Cloth masks are widely used in healthcare settings, particularly in resource-limited environments. However, their efficacy in preventing respiratory infections compared to medical masks remains a critical question. This article analyses a cluster randomised trial conducted in Hanoi, Vietnam, comparing cloth masks with medical masks among hospital healthcare workers (HCWs).
Introduction
The use of face masks to protect healthcare workers (HCWs) from respiratory infections has been a long-standing practice. While medical masks are standard in high-resource settings, cloth masks remain prevalent globally, especially in areas facing emerging infectious diseases or personal protective equipment (PPE) shortages. Despite their widespread use, few studies have rigorously evaluated the efficacy of cloth masks compared with medical masks in preventing respiratory infections among HCWs. This cluster randomised trial aims to address this gap.
Study Design and Methodology
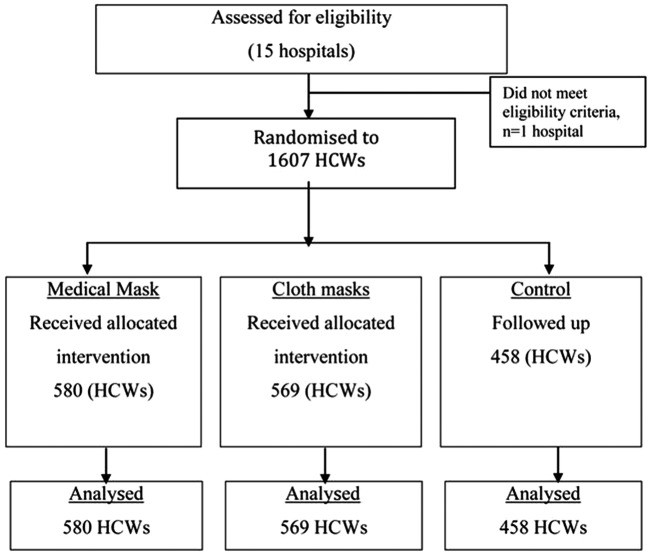
A cluster randomised trial was conducted in 14 hospitals in Hanoi, Vietnam, involving 1607 HCWs working in high-risk wards (emergency, infectious/respiratory disease, intensive care, and paediatrics). Wards were randomly assigned to one of three groups: medical masks, cloth masks, or a control group (usual practice, which often included mask use). Participants wore their assigned mask type for four consecutive weeks.
The primary outcomes measured were:
- Clinical Respiratory Illness (CRI): Defined as two or more respiratory symptoms or one respiratory symptom plus a systemic symptom.
- Influenza-Like Illness (ILI): Defined as fever ≥38°C plus one respiratory symptom.
- Laboratory-Confirmed Viral Respiratory Infection: Confirmed by nucleic acid detection using multiplex reverse transcriptase PCR (RT-PCR).
Compliance with mask use (wearing the mask for ≥70% of the work shift) was also monitored. Filtration efficiency of both mask types was tested according to the respiratory standard AS/NZS1716.
Results
The results indicated a significantly higher rate of ILI in the cloth mask group compared to the medical mask group (Relative Risk (RR)=13.25, 95% Confidence Interval (CI) 1.74 to 100.97). The cloth mask group also experienced a higher rate of ILI compared to the control group (RR=3.49, 95% CI 1.00 to 12.17).
A post-hoc analysis comparing all participants who used only medical masks with those who used only cloth masks, regardless of their assigned group, revealed that ILI (RR=6.64, 95% CI 1.45 to 28.65) and laboratory-confirmed virus infections (RR=1.72, 95% CI 1.01 to 2.94) remained significantly higher in the cloth mask group.
Filtration testing demonstrated that cloth masks allowed 97% of particles to penetrate, compared to 44% for medical masks.
Discussion
This study provides compelling evidence against the use of cloth masks for HCWs in high-risk settings. The significantly higher infection rates observed in the cloth mask group suggest that these masks may not offer adequate protection against respiratory viruses. Possible explanations include poor filtration, moisture retention, and potential self-contamination through reuse. While the study could not definitively conclude whether medical masks were protective or cloth masks were detrimental, the magnitude of the difference raises concerns about the safety of cloth masks for HCWs.
Conclusion
This cluster randomised trial demonstrates that cloth masks are associated with a significantly higher risk of respiratory illness compared to medical masks in healthcare workers. These findings have important implications for infection control guidelines and occupational health and safety practices. In high-risk healthcare settings, cloth masks should not be recommended for HCWs. Further research is needed to explore the development of more effective cloth mask designs for use in resource-limited settings.