A Compare The Structure Of The Pulmonary And Tricuspid Valves is crucial for understanding their function and addressing related heart conditions. At COMPARE.EDU.VN, we offer a detailed comparison of these valves, providing you with the insights needed to make informed decisions. Explore the structural disparities and similarities between these vital cardiac components.
1. Introduction: Understanding Heart Valve Structures
The human heart, a marvel of biological engineering, relies on a series of valves to ensure unidirectional blood flow, with the pulmonary and tricuspid valves being critical components. The pulmonary valve regulates blood flow from the right ventricle into the pulmonary artery, whereas the tricuspid valve controls flow from the right atrium to the right ventricle. This comparison delves into the intricate structures of both valves, and how these differences impact their function and susceptibility to disease.
1.1. Why Compare the Pulmonary and Tricuspid Valves?
Understanding the structure of heart valves is essential for medical professionals, students, and anyone interested in cardiovascular health. This analysis of the pulmonary and tricuspid valves provides a comprehensive overview that aids in diagnosing and treating valve-related conditions. A clear understanding of the anatomy and function of these valves is vital for informed medical interventions.
1.2. COMPARE.EDU.VN: Your Resource for Detailed Comparisons
At COMPARE.EDU.VN, we provide detailed and objective comparisons to help you make informed decisions. This analysis of the pulmonary and tricuspid valves exemplifies our commitment to providing clear, accurate, and comprehensive information. Our platform is designed to make complex topics accessible and understandable.
2. Anatomical Overview of the Heart Valves
To effectively compare the pulmonary and tricuspid valves, it is essential to understand their respective locations and roles within the heart.
2.1. Location and Function of the Pulmonary Valve
The pulmonary valve is located between the right ventricle and the pulmonary artery. It prevents backflow of blood into the right ventricle during diastole, ensuring that deoxygenated blood flows efficiently to the lungs for oxygenation. Its proper function is vital for maintaining systemic oxygen levels.
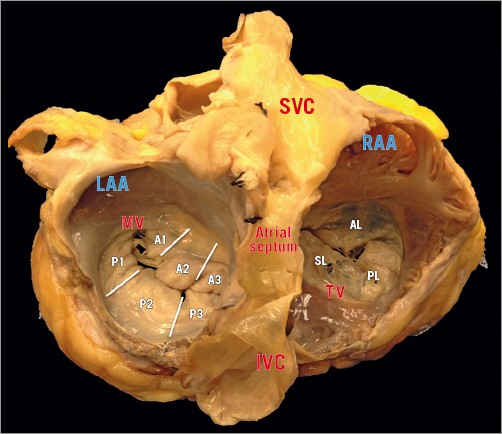
2.2. Location and Function of the Tricuspid Valve
The tricuspid valve is situated between the right atrium and the right ventricle. It prevents backflow of blood into the right atrium during ventricular systole, ensuring that blood moves forward into the pulmonary circulation. Effective tricuspid valve function is critical for maintaining right heart hemodynamics.
3. Detailed Structural Comparison
A detailed structural comparison highlights the similarities and differences between the pulmonary and tricuspid valves, and how these variations influence their respective functions.
3.1. Number of Leaflets
- Pulmonary Valve: The pulmonary valve is a semilunar valve comprising three leaflets or cusps, typically named the anterior, left, and right cusps. These cusps are thinner and more delicate compared to those of the tricuspid valve.
- Tricuspid Valve: The tricuspid valve, as its name suggests, consists of three leaflets: the anterior, posterior, and septal leaflets. These leaflets are larger and more robust than those of the pulmonary valve, reflecting the higher pressures they must withstand.
3.2. Annulus Structure
- Pulmonary Valve: The pulmonary valve annulus is a fibrous ring that supports the valve leaflets. It is relatively smaller and more circular compared to the tricuspid annulus.
- Tricuspid Valve: The tricuspid valve annulus is larger and more elliptical. It is also dynamic, changing shape during the cardiac cycle to optimize valve function. The annulus is less rigid, which contributes to its susceptibility to dilation in conditions like tricuspid regurgitation.
3.3. Chordae Tendineae and Papillary Muscles
- Pulmonary Valve: The pulmonary valve is unique among heart valves because it typically lacks chordae tendineae and papillary muscles. The valve cusps are supported by the shape and flexibility of the valve leaflets themselves.
- Tricuspid Valve: The tricuspid valve has chordae tendineae, fibrous cords that attach the valve leaflets to the papillary muscles within the right ventricle. The papillary muscles (anterior, posterior, and septal) prevent the leaflets from prolapsing into the right atrium during ventricular contraction.
3.4. Tissue Composition
- Pulmonary Valve: The pulmonary valve leaflets are composed of thin, pliable tissue that allows for easy opening and closing. This design is suited to the lower-pressure environment of the right ventricle and pulmonary artery.
