Breast cancer screening mammography is a vital tool for all women, irrespective of their race, ethnicity, or breast cancer risk. Mammograms, combined with subsequent tests and treatment when necessary, significantly improve the chances of surviving breast cancer.
However, access to and utilization of screening mammography are not uniform across all populations. Significant disparities exist in breast cancer screening rates within the U.S., influenced by a complex interplay of factors. Understanding these inequities is the first step towards achieving health equity.
Learn more about Susan G. Komen®’s initiatives to advance health equity.
The Role of Health Insurance in Screening Access
Health insurance coverage is a primary determinant of whether women receive screening mammograms.
Women without health insurance are considerably less likely to undergo screening mammography compared to those with coverage.
Data from 2021 reveals disparities among women aged 50-74 [162]:
- Only 42% of uninsured women had a mammogram within the past two years.
- 71% of women with Medicaid or other public insurance had a mammogram in the same timeframe.
- A higher 80% of women with private health insurance were screened in the past two years.
For women aged 65 and older in 2021 [162]:
- 75% of Medicare beneficiaries had received a screening mammogram within the last two years.
While lack of insurance is a major barrier, it’s not the only factor. Even among insured women aged 50-74, a notable percentage (20-29%) did not receive recent mammograms [162], indicating other obstacles are at play.
The Affordable Care Act, since September 2010, mandates that new health insurance plans cover screening mammograms without co-pays [19]. This coverage extends to mammograms every two years for women 50 and older, and as recommended by healthcare providers for women aged 40-49 [19].
Explore further details on Medicare, Medicaid, and private insurance coverage for mammograms.
Find resources for accessing low-cost or free mammograms.
Learn more about health insurance options.
Beyond Insurance: Additional Barriers to Screening
Beyond financial constraints, numerous other barriers impede access to mammography screening [65, 115-120, 162]:
- Financial Concerns: Low income and anxiety about screening costs.
- Access to Care: Limited transportation to mammography centers, particularly in rural areas.
- Healthcare Access: Lack of a consistent healthcare provider.
- Provider Recommendation: Absence of a healthcare provider’s recommendation for mammography.
- Education Levels: Lower levels of education correlate with lower screening rates.
- Knowledge Gaps: Insufficient understanding of breast cancer risks and screening methods.
- Caregiving Responsibilities: Lack of childcare or eldercare support.
- Workplace Limitations: Lack of sick leave or inability to take time off work.
- Fear and Anxiety: Fear of receiving bad news or experiencing pain during mammography.
- Immigration Status: Recent immigrants (in the U.S. for less than 10 years) may face additional hurdles.
- Cultural and Language Differences: Cultural beliefs and language barriers can impact screening uptake.
These factors contribute to disparities in screening rates across diverse populations, including racial and ethnic groups and women in different geographic locations. For instance, women in rural areas, often facing healthcare access challenges, are less likely to be screened compared to urban counterparts [121].
Racial and Ethnic Disparities in Screening Rates
Mammography screening rates exhibit variations across racial and ethnic groups in the U.S. (refer to Figure 3.6 below).
Figure 3.6: Mammography Rates by Race and Ethnicity (2021)
| Race/Ethnicity | Percentage of women ages 50-74 screened in the past 2 years (2021) |
|---|---|
| Black | 82% |
| White | 76% |
| Hispanic | 74% |
| Asian | 67% |
| American Indian/Alaska Native | 59% |
| Adapted from American Cancer Society [162]. |
Breast Cancer in Black Women
In 2021, Black women demonstrated higher mammography screening rates compared to other groups [162].
While the overall breast cancer incidence rate is lower in Black women than White women [174], a stark disparity exists in mortality rates.
Breast cancer mortality is significantly higher among Black women compared to White women (see Figure 3.7 below) [175].
For example, from 2018-2021, the breast cancer mortality rate was approximately 37% higher for Black women than White women [175].
