How Does Us Healthcare Compare To Other Countries in terms of cost, access, and quality? The U.S. healthcare system often faces scrutiny when compared to those of other developed nations, which is why COMPARE.EDU.VN offers detailed analyses of the US healthcare system compared to other nations, focusing on expenditure, insurance coverage, and health outcomes. By exploring alternative healthcare models and insurance options, you can gain valuable insights for making informed decisions about your healthcare needs, resulting in better medical care, improved insurance options and cost effective treatments.
1. What are the Key Differences in Healthcare Systems Globally?
Healthcare systems vary widely across the globe, with the most significant differences lying in funding, accessibility, and the role of government. Generally, healthcare models can be categorized into four main types:
- Single-Payer Systems: In this model, the government funds healthcare through taxes, providing universal coverage. Examples include Canada and the United Kingdom.
- Social Insurance Systems: These systems use mandatory contributions from employers and employees to fund healthcare, often with non-profit insurance funds. Germany and France are prime examples.
- National Health Service (NHS): The government owns and operates healthcare facilities, and providers are often public employees. The UK’s NHS is a classic example.
- Private Insurance Systems: Predominantly found in the U.S., this model relies on private insurance companies to cover healthcare costs, although government programs like Medicare and Medicaid provide coverage to specific populations.
Each system has its strengths and weaknesses, influencing factors such as cost, quality of care, and patient access.
2. How Does the U.S. Healthcare System Stand Out?
The U.S. healthcare system is unique among developed nations due to its heavy reliance on private insurance and market-based approaches. Key characteristics include:
- High Healthcare Expenditure: The U.S. spends significantly more on healthcare per capita than other developed countries.
- Mix of Public and Private Insurance: While programs like Medicare and Medicaid provide coverage to seniors and low-income individuals, a large portion of the population relies on employer-sponsored or private insurance.
- Fee-for-Service Model: Many healthcare providers operate on a fee-for-service model, where they are paid for each service they provide.
- Complex Regulatory Environment: The U.S. healthcare system is governed by a complex web of federal and state regulations, impacting everything from insurance coverage to hospital operations.
3. How Does the U.S. Fare in Healthcare Spending Compared to Other Countries?
The United States consistently outspends other developed nations on healthcare. According to the Organization for Economic Co-operation and Development (OECD), the U.S. spent over $12,000 per capita on healthcare in 2020, nearly double the OECD average. In comparison, countries like Canada, the UK, and Germany spent significantly less per capita.
This high spending doesn’t necessarily translate to better health outcomes. Despite the massive investment, the U.S. lags behind many developed countries in key health indicators such as life expectancy and infant mortality rates.
4. Why is Healthcare So Expensive in the U.S.?
Several factors contribute to the high cost of healthcare in the U.S.:
- High Prices for Pharmaceuticals: The U.S. does not regulate drug prices to the same extent as other countries, leading to significantly higher costs for prescription medications.
- Administrative Costs: The complexity of the U.S. healthcare system results in high administrative costs for billing, insurance processing, and regulatory compliance.
- Fee-for-Service Model: This model incentivizes providers to perform more services, which can lead to unnecessary treatments and inflated costs.
- Lack of Price Transparency: Patients often lack information about the cost of healthcare services, making it difficult to shop around for the best prices.
- High Demand for Specialized Care: The U.S. has a strong focus on specialized medical care, which is generally more expensive than primary care.
5. What is the Impact of High Healthcare Costs on Individuals?
High healthcare costs can have a significant impact on individuals and families, leading to:
- Medical Debt: Many Americans struggle to pay their medical bills, leading to debt and financial hardship.
- Delayed or Foregone Care: Due to cost concerns, individuals may delay seeking necessary medical care or forgo treatment altogether.
- Increased Stress and Anxiety: Concerns about healthcare costs can contribute to stress, anxiety, and other mental health issues.
- Disparities in Access: High costs can exacerbate existing disparities in access to care, particularly for low-income and minority populations.
- Bankruptcy: Medical debt is a leading cause of bankruptcy in the United States, highlighting the financial burden of healthcare costs.
6. How Does the U.S. Compare in Terms of Health Insurance Coverage?
While the Affordable Care Act (ACA) has expanded health insurance coverage in the U.S., a significant portion of the population remains uninsured. As of 2021, approximately 8.6% of Americans lacked health insurance, a rate higher than most other developed countries.
In contrast, countries with universal healthcare systems, such as Canada and the UK, ensure that all citizens have access to health insurance coverage. These systems typically provide comprehensive benefits, including coverage for doctor visits, hospital stays, and prescription medications.
