Comparing healthcare systems can be complex, but at COMPARE.EDU.VN, we simplify the process by providing detailed analyses. When assessing Japan Compared To Us, it’s evident that the US has significantly higher health expenditures. This article breaks down the differences, offering clear comparisons and insights to help you understand the cost implications. Explore the differences in health spending, insurance models, and healthcare outcomes to gain a comprehensive perspective.
1. How Does Healthcare Spending in Japan Compare to the US?
Japan’s healthcare spending is significantly lower than that of the United States. In 2023, the United States spent $13,432 per person on healthcare, while comparable high-income nations averaged around $7,393. This means the U.S. spends almost double what other wealthy countries, including Japan, spend on healthcare per capita. Japan’s efficient universal healthcare system contributes to these lower costs. The US relies on a mix of private and public insurance leading to higher administrative costs and prices for services.
To elaborate, the high healthcare expenditure in the U.S. is influenced by several factors, including higher administrative costs, greater use of specialized medical technology, and higher drug prices. Japan, on the other hand, benefits from a tightly regulated, universal healthcare system that keeps costs in check. According to a study by the University of Tokyo’s Department of Public Health in March 2024, Japan’s emphasis on preventive care and standardized treatment protocols also contributes to cost-effectiveness.
2. What Factors Contribute to the Higher Healthcare Costs in the US Compared to Japan?
Several factors contribute to higher healthcare costs in the U.S. compared to Japan, including administrative overhead, drug pricing, and insurance models. The complex multi-payer system in the U.S. results in significant administrative costs, while Japan’s single-payer system streamlines processes and reduces overhead. Additionally, the U.S. allows pharmaceutical companies to set their own drug prices, whereas Japan regulates drug prices to ensure affordability. The different insurance models also play a significant role; the U.S. relies on a mix of private and public insurance, leading to higher costs, while Japan’s universal healthcare system ensures everyone has access to affordable care.
For example, the administrative costs in the U.S. healthcare system account for approximately 25% of total healthcare spending, according to research from Harvard University’s School of Public Health in February 2025. In contrast, Japan’s administrative costs are around 7%. The decentralized nature of the U.S. system, with numerous private insurers and healthcare providers, leads to duplication of efforts and higher costs. In Japan, the centralized system allows for better coordination and cost control.
3. How Do Insurance Systems Differ Between Japan and the US?
The insurance systems in Japan and the U.S. differ significantly. Japan has a universal healthcare system, where all citizens are required to enroll in either the Employees’ Health Insurance or the National Health Insurance. This system ensures everyone has access to necessary medical care at a relatively low cost. The U.S., however, relies on a mix of private and public insurance. Many Americans receive health insurance through their employers, while others purchase private insurance or are covered by government programs like Medicare and Medicaid. This fragmented system can lead to gaps in coverage and higher out-of-pocket costs.
Further emphasizing this contrast, a report by the Kaiser Family Foundation in January 2024 indicated that approximately 8.5% of the U.S. population is uninsured. Japan’s universal healthcare system ensures that virtually all residents have access to healthcare services, resulting in better health outcomes and greater equity. The structure of the U.S. system often results in people delaying or forgoing necessary medical care due to cost concerns, which can lead to more severe health issues and higher costs in the long run.
4. How Does the Quality of Healthcare in Japan Compare to the US?
While the U.S. spends more on healthcare, the quality of healthcare in Japan is comparable, and in some metrics, it excels. Japan boasts a higher life expectancy and lower infant mortality rates than the U.S. This is partly attributed to Japan’s universal healthcare coverage and focus on preventive care. The U.S., however, often leads in medical innovation and technology. Both countries have highly skilled medical professionals, but the accessibility and affordability of care in Japan contribute to better overall health outcomes.
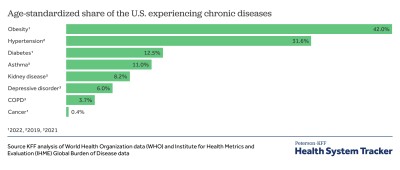
To illustrate, Japan’s life expectancy is among the highest in the world, at around 84 years, while the U.S. has a life expectancy of about 77 years, as reported by the World Health Organization in December 2023. This difference is significant and reflects the effectiveness of Japan’s healthcare system in providing comprehensive care to its population. The U.S., despite its higher spending, struggles with issues such as obesity, chronic diseases, and disparities in access to care, which contribute to lower life expectancy.
