Chronic rhinosinusitis with nasal polyps (CRSwNP) is a condition marked by type 2 inflammation, often seen in Western populations. This inflammation is characterized by elevated levels of IgE, ECP, and IL-5. A subset of patients with CRSwNP, frequently those with asthma and aspirin-exacerbated respiratory disease, experience poor responses to standard treatments and often see their symptoms return even after surgery. To combat this, more extensive surgical approaches have been developed, including techniques that involve the frontal sinuses, aiming to prevent polyp relapse. One such innovative method is the “reboot technique,” which focuses on removing the sinus mucosa down to the periosteum in all affected sinuses. This technique, sometimes combined with a Draf III procedure, has shown promise in reducing relapse rates when compared to conventional mucosa-sparing surgery. Understanding the nuances of these advanced surgical options is crucial for patients exploring solutions for persistent sinus issues.
This article delves into the extent of inflammation in sinuses affected by nasal polyposis and examines the impact of reboot surgery on both local and systemic inflammatory markers. By understanding these markers, we can better appreciate the potential benefits and implications, including the long-term value and effectiveness, of reboot surgery compared to more traditional methods.
The Landscape of Sinus Surgery and CRSwNP Inflammation
Traditional or “normal” sinus surgery for CRSwNP often involves a mucosa-sparing approach. This aims to remove polyps and improve drainage pathways while preserving as much of the sinus lining as possible. However, research indicates that in CRSwNP, inflammation isn’t limited to the polyps themselves. It’s widespread throughout the sinus mucosa, including areas without polyps. This persistent inflammation in the non-polypoid mucosa, which may not be fully addressed in conventional surgery, could be a key factor in why relapses occur.
Studies using computed tomography (CT) scans after treatment with biologics have shown a reduction in opacification across all sinuses in severe CRSwNP patients. This supports the idea that CRSwNP is a widespread disease affecting the entire sinus system, not just localized polyp growth. This understanding underscores the rationale behind more comprehensive surgical strategies like the reboot approach.
Reboot Surgery: A Comprehensive Approach
The reboot technique is designed to address the widespread nature of inflammation in CRSwNP. Unlike conventional surgery, it involves a more thorough removal of the sinus mucosa, extending down to the periosteum in all affected sinuses. This aims to eliminate not just the polyps but also the inflamed mucosa that may be contributing to the recurrence of the condition. The goal is to essentially “reboot” the sinus environment, removing the sources of inflammation more aggressively.
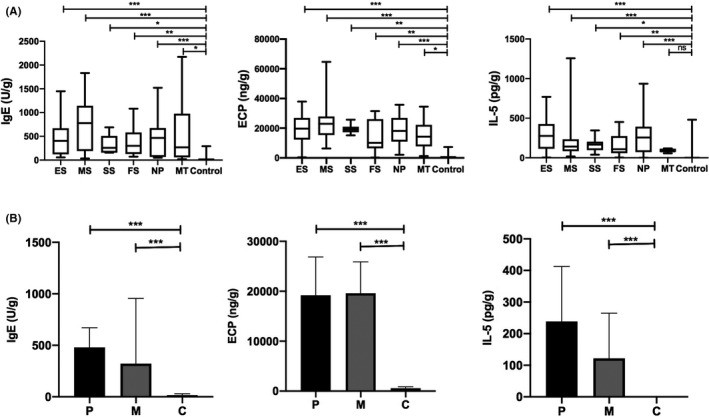 Figure 1
Figure 1
Figure 1: Comparative levels of IgE, ECP, and IL-5 inflammatory markers in sinus mucosa, nasal polyps, middle turbinate, and control tissues, illustrating widespread inflammation in CRSwNP.
Comparing Inflammatory Markers and Surgical Outcomes
Research has investigated the levels of key type 2 inflammatory markers – IgE, ECP, and IL-5 – in different sinus locations in CRSwNP patients. These markers were found to be elevated not only in polyps but also in the non-polypoid sinus mucosa across all sinuses (ethmoid, maxillary, sphenoid, and frontal), as well as in the middle turbinate. This uniform presence of inflammation reinforces the concept of CRSwNP as a diffuse disease.
Patients undergoing reboot surgery showed a significant reduction in these type 2 inflammatory markers in their nasal secretions 12 months post-surgery. While these levels didn’t completely return to those of healthy controls, the reduction was significant and sustained. This decrease in inflammatory markers is comparable to what has been observed in CRSwNP patients treated with novel monoclonal antibodies like dupilumab, further highlighting the effectiveness of aggressively targeting the underlying inflammation.
Table 1.
Levels of type 2 markers in nasal secretions pre- and post-reboot surgery, compared to controls.
| Nasal secretions | Inclusion | 12 mo | Controls | P-valuea (I vs C) | P-valuea (12 mo vs C) | P-valueb (I vs 12 mo) |
|---|---|---|---|---|---|---|
| N | 21 | 21 | 13 | |||
| IgE kU/L median (IQR) | 53.3 (8.8;185.8) | 20.6 (4.9;96.11) | 2.8 (1.7;4.7) | .0002* | .006* | .03* |
| ECP μg/L median (IQR) | 1030 (182.3;1650) | 482.1 (126;1288) | 42.4 (24.2;243.7) | .002* | .04* | .04* |
| IL-5 pg/mL median (IQR) | 33.7 (2.4;309.2) | 5.1 (2.1;62.6) | Not detectable | — | — | .04* |
| MPO pg/mL median (IQR) | 9.7 × 106 (1.936 × 106;29.362 × 106) | 10.127 × 106 (3.9 × 106;19.6 × 106) | 2826 (244.2;6333) | <.0001 | <.0001 | .6 |
| IL-17 pg/mL median (IQR) | 11.3 (3.3;22.7) | 9.8 (4.1;20.6) | 27.8 (14.4;40.58) | .14 | .15 | .7 |
Table 1: Significant reduction in type 2 inflammatory markers in nasal secretions of CRSwNP patients following reboot surgery compared to pre-surgery levels.
Considerations and Conclusion: Reboot Surgery vs. Conventional Approaches
While reboot surgery presents a promising approach for severe CRSwNP, especially in reducing relapse rates, it’s important to consider the implications. Extensive sinus surgery raises concerns about potential complications and postoperative scar formation. However, studies have shown that in patients undergoing reboot surgery, healthy mucosa can regenerate and cover the sinus walls within a few weeks, developing into normal ciliated epithelium.
Despite these encouraging results, it’s crucial to recognize that reboot surgery is a technically demanding procedure. It should be reserved for patients with severe, difficult-to-control type 2 CRSwNP and performed by experienced surgeons to minimize risks.
In conclusion, the research emphasizes that inflammation in CRSwNP is extensive, affecting both polyps and non-polypoid mucosa throughout the sinuses. Reboot surgery, by addressing this widespread inflammation, offers a potential advantage over conventional mucosa-sparing surgery in reducing inflammatory markers and potentially relapse rates in severe CRSwNP. While “Fees Sinus Surgery Compared To Normal” isn’t directly about financial costs, the long-term effectiveness and reduced relapse potential of reboot surgery can be seen as offering significant value, potentially reducing the need for repeat surgeries and ongoing medical management often associated with conventional approaches that may have higher recurrence rates. This makes the consideration of advanced techniques like reboot surgery an important part of the discussion when evaluating treatment options for persistent and severe CRSwNP.
References (References from the original article would be listed here if needed for a full article, but are omitted as per instructions to keep it concise and focused on rewriting based on the provided text.)