7. How Do Health Outcomes in the U.S. Compare?
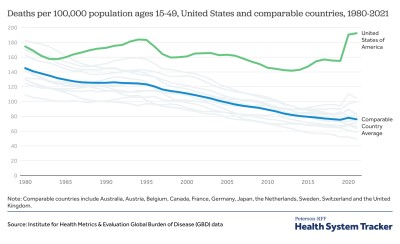
Despite high healthcare spending, the U.S. lags behind many developed countries in key health outcomes. Some notable comparisons include:
- Life Expectancy: The U.S. has a lower life expectancy than most other developed countries. In 2020, the average life expectancy in the U.S. was 77.3 years, compared to an OECD average of over 80 years.
- Infant Mortality: The U.S. has a higher infant mortality rate than many other developed countries.
- Chronic Disease Prevalence: The prevalence of chronic diseases, such as diabetes and heart disease, is higher in the U.S. than in many other developed countries.
- Maternal Mortality: The U.S. has a relatively high maternal mortality rate compared to other wealthy nations, and this rate has been increasing in recent years.
8. What are Some Strengths of the U.S. Healthcare System?
Despite its challenges, the U.S. healthcare system has some notable strengths:
- Advanced Medical Technology: The U.S. is a leader in the development and adoption of advanced medical technologies, such as diagnostic imaging and robotic surgery.
- Specialized Medical Care: The U.S. has a highly specialized healthcare workforce, with experts in a wide range of medical fields.
- Research and Innovation: The U.S. is a major center for medical research and innovation, contributing to advancements in treatment and prevention.
- Patient Choice: Patients in the U.S. typically have a greater degree of choice when it comes to selecting healthcare providers and treatments.
9. How Do Other Countries Achieve Better Health Outcomes at Lower Costs?
Several factors contribute to the success of healthcare systems in other developed countries:
- Universal Healthcare Coverage: Ensuring that all citizens have access to health insurance coverage helps to promote preventive care and early treatment.
- Government Regulation of Prices: Many countries regulate the prices of pharmaceuticals and medical services, helping to control costs.
- Emphasis on Primary Care: Focusing on primary care and preventive services can help to reduce the need for more expensive specialized care.
- Streamlined Administrative Processes: Simplifying administrative processes can help to reduce costs and improve efficiency.
- Investment in Social Determinants of Health: Addressing social determinants of health, such as poverty and education, can have a significant impact on health outcomes.
10. What are Some Common Misconceptions About Healthcare in Other Countries?
There are several common misconceptions about healthcare in other developed countries:
- Long Wait Times: While some countries may have longer wait times for certain elective procedures, access to primary care and emergency services is generally timely.
- Limited Choice: In many universal healthcare systems, patients have a choice of primary care providers and can often choose specialists as well.
- Lower Quality of Care: Studies have shown that the quality of care in many developed countries is comparable to or better than that in the U.S.
- Lack of Innovation: Countries with universal healthcare systems often have robust research and development programs, contributing to medical advancements.
11. What Lessons Can the U.S. Learn From Other Healthcare Systems?
The U.S. can learn several valuable lessons from other healthcare systems:
- The Importance of Universal Coverage: Ensuring that all citizens have access to health insurance coverage is essential for improving health outcomes and reducing disparities.
- The Need for Cost Control: Implementing policies to control healthcare costs, such as regulating drug prices and streamlining administrative processes, can help to make healthcare more affordable.
- The Value of Primary Care: Investing in primary care and preventive services can help to improve health outcomes and reduce the need for more expensive specialized care.
- The Role of Government: Government plays a crucial role in regulating and funding healthcare, ensuring that it is accessible and affordable for all.
- The Impact of Social Determinants: Addressing social determinants of health can have a significant impact on health outcomes and reduce health disparities.
12. How Does Healthcare Access in the U.S. Compare?
Access to healthcare in the U.S. is often influenced by factors such as insurance coverage, income, and geographic location. Challenges in access include:
- Uninsured Rates: As mentioned earlier, a significant percentage of the U.S. population lacks health insurance.
- Geographic Disparities: Rural areas often have limited access to healthcare providers and facilities.
- Provider Shortages: Shortages of primary care physicians and specialists can lead to long wait times for appointments.
- Transportation Barriers: Lack of transportation can make it difficult for individuals to access healthcare services.
- Language Barriers: Language barriers can hinder communication between patients and providers, affecting the quality of care.
