Are Compared To Is a critical aspect of understanding global healthcare systems. COMPARE.EDU.VN offers comprehensive analyses, revealing disparities in healthcare expenditures, access, and outcomes across nations. Explore comparative healthcare metrics and improve your decision-making. Discover benchmarking, comparative analysis, and international healthcare assessments.
1. Understanding Healthcare Expenditure Comparisons
Healthcare expenditure is a significant indicator of a nation’s investment in the health and well-being of its population. Comparing healthcare costs across different countries is essential to understand the efficiency and effectiveness of various healthcare systems. Several factors influence healthcare expenditure, including economic development, population demographics, healthcare policies, and technological advancements. These factors create a complex landscape that requires careful analysis to draw meaningful conclusions.
1.1. Key Factors Influencing Healthcare Spending
Several elements determine how much a country spends on healthcare. These include:
- GDP per Capita: Wealthier countries generally spend more on healthcare.
- Ageing Population: Countries with older populations tend to have higher healthcare costs due to increased needs for geriatric care.
- Healthcare System Structure: Single-payer systems versus multi-payer systems can impact overall spending.
- Technology and Innovation: Advanced medical technologies often come with higher costs.
- Prevalence of Chronic Diseases: Higher rates of chronic diseases can drive up healthcare expenditure.
- Insurance Coverage: The extent of insurance coverage affects access to care and, consequently, spending.
1.2. Methodologies for Comparing Healthcare Costs
To accurately compare healthcare costs across countries, standardized methodologies are essential. Common methods include:
- Per Capita Spending: Total healthcare expenditure divided by the population.
- Percentage of GDP: Healthcare expenditure as a percentage of the Gross Domestic Product (GDP).
- Purchasing Power Parity (PPP): Adjusting for differences in the cost of goods and services to provide a more accurate comparison of real spending.
- Health Account Data: Standardized data collection frameworks like the System of Health Accounts (SHA) by the OECD.
1.3. The Role of COMPARE.EDU.VN in Healthcare Expenditure Analysis
COMPARE.EDU.VN plays a crucial role in providing detailed comparisons of healthcare expenditures. The website offers:
- Comprehensive Data: Access to extensive databases and statistical analyses.
- User-Friendly Interface: Easy-to-understand visualizations and reports.
- Objective Comparisons: Unbiased analyses of healthcare systems and expenditures.
- Expert Insights: Contributions from healthcare economists and policy experts.
2. Examining U.S. Healthcare Spending Compared to Other OECD Countries
The United States consistently spends more on healthcare than other developed nations. Examining how U.S. health spending compares to other OECD (Organisation for Economic Co-operation and Development) countries reveals significant disparities in healthcare costs and outcomes. Understanding these differences is critical for informing policy decisions and improving the efficiency of the U.S. healthcare system.
2.1. Overview of U.S. Healthcare Expenditure
In 2022, the U.S. healthcare expenditure reached $12,555 per person, significantly higher than any other high-income nation. This spending accounts for approximately 16.6% of the U.S. GDP. Despite this high level of investment, the U.S. does not consistently achieve better health outcomes compared to other OECD countries.
2.2. Benchmarking U.S. Healthcare Costs Against OECD Averages
On average, other large, wealthy countries spend about half as much per person on health as the U.S. The average amount spent on health per person in comparable countries is $6,651, highlighting a substantial difference.
2.3. Factors Contributing to Higher U.S. Costs
Several factors contribute to the higher healthcare costs in the U.S.:
- Administrative Costs: Higher administrative overhead compared to other countries.
- Drug Prices: Significantly higher prices for prescription drugs.
- Fee-for-Service Model: Encourages more services, potentially leading to overutilization.
- Technology Adoption: Rapid adoption of expensive medical technologies.
- Insurance Complexity: A fragmented insurance system with multiple payers.
2.4. Visual Representation of Healthcare Spending
This chart illustrates the disparity in healthcare spending per person, with the U.S. significantly exceeding other high-income nations.
3. Trends in Healthcare Spending Across Nations
Analyzing the trends in healthcare spending across different nations provides insights into how various healthcare systems are evolving. Understanding these trends is essential for predicting future healthcare costs and developing sustainable healthcare policies. Changes in demographics, technology, and healthcare policies significantly influence these trends.