- Tricuspid Valve: The tricuspid valve leaflets are thicker and more fibrous to withstand the mechanical stress from the higher pressures in the right ventricle. This robust structure ensures valve competence throughout the cardiac cycle.
3.5. Spatial Orientation
- Pulmonary Valve: The pulmonary valve is positioned at the entrance to the pulmonary artery, directing blood away from the heart towards the lungs. It is oriented superiorly and anteriorly relative to the other heart valves.
- Tricuspid Valve: The tricuspid valve is located between the right atrium and right ventricle, oriented horizontally within the heart. Its position is medial to the mitral valve on the left side of the heart.
4. Functional Implications of Structural Differences
The structural differences between the pulmonary and tricuspid valves have significant functional implications, affecting their roles in cardiac physiology and susceptibility to disease.
4.1. Hemodynamic Function
- Pulmonary Valve: The pulmonary valve’s primary function is to ensure unidirectional blood flow to the lungs. Its structure, with thin cusps and lack of chordae tendineae, allows for efficient opening and closing under low-pressure conditions.
- Tricuspid Valve: The tricuspid valve is responsible for maintaining proper blood flow between the right atrium and ventricle. Its larger leaflets, supported by chordae tendineae and papillary muscles, withstand the higher pressures generated during ventricular contraction, preventing backflow.
4.2. Susceptibility to Disease
- Pulmonary Valve: Pulmonary valve stenosis and regurgitation are relatively rare compared to tricuspid valve disorders. Congenital abnormalities are the most common cause of pulmonary valve disease.
- Tricuspid Valve: Tricuspid regurgitation is a common condition, often secondary to left-sided heart failure. The tricuspid valve’s larger size, dynamic annulus, and complex subvalvular apparatus make it more prone to dysfunction.
4.3. Response to Pressure Overload
- Pulmonary Valve: The pulmonary valve can develop stenosis due to calcification or congenital defects, leading to increased right ventricular pressure. This can result in right ventricular hypertrophy and eventual heart failure.
- Tricuspid Valve: The tricuspid valve is highly susceptible to dilation and dysfunction due to chronic pressure overload from pulmonary hypertension or left-sided heart failure. This leads to tricuspid regurgitation, which further exacerbates right heart failure.
5. Imaging Techniques for Valve Assessment
Various imaging techniques are used to assess the structure and function of the pulmonary and tricuspid valves, providing valuable information for diagnosis and treatment planning.
5.1. Echocardiography
Echocardiography, including transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE), is the primary imaging modality for evaluating heart valves. It provides real-time visualization of valve structure and function, allowing for assessment of stenosis, regurgitation, and valve morphology.
- Pulmonary Valve: Echocardiography can effectively assess pulmonary valve stenosis and regurgitation, measuring pressure gradients across the valve and quantifying the severity of regurgitation.
- Tricuspid Valve: Echocardiography is crucial for diagnosing and grading tricuspid regurgitation. It can also assess tricuspid valve stenosis, although this is less common. TEE provides better visualization of the tricuspid valve compared to TTE.
5.2. Cardiac Magnetic Resonance Imaging (MRI)
Cardiac MRI offers detailed anatomical and functional information about the heart valves, including valve area, regurgitant fraction, and ventricular volumes.
- Pulmonary Valve: MRI is useful for assessing pulmonary valve stenosis and regurgitation, especially in patients with poor echocardiographic windows or complex congenital heart disease.
- Tricuspid Valve: MRI can accurately quantify tricuspid regurgitation and assess the impact on right ventricular size and function. It also provides detailed anatomical information about the tricuspid valve annulus and leaflets.
5.3. Computed Tomography (CT) Scanning
CT scanning provides high-resolution anatomical images of the heart valves, particularly useful for pre-procedural planning for valve interventions.
- Pulmonary Valve: CT scanning can visualize pulmonary valve morphology and assess for calcification or other structural abnormalities.
- Tricuspid Valve: CT scanning is used to evaluate the tricuspid valve annulus and surrounding structures before transcatheter valve interventions. It helps in determining valve size and selecting appropriate device dimensions.
6. Clinical Implications and Treatment Strategies
Understanding the structural and functional differences between the pulmonary and tricuspid valves is essential for guiding clinical decision-making and selecting appropriate treatment strategies.
6.1. Pulmonary Valve Disease
- Pulmonary Stenosis: Mild pulmonary stenosis may not require treatment, while severe stenosis typically requires intervention. Balloon valvuloplasty is the preferred treatment for congenital pulmonary stenosis. Surgical valve replacement may be necessary in cases of severe valve disease or associated anomalies.
- Pulmonary Regurgitation: Mild pulmonary regurgitation is often well-tolerated. Significant regurgitation can lead to right ventricular dilatation and dysfunction, requiring pulmonary valve replacement.
6.2. Tricuspid Valve Disease
- Tricuspid Regurgitation: Management of tricuspid regurgitation depends on the severity of regurgitation and associated symptoms. Diuretics are used to manage symptoms of fluid overload. Surgical tricuspid valve repair or replacement may be necessary in severe cases. Transcatheter tricuspid valve repair devices are emerging as less invasive alternatives for high-risk patients.