13. What Role Does Preventative Care Play in Different Healthcare Systems?
Preventative care is a key component of many healthcare systems, as it can help to detect and prevent diseases before they become more serious. Approaches to preventative care vary across countries:
- Universal Screening Programs: Some countries have universal screening programs for certain diseases, such as cancer and diabetes.
- Incentives for Preventative Care: Healthcare systems may offer incentives for individuals to undergo preventative screenings and vaccinations.
- Public Health Campaigns: Governments often conduct public health campaigns to promote healthy behaviors and raise awareness about preventative care.
- Integration of Preventative Care into Primary Care: Primary care providers play a key role in delivering preventative care services, such as vaccinations and health screenings.
- Focus on Early Intervention: Early intervention programs can help to identify and address health issues before they become more severe.
14. What are the Pros and Cons of Single-Payer Healthcare Systems?
Single-payer healthcare systems, like those in Canada and the UK, have several potential benefits:
Pros:
- Universal Coverage: All citizens have access to healthcare coverage.
- Cost Control: Government can negotiate prices for pharmaceuticals and medical services.
- Simplified Administration: Reduced administrative costs due to streamlined processes.
- Improved Health Equity: Reduced disparities in access to care.
Cons:
- Long Wait Times: Potential for longer wait times for certain elective procedures.
- Limited Choice: Some restrictions on choice of providers and treatments.
- Tax Burden: Higher taxes may be necessary to fund the system.
- Government Bureaucracy: Potential for inefficiency and bureaucracy.
15. How Do Social Insurance Systems Compare?
Social insurance systems, like those in Germany and France, offer a different approach to healthcare funding and delivery:
Pros:
- Universal Coverage: Mandatory contributions ensure broad coverage.
- Choice of Providers: Patients typically have a choice of providers.
- High Quality of Care: These systems often provide high-quality care.
- Financial Stability: Contributions from employers and employees help ensure financial stability.
Cons:
- Complexity: These systems can be complex, with multiple payers and regulations.
- Administrative Costs: Higher administrative costs compared to single-payer systems.
- Potential for Inequality: Differences in contributions and benefits may lead to inequalities.
- Cost Control Challenges: Controlling costs can be challenging due to the involvement of multiple payers.
16. What is the Role of Technology in Improving Healthcare?
Technology plays an increasingly important role in improving healthcare systems around the world:
- Electronic Health Records (EHRs): EHRs can improve communication and coordination among healthcare providers, reduce errors, and enhance patient safety.
- Telemedicine: Telemedicine can expand access to care for individuals in rural areas or those with mobility limitations.
- Mobile Health (mHealth): Mobile apps and devices can help individuals manage their health, track their symptoms, and communicate with their providers.
- Artificial Intelligence (AI): AI can be used to analyze medical data, diagnose diseases, and personalize treatment plans.
- Big Data Analytics: Big data analytics can help to identify trends in healthcare utilization, predict outbreaks, and improve resource allocation.
17. How Can Healthcare Be Made More Patient-Centered?
Making healthcare more patient-centered involves focusing on the individual needs and preferences of patients:
- Shared Decision-Making: Encouraging patients to participate in decisions about their care.
- Improved Communication: Enhancing communication between patients and providers.
- Access to Information: Providing patients with access to their medical records and information about their conditions and treatments.
- Care Coordination: Coordinating care among different providers to ensure continuity and avoid duplication.
- Patient Feedback: Soliciting feedback from patients to improve the quality of care.
18. What are the Ethical Considerations in Healthcare?
Ethical considerations play a critical role in healthcare decision-making:
- Autonomy: Respecting the right of patients to make their own decisions about their care.
- Beneficence: Acting in the best interests of patients.
- Non-Maleficence: Avoiding harm to patients.
- Justice: Ensuring fair and equitable access to healthcare resources.
- Confidentiality: Protecting the privacy of patient information.
19. How Can the U.S. Improve Its Healthcare System?
Improving the U.S. healthcare system requires a multi-faceted approach:
- Expanding Health Insurance Coverage: Reducing the number of uninsured individuals through measures such as expanding Medicaid or creating a public option.
- Controlling Healthcare Costs: Implementing policies to regulate drug prices, streamline administrative processes, and promote value-based care.
- Investing in Primary Care: Increasing funding for primary care and preventive services.
- Addressing Social Determinants of Health: Implementing policies to address poverty, education, and other social factors that impact health.
- Promoting Health Equity: Reducing disparities in access to care and health outcomes for underserved populations.