3.1. Recent Increases in Per Capita Health Spending
In almost all peer nations, health spending per capita increased between 2021 and 2022, with the exception of the Netherlands where spending declined by 0.1%. In the U.S., per capita health spending saw a 2.9% increase, a smaller increase than in most comparable nations, though larger than in Australia (2.4%), Canada (0.7%), and the United Kingdom (0.5%). Belgium had the largest increase in per capita health spending among countries with available data between 2021 and 2022, at 9.6%.
This 2.9% increase in per capita health spending is slightly higher than the previous increase between 2020 and 2021 (2.4%), but still much lower than the 9.8% increase from 2019 to 2020.
3.2. Impact of the COVID-19 Pandemic on Healthcare Spending
The COVID-19 pandemic led to both an increase in health spending and an economic downturn resulting in higher health spending as a share of the GDP in the U.S. and every comparable country between 2019 to 2020. As the economy has recovered since then, health spending as a share of GDP has declined in the U.S. and most other peer nations. In 2020, the U.S. spent 18.8% of its GDP on health-related expenditures, up from 16.7% in 2019. Health spending as a share of GDP in the U.S. declined to 17.4% in 2021 and then 16.6% in 2022—but remains substantially higher than in peer countries.
3.3. Long-Term Trends in Healthcare Spending as a Share of GDP
Over the past five decades, the difference between health spending as a share of the economy in the U.S. and comparable OECD countries has widened. In 1970, the U.S. spent about 6.2% of its GDP on health, similar to spending in several comparable countries (the average of comparably wealthy countries was about 4.9% of GDP in 1970). The U.S. was relatively on pace with other countries until the 1980s, when health spending in the U.S. grew at a significantly faster rate relative to its GDP. Since then, health spending as a share of the economy has grown faster in the U.S. than in peer nations.
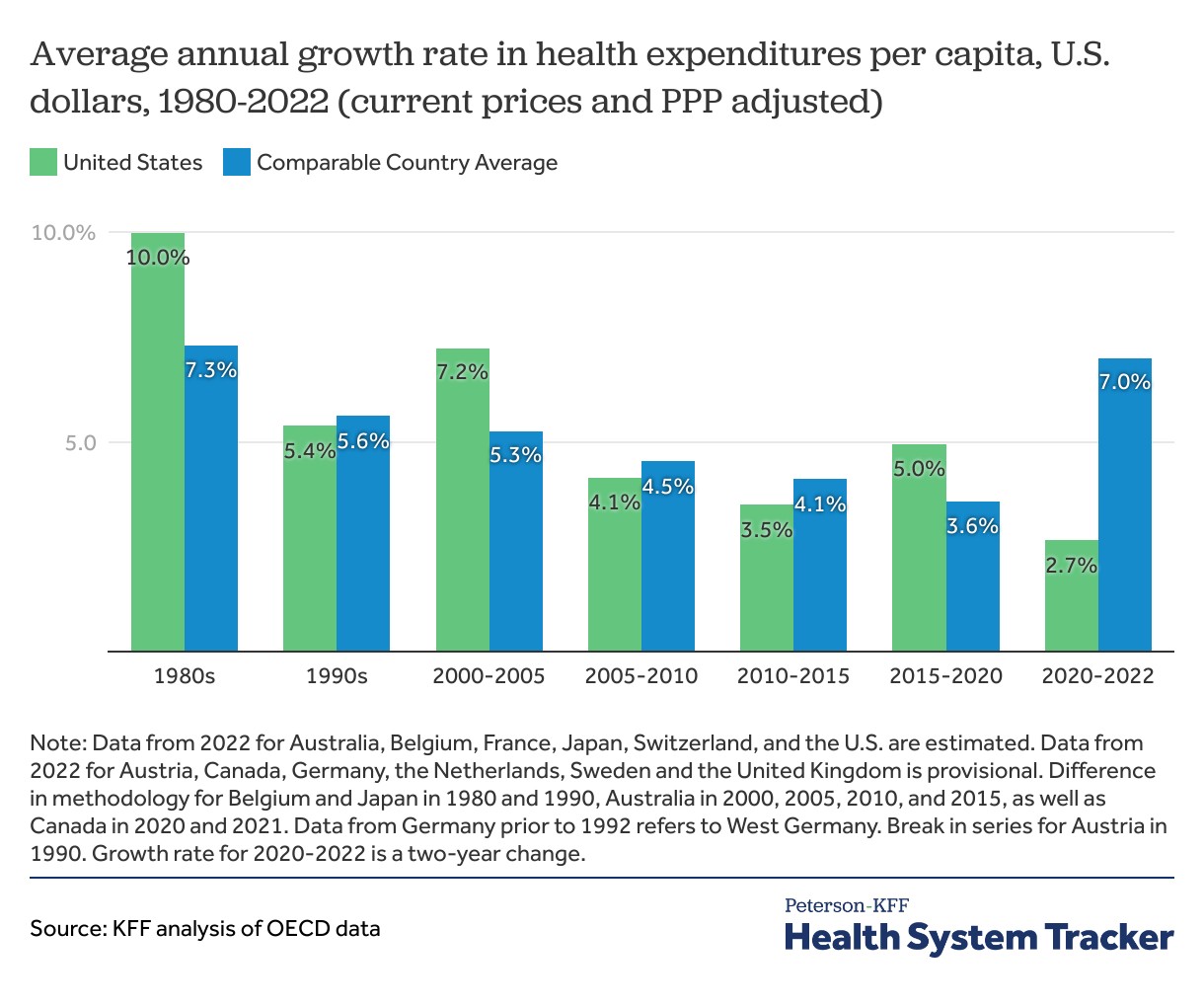
3.4. Comparative Growth Rates in Healthcare Expenditure
While the U.S. has long had higher than average health spending, recent years have seen higher spending growth in other nations. Historically, the 1980s saw accelerated growth in health expenditures per capita in the U.S. The 10.0% average annual growth rate in the U.S. during the 1980s was significantly higher than comparable countries. Comparably wealthy countries saw an average of 7.3% annual growth during this period.
Looking at 5-year growth rates, during the period from 2005-2010, the U.S. saw an average annual growth rate in health spending of 4.1%, compared to 7.2% during the previous five-year period. Comparable countries also saw health spending growth slow down on average, from 4.5% average annual growth during the 2005-2010 period, down from 5.3% during the 2000-2005 period. In the 5 years leading up to the COVID-19 pandemic (2015-2020), the U.S.’s growth in health spending per capita outpaced the average for comparable countries (5.0% versus 3.6%). The annual growth rate for the average of comparable countries increased between 2020 and 2022 to 7.0% versus a 2.7% increase for the U.S. during the same period.