Figure 3.7: Breast Cancer Incidence vs. Mortality: Black Women Compared to White Women
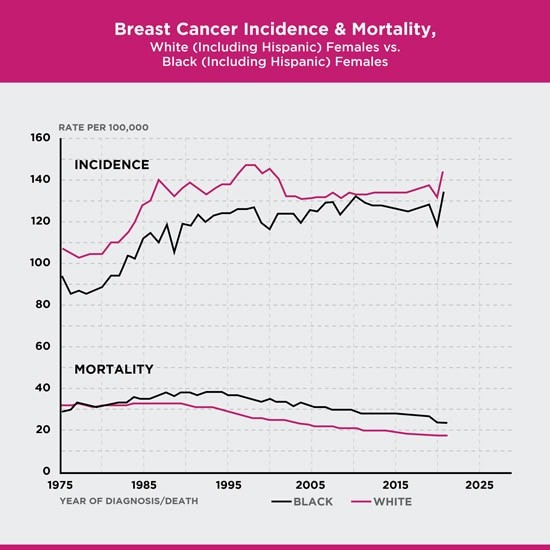 Figure 1.2 Breast Cancer Incidence and Mortality Between Black Women and White Women
Figure 1.2 Breast Cancer Incidence and Mortality Between Black Women and White Women
Figure comparing breast cancer incidence and mortality rates between Black and White women. Black women, despite lower incidence, face significantly higher mortality rates.
Age-adjusted to the 2000 U.S. standard population. Source: 1975-2022 SEER data, 2024 [176-177]
Follow-up Care Disparities for Black Women
Disparities in access to timely follow-up care after abnormal mammograms may contribute to the survival gap between Black and White women.
Research suggests that Black women may experience greater delays in receiving follow-up care after an abnormal mammogram than White women [128-130].
These delays in follow-up can negatively impact survival rates for Black women [131].
Other Factors Influencing Survival in Black Women
Even when considering income and healthcare access, Black women are more likely to be diagnosed with advanced-stage breast cancer and experience poorer survival outcomes compared to White women [131-133, 186].
Learn more about factors impacting breast cancer risk and survival in Black women: factors that may impact breast cancer risk and survival among Black women.
Learn about Susan G. Komen®’s work in advancing health equity.
Read the Stand for H.E.R. – A Healthy Equity Revolution breast cancer impact report.
Younger Age at Diagnosis for Black Women
Black women are often diagnosed with breast cancer at a younger age than White women [178].
From 2017-2021, the median age at diagnosis for Black women was 61, compared to 65 for White women [178]. This younger age at diagnosis highlights the importance of early screening for Black women.
Breast Cancer in Hispanic/Latina Women
In 2021, Hispanic women had mammography screening rates comparable to White women, but lower than Black women (see Figure 3.6) [162].
However, research indicates Hispanic women may encounter more barriers to mammography screening than women of other ethnicities [116, 120].
Screening Variations within Hispanic/Latina Groups
Screening rates among Hispanic/Latina women differ based on their specific origin. For instance, women of Central/South American origin exhibit higher screening rates compared to Mexican American women [136].
Importance of Mammography for Hispanic/Latina Women
While Hispanic women have lower rates of breast cancer and mortality compared to Black and White women [174-175], breast cancer remains the most common cancer and leading cause of cancer death in this population [136, 187]. Hispanic women are also more likely to be diagnosed with advanced-stage breast cancer than White women [136]. Therefore, mammography is equally critical for Hispanic/Latina women.
Breast Cancer in Asian American, Native Hawaiian, and Pacific Islander Women
Asian American women in the U.S. had the lowest mammography screening rates in 2021 compared to Black, White, and Hispanic women [162].
Furthermore, Asian women experience longer delays in follow-up care after abnormal mammograms compared to White women [141].
Non-Hispanic Asian and Pacific Islander women generally have lower breast cancer incidence and mortality rates than Black and White women [174-175]. However, breast cancer is still the second leading cause of cancer death for these women (lung cancer is the first) [187]. Mammography remains a vital screening tool for Asian American, Native Hawaiian, and Pacific Islander women.
Breast Cancer in Native American and Alaska Native Women
In 2021, American Indian and Alaska Native women had the lowest reported breast cancer screening rates [162].
Among women aged 50-74, only 59% of American Indian and Alaska Native women had a mammogram in the past two years, compared to 82% of Black women and 76% of White women (see Figure 3.6) [162].
Limited access to healthcare facilities, often requiring long travel distances, is a significant barrier for these communities [137].
Screening Variations within Native American and Alaska Native Groups
Mammography rates within these communities vary geographically. Women in the Southern Plains and Alaska have higher rates than those on the Pacific Coast [1].