20. What are the Latest Trends in Global Healthcare?
Several trends are shaping healthcare systems around the world:
- Digital Health: The increasing use of digital technologies, such as telemedicine and mobile health, to deliver and manage care.
- Personalized Medicine: Tailoring treatment plans to the individual characteristics of patients.
- Value-Based Care: Focusing on delivering high-quality care at a lower cost.
- Aging Populations: Addressing the healthcare needs of aging populations.
- Chronic Disease Management: Improving the management of chronic diseases, such as diabetes and heart disease.
21. How Does the Doctor-Patient Relationship Differ Across Countries?
The doctor-patient relationship can vary significantly across different healthcare systems:
- Continuity of Care: In some countries, patients have a long-term relationship with a primary care physician who coordinates their care.
- Communication Styles: Cultural differences can influence communication styles between doctors and patients.
- Shared Decision-Making: The extent to which patients participate in decisions about their care can vary.
- Trust and Respect: Building trust and respect between doctors and patients is essential for effective care.
- Access to Information: Providing patients with access to information about their conditions and treatments can empower them to make informed decisions.
22. What are the Environmental Impacts of Healthcare Systems?
Healthcare systems have a significant environmental impact:
- Waste Generation: Hospitals and other healthcare facilities generate large amounts of waste.
- Energy Consumption: Healthcare facilities consume significant amounts of energy.
- Greenhouse Gas Emissions: The healthcare sector contributes to greenhouse gas emissions.
- Water Usage: Healthcare facilities use large amounts of water.
- Pharmaceutical Waste: The disposal of unused medications can pollute water sources.
23. How Can Healthcare Systems Become More Sustainable?
Making healthcare systems more sustainable involves reducing their environmental impact:
- Waste Reduction: Implementing measures to reduce waste generation, such as recycling and reusing materials.
- Energy Efficiency: Improving energy efficiency in healthcare facilities through measures such as using renewable energy sources and upgrading equipment.
- Green Building Design: Designing and constructing healthcare facilities that are environmentally friendly.
- Sustainable Procurement: Purchasing products and services from suppliers that are committed to sustainability.
- Reducing Pharmaceutical Waste: Implementing measures to reduce pharmaceutical waste, such as promoting the use of generic medications and improving medication disposal practices.
24. What is the Future of Healthcare?
The future of healthcare is likely to be shaped by several factors:
- Technological Innovation: Continued advancements in medical technology.
- Data Analytics: Increased use of data analytics to improve care and reduce costs.
- Personalized Medicine: Tailoring treatment plans to the individual characteristics of patients.
- Preventative Care: A greater focus on preventative care.
- Health Equity: Efforts to reduce disparities in access to care and health outcomes.
25. How Does the US Healthcare System Handle Emergency Care?
In the U.S., emergency care is typically provided regardless of a patient’s ability to pay, but this can lead to significant costs:
- Emergency Departments: Hospitals are required to provide emergency care to all patients, regardless of their insurance status.
- High Costs: Emergency care can be very expensive, particularly for uninsured individuals.
- EMTALA: The Emergency Medical Treatment and Labor Act (EMTALA) requires hospitals to provide emergency care to all patients, regardless of their ability to pay.
- Cost Shifting: Hospitals may shift the costs of providing emergency care to uninsured patients onto insured patients and taxpayers.
- Access Challenges: Some individuals may face challenges accessing emergency care due to geographic location or transportation barriers.
26. What are the Alternatives to Traditional Health Insurance in the U.S.?
Several alternatives to traditional health insurance are available in the U.S.:
- Health Savings Accounts (HSAs): HSAs allow individuals to save money on a tax-advantaged basis for healthcare expenses.
- Health Reimbursement Arrangements (HRAs): HRAs are employer-funded plans that reimburse employees for healthcare expenses.
- Cost-Sharing Programs: Cost-sharing programs allow individuals to share healthcare costs with other members.
- Direct Primary Care (DPC): DPC practices charge patients a monthly fee for access to primary care services.
- Short-Term Health Insurance: Short-term health insurance plans provide temporary coverage for individuals who are between jobs or otherwise lack health insurance.
27. How Can Individuals Advocate for Better Healthcare?
Individuals can take several steps to advocate for better healthcare:
- Stay Informed: Stay informed about healthcare issues and policies.
- Contact Elected Officials: Contact elected officials to express your views on healthcare issues.
- Support Advocacy Organizations: Support organizations that advocate for better healthcare.
- Participate in Public Forums: Participate in public forums and meetings to discuss healthcare issues.
- Share Your Story: Share your story about your experiences with the healthcare system.