3.5. Visualizing Healthcare Spending Growth
This graph illustrates the trends in healthcare spending growth, highlighting periods of rapid growth and more recent changes influenced by the COVID-19 pandemic.
4. Assessing Healthcare System Efficiency and Effectiveness
Comparing healthcare costs is only part of the picture; assessing the efficiency and effectiveness of healthcare systems is equally important. Efficiency refers to how well resources are used to deliver healthcare services, while effectiveness measures the extent to which these services improve health outcomes. A system can be efficient but not effective, or vice versa.
4.1. Key Metrics for Evaluating Healthcare System Performance
Several key metrics are used to evaluate the performance of healthcare systems:
- Life Expectancy: Average number of years a person is expected to live.
- Infant Mortality Rate: Number of deaths per 1,000 live births.
- Maternal Mortality Rate: Number of maternal deaths per 100,000 live births.
- Mortality Rates for Specific Diseases: Rates for conditions like heart disease, cancer, and diabetes.
- Access to Care: Proportion of the population with access to necessary healthcare services.
- Quality of Care: Measures such as patient satisfaction, adherence to clinical guidelines, and preventable hospital admissions.
4.2. Comparing Health Outcomes in the U.S. and Other Developed Nations
Despite its high healthcare spending, the U.S. often lags behind other developed nations in key health outcomes. For example, life expectancy in the U.S. is lower than the OECD average, and infant mortality rates are higher. This discrepancy suggests that the U.S. healthcare system may not be as efficient or effective as those in other countries.
4.3. Factors Affecting Healthcare System Efficiency and Effectiveness
Several factors can impact the efficiency and effectiveness of a healthcare system:
- Healthcare Policies: Government regulations and policies influencing healthcare delivery.
- System Structure: Whether the system is single-payer, multi-payer, or a mix of both.
- Preventive Care: Emphasis on preventive services and early detection of diseases.
- Care Coordination: How well different parts of the healthcare system work together.
- Health Disparities: Differences in health outcomes among different population groups.
4.4. The Role of COMPARE.EDU.VN in Assessing Healthcare System Performance
COMPARE.EDU.VN provides tools and resources to assess healthcare system performance:
- Data Visualization: Interactive charts and graphs illustrating key metrics.
- Comparative Analyses: Reports comparing different healthcare systems.