Importance of Mammography for Native American and Alaska Native Women
Breast cancer is the most common cancer among American Indian and Alaska Native women [187]. While incidence and mortality are generally lower than in Black and White women [174-175], diagnosis at later stages is more common compared to White women [179]. Breast cancer rates also vary significantly by region within these populations.
Breast Cancer in LGBTQ+ Individuals
Listen to the Real Pink podcast episode: Breast Health in the LGBTQ+ Community.
Mammography screening rates for lesbians and bisexual women are similar to those of heterosexual women [162, 165].
In 2021 [162]:
- 78% of gay and lesbian women ages 50-74 had a mammogram in the past 2 years.
- 76% of straight women ages 50-74 had a mammogram in the past 2 years.
Data on transgender and nonbinary individuals is limited.
Some lesbians and bisexual women may still face barriers to regular screening, including [144-145, 165]:
- Lack of insurance.
- Perceived low risk.
- Past negative experiences with healthcare providers (discrimination or insensitivity).
- Mistrust of healthcare systems.
- Difficulty finding inclusive healthcare providers.
Finding a healthcare provider who is sensitive to LGBTQ+ needs is crucial. Resources like the National LGBT Cancer Network offer directories of LGBT-welcoming cancer screening centers.
Regular healthcare visits are essential for discussing breast cancer risk and accessing appropriate screening and care.
Learn about breast cancer screening for transgender people.
Breast Cancer in Women with Physical Disabilities
Women with physical disabilities often receive mammograms less frequently than women without disabilities [146-147]. This is often due to limited access to mammography centers that are physically accessible and equipped to meet their needs [147-149].
Many mammography centers, particularly mobile units, are not designed for women with mobility challenges.
Positive experiences at accessible centers increase the likelihood of women with disabilities returning for routine screenings [150].
If accessibility is a concern, contacting local mammography centers to find one that accommodates specific needs is recommended. Partnering with healthcare providers can also aid in this search.
If access for women with disabilities is limited in a community, raising awareness with local medical centers can help drive improvements.
The CDC provides a tip sheet for breast cancer screening for women with disabilities.
Advocacy and Action
Women with disabilities are best positioned to advocate for improvements in mammography centers, medical equipment, and patient-provider interactions. Voice your concerns to local medical centers, insurance companies, and elected officials to push for better healthcare access for people with disabilities. With approximately 36 million women in the U.S. having a physical disability [151], collective action can be powerful.
| Susan G. Komen® Initiatives |
|---|
| Komen collaborates with the American Association on Health and Disability (AAHD) to address and eliminate barriers to breast cancer screening and treatment for women with disabilities. Project Accessibility USA, a joint initiative, aims to enhance care and ensure equitable access to high-quality breast cancer care for all women with disabilities. |
Overcoming Screening Barriers
Numerous barriers can hinder women’s access to breast cancer screening and timely follow-up care. Improving access, raising awareness, and promoting cultural sensitivity are crucial steps in dismantling these barriers, particularly for low-income and uninsured women. Key strategies include [65, 120, 152, 162]:
- Expanding access to mammography and primary care services.
- Eliminating financial obstacles to screening.
- Addressing language barriers through interpretation services and culturally tailored materials.
- Implementing community education campaigns to address misconceptions and anxieties surrounding mammography.
- Ensuring healthcare providers are culturally sensitive and responsive to the diverse needs of their patients. A provider’s recommendation is a significant factor in a woman’s decision to get screened.
Impact of the Affordable Care Act
The Affordable Care Act, by mandating no-cost screening mammogram coverage since September 2010 [19], has contributed to reducing disparities. Gaps in mammography screening between high- and low-income women, as well as between women with high and low education levels, have narrowed since its implementation [153].
Find resources for low-cost or free mammograms.
Open Communication with Healthcare Providers
Komen advocates for accessible, regular mammography screening for all women, guided by shared decision-making between women and their healthcare providers based on individual risk factors.
Learn more about communicating effectively with your healthcare provider.
Timely Follow-up Care is Essential
If a mammogram reveals abnormalities, prompt follow-up testing is crucial to determine if breast cancer is present. Patient navigators at medical centers can assist in coordinating follow-up appointments. Early detection and treatment significantly improve survival chances for breast cancer.
Learn more about follow-up procedures after an abnormal mammogram.
| Susan G. Komen® Support Resources |
|---|
Updated 01/30/25