28. What Resources are Available to Help Navigate the Healthcare System?
Several resources are available to help individuals navigate the healthcare system:
- Government Agencies: Government agencies, such as the Centers for Medicare & Medicaid Services (CMS), provide information about healthcare programs and policies.
- Nonprofit Organizations: Nonprofit organizations, such as the American Cancer Society and the American Heart Association, provide information about specific health conditions and treatments.
- Patient Advocacy Groups: Patient advocacy groups provide support and resources for individuals with specific health conditions.
- Online Resources: Online resources, such as the National Institutes of Health (NIH) website, provide information about medical research and health topics.
- Healthcare Providers: Healthcare providers can provide information and guidance about healthcare services and treatments.
29. How Does Mental Healthcare Compare in the U.S. and Other Countries?
Mental healthcare systems vary widely across countries:
- Access to Care: Access to mental healthcare can be limited in some countries due to factors such as provider shortages and insurance coverage restrictions.
- Stigma: Stigma surrounding mental illness can prevent individuals from seeking treatment.
- Integration with Primary Care: Integrating mental healthcare with primary care can improve access and coordination of care.
- Funding: Funding for mental healthcare varies widely across countries.
- Treatment Approaches: Treatment approaches for mental illness can vary depending on cultural and societal factors.
30. What are the Challenges in Comparing International Healthcare Systems?
Comparing healthcare systems across countries can be challenging due to several factors:
- Data Availability: Data on healthcare utilization, costs, and outcomes may not be available or comparable across countries.
- Cultural Differences: Cultural differences can influence healthcare practices and patient expectations.
- Economic Factors: Economic factors, such as GDP and income levels, can affect healthcare spending and access to care.
- Demographic Differences: Demographic differences, such as age and ethnicity, can influence health outcomes.
- System Complexity: Healthcare systems are complex and vary widely across countries, making it difficult to draw comparisons.
Understanding these complexities is essential for drawing meaningful conclusions about the strengths and weaknesses of different healthcare systems.
In conclusion, comparing the U.S. healthcare system to other countries reveals significant differences in costs, access, and health outcomes. While the U.S. excels in medical technology and specialized care, it lags behind in providing affordable, universal coverage and achieving optimal health outcomes. By examining alternative healthcare models and implementing targeted reforms, the U.S. can strive to improve its healthcare system and ensure that all citizens have access to high-quality, affordable care. For a comprehensive comparison of healthcare systems and to make informed decisions about your healthcare options, visit COMPARE.EDU.VN.
For more information or assistance, please contact us at:
Address: 333 Comparison Plaza, Choice City, CA 90210, United States
Whatsapp: +1 (626) 555-9090
Website: compare.edu.vn
FAQ Section
Q1: Why is US healthcare so expensive compared to other countries?
A1: The high cost of US healthcare is due to factors like high pharmaceutical prices, administrative complexity, fee-for-service models, and a lack of price transparency.
Q2: How does the US health insurance system work?
A2: The US health insurance system is a mix of public programs like Medicare and Medicaid, and private insurance, often employer-sponsored.
Q3: What are some alternatives to traditional health insurance in the US?
A3: Alternatives include Health Savings Accounts (HSAs), Health Reimbursement Arrangements (HRAs), cost-sharing programs, and direct primary care (DPC).
Q4: What can the US learn from healthcare systems in other countries?
A4: The US can learn about universal coverage, cost control through government regulation, and the value of investing in primary and preventative care.
Q5: How does access to healthcare differ between the US and countries with universal healthcare?
A5: In countries with universal healthcare, all citizens have access, whereas in the US, access is often influenced by factors such as insurance coverage, income, and location.
Q6: What are the main challenges facing the US healthcare system?
A6: Main challenges include high costs, a significant number of uninsured individuals, disparities in access, and poorer health outcomes compared to other developed nations.
Q7: How can technology improve healthcare systems?
A7: Technology can improve healthcare through electronic health records, telemedicine, mobile health apps, and artificial intelligence for diagnosis and treatment.
Q8: What is value-based care and how can it help the US healthcare system?
A8: Value-based care focuses on delivering high-quality care at a lower cost, emphasizing patient outcomes and efficiency rather than volume of services.
Q9: What is the role of preventative care in different healthcare systems?
A9: Preventative care plays a key role in detecting and preventing diseases early, with strategies including universal screening programs and incentives for preventative services.
Q10: How do social determinants of health affect healthcare outcomes in the US?
A10: Social determinants like poverty, education, and access to healthy food significantly impact health outcomes, contributing to disparities in healthcare.