- Expert Commentary: Insights from healthcare professionals and researchers.
- Policy Recommendations: Evidence-based recommendations for improving healthcare system performance.
4.5. Visualizing Health Outcomes
This chart visually represents the differences in life expectancy, highlighting the U.S.’s position compared to other nations.
5. The Influence of Healthcare Policies and Systems
Healthcare policies and systems play a crucial role in shaping healthcare expenditure and outcomes. Different countries adopt varying approaches to healthcare, ranging from single-payer systems to multi-payer models. Understanding these differences is essential for evaluating the impact of policies on healthcare costs and quality.
5.1. Overview of Different Healthcare Systems
- Single-Payer Systems: Typically funded by taxes and administered by the government. Examples include Canada and the United Kingdom.
- Multi-Payer Systems: Funded by a combination of public and private sources, with multiple insurance providers. The U.S. is an example of a multi-payer system.
- Social Health Insurance Systems: Funded by mandatory contributions from employers and employees, with non-profit insurance funds. Germany and France are examples.
5.2. How Policies Impact Healthcare Spending and Outcomes
Healthcare policies can influence spending and outcomes in several ways:
- Price Controls: Policies aimed at controlling the prices of drugs and medical services.
- Insurance Mandates: Requirements for individuals or employers to provide health insurance.
- Regulation of Healthcare Providers: Policies affecting the supply and distribution of healthcare providers.
- Investment in Public Health: Policies supporting preventive care and public health initiatives.
5.3. Case Studies of Policy Impact
- Canada: A single-payer system that provides universal healthcare coverage, resulting in lower administrative costs but potential wait times for certain procedures.
- Germany: A social health insurance system with mandatory contributions, leading to high levels of coverage and quality of care but higher labor costs for employers.
- United Kingdom: The National Health Service (NHS) provides healthcare to all residents, funded by taxes. This results in universal access but potential resource constraints.
- United States: A multi-payer system with a mix of public and private insurance. This leads to high levels of innovation and choice but also high costs and unequal access.
5.4. The Role of COMPARE.EDU.VN in Policy Analysis
COMPARE.EDU.VN offers valuable resources for analyzing the impact of healthcare policies:
- Policy Briefs: Summaries of key policy issues and their potential impact.
- Comparative Data: Data comparing healthcare systems and outcomes under different policy regimes.
- Expert Analysis: Insights from policy experts on the effectiveness of different policies.
- Interactive Tools: Tools for modeling the potential impact of policy changes.
6. Technology and Innovation in Healthcare
Technology and innovation play a significant role in shaping healthcare costs and outcomes. Advances in medical technology can improve the quality of care and lead to better health outcomes, but they often come with higher costs. Understanding the impact of technology on healthcare is essential for making informed decisions about healthcare investments.
6.1. Impact of Medical Technology on Healthcare Costs
- New Diagnostic Tools: Advanced imaging technologies like MRI and CT scans can improve diagnostic accuracy but are expensive.
- Minimally Invasive Procedures: Surgical techniques that reduce recovery times but require specialized equipment.
- Robotic Surgery: Enhances precision and reduces complications but involves high upfront costs.
- Personalized Medicine: Tailoring treatments to individual patients based on genetic information, which can be costly but more effective.
6.2. Telehealth and Digital Health Solutions
Telehealth and digital health solutions offer the potential to improve access to care and reduce costs:
- Remote Monitoring: Allows patients to monitor their health conditions from home, reducing the need for hospital visits.
- Virtual Consultations: Provides convenient access to healthcare providers, especially in rural areas.
- Mobile Health Apps: Helps patients manage their health and track their progress.
- Electronic Health Records (EHRs): Improves care coordination and reduces administrative costs.
6.3. Comparative Analysis of Technology Adoption
Countries vary in their adoption of medical technologies. Factors influencing adoption rates include:
- Regulatory Environment: Approval processes for new technologies.
- Reimbursement Policies: How healthcare providers are reimbursed for using new technologies.
- Infrastructure: Availability of necessary infrastructure, such as broadband internet access.
- Cultural Factors: Attitudes towards technology and innovation.
6.4. The Role of COMPARE.EDU.VN in Evaluating Technology Impact
COMPARE.EDU.VN provides resources for evaluating the impact of technology on healthcare:
- Technology Assessments: Reports assessing the clinical and economic impact of new technologies.
- Comparative Data: Data comparing technology adoption rates and their impact on outcomes.