- Tricuspid Stenosis: Tricuspid stenosis is rare and often associated with rheumatic heart disease. Treatment involves managing symptoms and addressing the underlying cause. Surgical valve repair or replacement may be necessary in severe cases.
6.3. Interventional Approaches
- Transcatheter Pulmonary Valve Replacement (TPVR): TPVR is a minimally invasive procedure used to replace the pulmonary valve using a catheter-based approach. It is an effective alternative to surgical valve replacement in selected patients with pulmonary valve dysfunction.
- Transcatheter Tricuspid Valve Repair (TTVR): TTVR devices aim to reduce tricuspid regurgitation by clipping leaflets together or by placing a valve within the existing tricuspid valve. These procedures offer a less invasive option for patients who are not candidates for surgery.
7. Emerging Technologies and Future Directions
The field of heart valve therapy is rapidly evolving, with new technologies and treatment strategies emerging to improve outcomes for patients with pulmonary and tricuspid valve disease.
7.1. Novel Imaging Techniques
Advanced imaging techniques, such as 3D echocardiography and computational flow dynamics, provide more detailed assessment of valve structure and function, allowing for better diagnosis and treatment planning.
7.2. Next-Generation Transcatheter Valves
Next-generation transcatheter valves are being designed to address the limitations of current devices, with improved durability, hemodynamics, and ease of implantation.
7.3. Personalized Treatment Strategies
Personalized treatment strategies based on individual patient characteristics and valve morphology are being developed to optimize outcomes and minimize complications.
8. Conclusion: Informed Decisions with COMPARE.EDU.VN
Understanding the structural differences between the pulmonary and tricuspid valves is essential for healthcare professionals, students, and patients. By providing detailed and objective comparisons, COMPARE.EDU.VN empowers you to make informed decisions about your health. Explore our comprehensive resources to deepen your understanding of heart valve disease and its management.
8.1. Summary of Key Differences
The pulmonary and tricuspid valves differ significantly in their structure, function, and susceptibility to disease. The pulmonary valve, with its thin cusps and lack of chordae tendineae, is adapted for low-pressure pulmonary circulation. The tricuspid valve, with its larger leaflets, chordae tendineae, and dynamic annulus, is designed to withstand higher pressures in the right heart.
8.2. Call to Action: Explore COMPARE.EDU.VN for More Insights
For more detailed comparisons and objective information on heart valve disease and other medical conditions, visit COMPARE.EDU.VN. Our platform offers a wealth of resources to help you make informed decisions about your health.
Navigating complex medical information can be challenging, but COMPARE.EDU.VN is here to help. Contact us at 333 Comparison Plaza, Choice City, CA 90210, United States, or reach out via Whatsapp at +1 (626) 555-9090. Visit our website at compare.edu.vn for comprehensive comparisons and insights.
9. Frequently Asked Questions (FAQs)
9.1. What is the main function of the pulmonary valve?
The pulmonary valve controls blood flow from the right ventricle into the pulmonary artery, ensuring that deoxygenated blood flows efficiently to the lungs for oxygenation.
9.2. How does the tricuspid valve differ from the pulmonary valve in structure?
The tricuspid valve has three leaflets, chordae tendineae, and papillary muscles, while the pulmonary valve has three thinner cusps and lacks chordae tendineae and papillary muscles.
9.3. Why is tricuspid regurgitation more common than pulmonary regurgitation?
The tricuspid valve is more susceptible to dilation and dysfunction due to chronic pressure overload from pulmonary hypertension or left-sided heart failure.
9.4. What imaging techniques are used to assess the pulmonary and tricuspid valves?
Echocardiography, cardiac MRI, and CT scanning are commonly used to assess the structure and function of these valves.
9.5. What is transcatheter pulmonary valve replacement (TPVR)?
TPVR is a minimally invasive procedure used to replace the pulmonary valve using a catheter-based approach.
9.6. How is tricuspid regurgitation treated?
Treatment options include diuretics to manage symptoms, surgical valve repair or replacement, and transcatheter tricuspid valve repair (TTVR) for high-risk patients.
9.7. What are chordae tendineae and what is their function?
Chordae tendineae are fibrous cords that attach the valve leaflets to the papillary muscles within the ventricles, preventing the leaflets from prolapsing into the atria during ventricular contraction.
9.8. What is the annulus of a heart valve?
The annulus is a fibrous ring that supports the valve leaflets and maintains the structural integrity of the valve.
9.9. How does pulmonary stenosis affect the heart?
Pulmonary stenosis can lead to increased right ventricular pressure, resulting in right ventricular hypertrophy and eventual heart failure.
9.10. What emerging technologies are being developed for heart valve therapy?
Emerging technologies include advanced imaging techniques, next-generation transcatheter valves, and personalized treatment strategies to optimize outcomes.