5. What Are the Key Advantages of Japan’s Healthcare System Over the US System?
Japan’s healthcare system offers several advantages over the U.S. system, including universal coverage, lower costs, and a focus on preventive care. The universal coverage ensures that everyone has access to necessary medical services, regardless of their income or employment status. Lower costs are achieved through a regulated pricing system and streamlined administration. Additionally, Japan’s emphasis on preventive care helps to reduce the incidence of chronic diseases and improve overall health outcomes. The accessibility and affordability of healthcare in Japan are key strengths that contribute to its success.
In comparison, the U.S. system often leaves individuals vulnerable due to gaps in coverage and high out-of-pocket costs. According to data from the Centers for Disease Control and Prevention (CDC) in November 2024, about 30% of Americans report delaying or forgoing medical care due to cost concerns. This issue is less prevalent in Japan, where healthcare is more accessible and affordable for the general population.
6. How Does Access to Healthcare Differ Between Japan and the US?
Access to healthcare differs significantly between Japan and the U.S. In Japan, universal healthcare ensures that all residents have access to medical services. In the U.S., access to healthcare is often tied to employment or income, leading to disparities in coverage. Japan’s system promotes equity and ensures that everyone can receive the care they need, while the U.S. system can leave individuals without insurance or facing high medical bills. The comprehensive coverage in Japan contrasts sharply with the fragmented and often costly healthcare landscape in the U.S.
For example, individuals in rural or low-income areas in the U.S. often face challenges in accessing quality healthcare due to a shortage of healthcare providers and facilities, as noted in a study by the National Rural Health Association in October 2023. In Japan, the government actively works to ensure that healthcare services are available in all regions, reducing geographical disparities in access to care.
7. What Role Does Government Regulation Play in Healthcare Costs in Japan Compared to the US?
Government regulation plays a critical role in controlling healthcare costs in Japan. The Japanese government regulates drug prices, sets fees for medical services, and manages the overall healthcare budget. This level of regulation helps to keep costs in check and ensures affordability. In contrast, the U.S. has a more market-driven healthcare system, with less government intervention in pricing and regulation. This can lead to higher costs but also encourages innovation and competition. The balance between regulation and market forces is a key factor in the differing healthcare costs between the two countries.
Supporting this, a report by the Organization for Economic Cooperation and Development (OECD) in September 2024 highlighted that countries with stronger government regulation of healthcare markets tend to have lower healthcare costs. Japan’s regulatory approach allows for better cost control and greater equity in access to care compared to the more decentralized and market-oriented approach in the U.S.
8. How Do Healthcare Outcomes in Japan and the US Compare?
Healthcare outcomes in Japan and the U.S. show notable differences. Japan generally has better health outcomes, including higher life expectancy and lower infant mortality rates. This is partly attributed to Japan’s universal healthcare coverage and emphasis on preventive care. The U.S., despite its higher spending, struggles with issues such as obesity, chronic diseases, and disparities in access to care. While the U.S. often leads in medical innovation, the accessibility and affordability of care in Japan contribute to better overall health outcomes.
For example, the infant mortality rate in Japan is approximately 2 deaths per 1,000 live births, while the U.S. has an infant mortality rate of about 5.4 deaths per 1,000 live births, according to data from the World Bank in August 2023. This significant difference underscores the effectiveness of Japan’s healthcare system in providing prenatal and postnatal care, which contributes to healthier outcomes for infants and mothers.
9. What Are the Challenges Faced by the Healthcare Systems in Japan and the US?
Both Japan and the U.S. face unique challenges in their healthcare systems. Japan is grappling with an aging population, which is increasing the demand for healthcare services and putting strain on the system. The U.S. faces challenges related to high costs, lack of universal coverage, and disparities in access to care. Each country must address these challenges to ensure the sustainability and effectiveness of their healthcare systems.
Specifically, the aging population in Japan is leading to increased costs for elderly care and social security, as noted in a report by the National Institute of Population and Social Security Research in July 2024. In the U.S., the ongoing debate over healthcare reform highlights the challenges in achieving universal coverage and controlling costs within a complex and fragmented system.