- Expert Insights: Analysis from technology experts on the future of healthcare.
- Case Studies: Examples of successful technology implementation in healthcare.
7. Strategies for Improving Healthcare Value and Efficiency
Improving healthcare value and efficiency is a key goal for healthcare systems worldwide. Value refers to the relationship between the outcomes achieved and the costs incurred. Efficiency refers to how well resources are used to deliver healthcare services. Strategies for improving value and efficiency include:
7.1. Focus on Preventive Care
Investing in preventive care can reduce the incidence of chronic diseases and lower overall healthcare costs:
- Vaccination Programs: Prevents infectious diseases and reduces hospitalizations.
- Screening Programs: Early detection of diseases like cancer and diabetes.
- Health Education: Promotes healthy lifestyles and reduces risk factors.
7.2. Enhance Care Coordination
Improving care coordination can reduce fragmentation and improve outcomes:
- Integrated Care Models: Combines different healthcare services to provide comprehensive care.
- Accountable Care Organizations (ACOs): Groups of healthcare providers who work together to deliver coordinated care.
- Patient-Centered Medical Homes (PCMHs): Primary care practices that provide comprehensive, coordinated care.
7.3. Implement Value-Based Payment Models
Value-based payment models incentivize healthcare providers to deliver high-quality, cost-effective care:
- Bundled Payments: A single payment for all services related to a specific episode of care.
- Pay-for-Performance: Rewards healthcare providers for achieving specific quality and efficiency targets.
- Shared Savings Programs: Allows healthcare providers to share in any cost savings they achieve.
7.4. Reduce Administrative Costs
Reducing administrative costs can free up resources for direct patient care:
- Standardize Billing Practices: Simplifies billing processes and reduces errors.
- Invest in Health IT: Improves efficiency and reduces paperwork.
- Streamline Regulatory Processes: Reduces administrative burden on healthcare providers.
7.5. Promote Price Transparency
Price transparency allows patients to make informed decisions about their healthcare:
- Publish Prices for Common Procedures: Allows patients to compare prices across different providers.
- Provide Cost Estimates: Helps patients understand the costs of their care before they receive it.
7.6. The Role of COMPARE.EDU.VN in Improving Healthcare Value
COMPARE.EDU.VN offers resources for improving healthcare value:
- Best Practices: Examples of successful strategies for improving healthcare value.
- Comparative Data: Data comparing healthcare costs and outcomes across different providers and systems.
- Policy Recommendations: Evidence-based recommendations for improving healthcare value.
- Tools and Resources: Tools for measuring and improving healthcare value.
8. Addressing Health Disparities
Health disparities refer to differences in health outcomes among different population groups. Addressing these disparities is essential for achieving health equity and improving overall population health. Factors contributing to health disparities include socioeconomic status, access to care, and cultural factors.
8.1. Key Factors Contributing to Health Disparities
- Socioeconomic Status: Poverty, lack of education, and unemployment can limit access to healthcare and contribute to poor health outcomes.
- Access to Care: Lack of insurance, transportation, and healthcare providers in certain areas can limit access to necessary healthcare services.
- Cultural Factors: Language barriers, cultural beliefs, and discrimination can affect healthcare utilization and outcomes.
8.2. Strategies for Reducing Health Disparities
- Expand Access to Care: Increase insurance coverage, improve transportation, and increase the availability of healthcare providers in underserved areas.
- Address Social Determinants of Health: Implement policies to reduce poverty, improve education, and promote economic opportunity.
- Improve Cultural Competency: Train healthcare providers to provide culturally sensitive care.
- Increase Community Engagement: Involve community members in the design and implementation of healthcare programs.
8.3. The Role of COMPARE.EDU.VN in Addressing Disparities
COMPARE.EDU.VN provides resources for addressing health disparities:
- Data on Health Disparities: Data illustrating differences in health outcomes among different population groups.
- Best Practices: Examples of successful programs for reducing health disparities.
- Policy Recommendations: Evidence-based recommendations for addressing health disparities.
- Tools and Resources: Tools for measuring and tracking progress in reducing health disparities.
9. Future Trends in Healthcare Spending and Delivery
The healthcare landscape is constantly evolving, with new technologies, policies, and demographic trends shaping the future of healthcare spending and delivery. Understanding these trends is essential for preparing for the challenges and opportunities that lie ahead.
