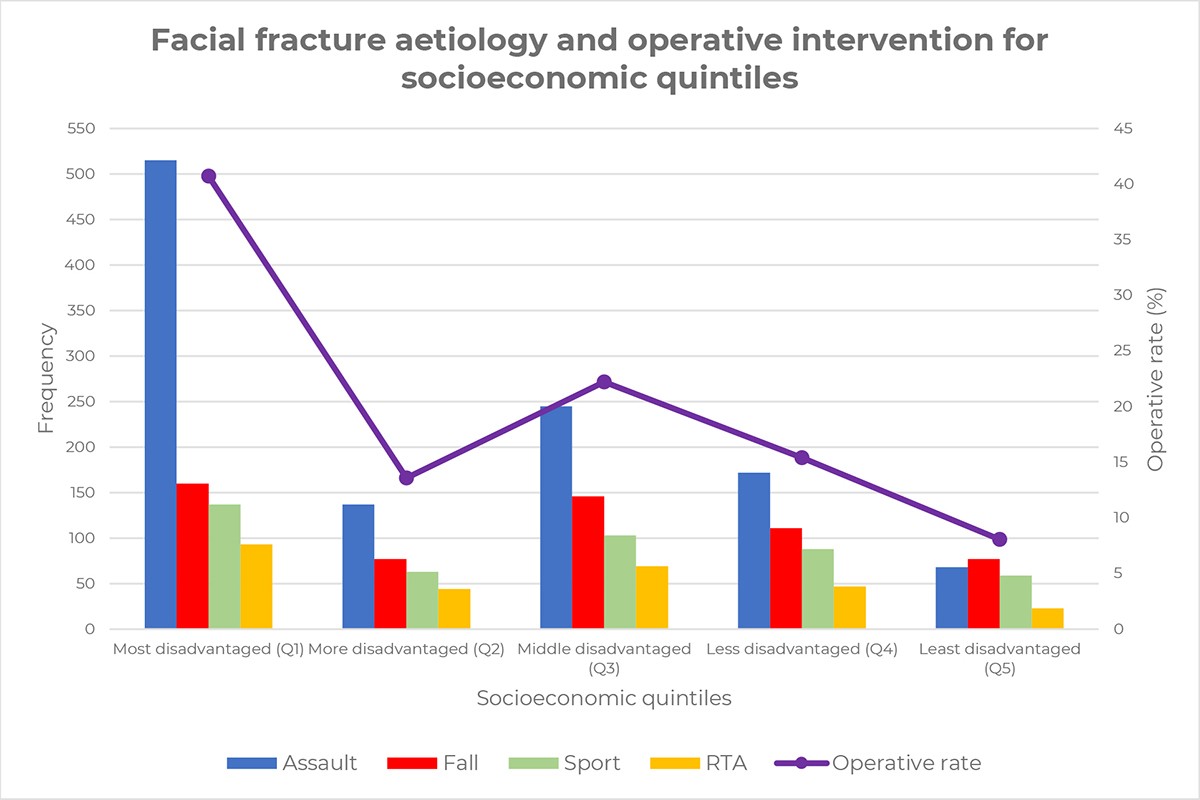 Fig 2 Facial fracture aetiology and operative intervention for socioeconomic quintiles
Fig 2 Facial fracture aetiology and operative intervention for socioeconomic quintiles
This study underscores the significant impact of socioeconomic disparities on the etiology and operative intervention rates in facial fractures, urging targeted public health strategies.