9.1. Aging Population
The global population is aging, which will increase demand for healthcare services and drive up healthcare costs. Strategies for addressing this trend include:
- Promoting Healthy Aging: Encouraging healthy lifestyles and preventive care to reduce the incidence of chronic diseases.
- Expanding Geriatric Care: Increasing the availability of specialized geriatric care services.
- Developing Age-Friendly Communities: Creating communities that support the needs of older adults.
9.2. Technological Advancements
New technologies will continue to transform healthcare, offering the potential to improve outcomes and reduce costs. Key trends include:
- Artificial Intelligence (AI): AI can be used to improve diagnostic accuracy, personalize treatments, and automate administrative tasks.
- Wearable Devices: Wearable devices can monitor health conditions and provide personalized feedback.
- 3D Printing: 3D printing can be used to create customized medical devices and prosthetics.
- Nanotechnology: Nanotechnology can be used to deliver drugs more effectively and diagnose diseases earlier.
9.3. Shift to Value-Based Care
The shift to value-based care will continue to accelerate, with a greater emphasis on improving outcomes and reducing costs. Key trends include:
- Increased Use of Data Analytics: Data analytics can be used to identify opportunities for improving care and reducing costs.
- Greater Collaboration: Healthcare providers will need to collaborate more effectively to deliver coordinated care.
- Focus on Patient Engagement: Patients will need to be more actively involved in their care.
9.4. The Role of COMPARE.EDU.VN in Navigating Future Trends
COMPARE.EDU.VN provides resources for navigating future trends in healthcare:
- Trend Reports: Reports analyzing emerging trends in healthcare.
- Expert Insights: Analysis from healthcare experts on the future of healthcare.
- Scenario Planning: Tools for developing strategies to address future challenges and opportunities.
- Community Forum: A platform for healthcare professionals to share ideas and best practices.
10. Conclusion: Making Informed Decisions with COMPARE.EDU.VN
Understanding how healthcare costs are compared to other metrics is crucial for making informed decisions about healthcare policies, investments, and individual health choices. COMPARE.EDU.VN offers a comprehensive platform for comparing healthcare systems, analyzing trends, and evaluating the impact of policies and technologies. By providing access to reliable data, expert insights, and user-friendly tools, COMPARE.EDU.VN empowers individuals, policymakers, and healthcare professionals to make evidence-based decisions that improve healthcare value and outcomes.
Are compared to is a cornerstone of effective healthcare analysis. COMPARE.EDU.VN excels in this area, providing detailed comparative assessments. Healthcare metrics, comparative analysis, and international healthcare standards are key to understanding the complex landscape. Utilize COMPARE.EDU.VN to make informed decisions.
For more information, visit COMPARE.EDU.VN or contact us at 333 Comparison Plaza, Choice City, CA 90210, United States. Whatsapp: +1 (626) 555-9090.
Are you struggling to compare healthcare options and make informed decisions? Visit COMPARE.EDU.VN for detailed, objective comparisons that help you choose the best solutions for your needs. Don’t navigate the complexities of healthcare alone – let COMPARE.EDU.VN guide you to smarter, more confident choices. Explore COMPARE.EDU.VN today and take control of your healthcare decisions.
FAQ: Frequently Asked Questions
- Why does the U.S. spend so much more on healthcare than other countries? The U.S. has higher administrative costs, drug prices, and technology adoption rates, contributing to higher overall spending.
- How does COMPARE.EDU.VN help in comparing healthcare systems? compare.edu.vn provides comprehensive data, user-friendly interfaces, and objective analyses of healthcare systems.
- What are the key metrics for evaluating healthcare system performance? Key metrics include life expectancy, infant mortality rate, and access to care.
- What role do healthcare policies play in healthcare spending and outcomes? Healthcare policies can influence spending through price controls, insurance mandates, and regulation of providers.
- How can technology improve healthcare value and efficiency? Technology can improve diagnostic accuracy, personalize treatments, and automate administrative tasks.
- What are some strategies for reducing health disparities? Strategies include expanding access to care, addressing social determinants of health, and improving cultural competency.
- How will the aging population impact healthcare spending? An aging population will increase demand for healthcare services and drive up costs.
- What is value-based care, and how does it improve healthcare? Value-based care incentivizes providers to deliver high-quality, cost-effective care.
- How can price transparency help patients make informed decisions? Price transparency allows patients to compare prices across different providers and understand the costs of their care.
- What future trends will shape healthcare spending and delivery? Future trends include technological advancements, the shift to value-based care, and the aging population.