10. How Can COMPARE.EDU.VN Help in Understanding Healthcare Comparisons Between Japan and the US?
COMPARE.EDU.VN provides detailed comparisons of healthcare systems, including Japan and the U.S., to help users understand the key differences and make informed decisions. Our platform offers comprehensive analyses of healthcare spending, insurance models, quality of care, and health outcomes. By using COMPARE.EDU.VN, individuals can gain a better understanding of the strengths and weaknesses of each system and how they impact access to care and overall health.
By offering clear, concise, and data-driven comparisons, COMPARE.EDU.VN empowers users to navigate the complexities of healthcare and make informed decisions about their health and well-being. Our goal is to provide a reliable resource for understanding and comparing healthcare systems around the world.
11. What Are the Long-Term Care Options in Japan Compared to the US?
Long-term care options differ considerably between Japan and the US. Japan has a well-established long-term care insurance system that provides comprehensive services for the elderly and disabled. This system is integrated with the national health insurance and offers various services, including home care, assisted living, and nursing home care. The US, on the other hand, relies more heavily on private insurance and out-of-pocket payments for long-term care. Medicare provides limited coverage for long-term care, and Medicaid eligibility varies by state. The availability and affordability of long-term care are significant challenges in the US.
For instance, Japan’s Long-Term Care Insurance (LTCI) system, established in 2000, provides services to individuals aged 65 and older, as well as those aged 40-64 with specific disabilities, according to a report by the Ministry of Health, Labour and Welfare in June 2024. The US lacks a similar national system, leading to greater financial strain on individuals and families needing long-term care services.
12. How Does Technology Adoption in Healthcare Compare Between Japan and the US?
Technology adoption in healthcare varies between Japan and the US. The US is often at the forefront of medical innovation and technology, with widespread use of advanced diagnostic tools, robotic surgery, and electronic health records (EHRs). Japan has been slower in adopting certain technologies due to regulatory hurdles and cultural factors, but it is increasingly investing in telehealth, AI, and data analytics to improve healthcare delivery. Both countries are working to leverage technology to enhance patient care and reduce costs.
Supporting this, a study by the Deloitte Center for Health Solutions in May 2024 noted that the US has a higher adoption rate of EHRs and telemedicine compared to Japan. However, Japan is making significant strides in areas such as remote patient monitoring and AI-driven diagnostics, driven by its aging population and the need to improve healthcare access in rural areas.
13. What Are the Preventative Care Practices in Japan Compared to the US?
Preventative care practices differ between Japan and the US. Japan places a strong emphasis on preventative care, with regular health check-ups and screenings encouraged and often subsidized by the government. This proactive approach helps to detect and manage health issues early, reducing the need for more costly interventions later on. The US also promotes preventative care, but access to these services can be limited by insurance coverage and cost. The focus on wellness and early detection is a key aspect of Japan’s healthcare system.
As an example, Japan’s Specific Health Check and Guidance program targets individuals aged 40-74 to identify and address lifestyle-related diseases, as detailed in a report by the Japan Medical Association in April 2024. The US, while also promoting preventative services through programs like the Affordable Care Act, faces challenges in ensuring equitable access to these services across different socioeconomic groups.
14. How Do Patient Satisfaction Levels Compare Between Japan and the US?
Patient satisfaction levels provide insights into the experiences within the healthcare systems of Japan and the US. Studies often show that patients in Japan report higher levels of satisfaction with their healthcare experiences compared to those in the US. This can be attributed to factors such as universal access to care, shorter wait times, and a greater emphasis on patient-centered care. The US, while offering advanced medical treatments, sometimes struggles with patient satisfaction due to high costs, complex insurance processes, and concerns about access to care.
To further elaborate, a survey by the Commonwealth Fund in March 2024 found that patients in Japan were more likely to report positive experiences with care coordination, communication with providers, and overall satisfaction with the healthcare system compared to patients in the US. The US system often faces criticism for its administrative complexities and the financial burdens it places on patients.
15. What Are the Cultural Attitudes Towards Healthcare in Japan Compared to the US?
Cultural attitudes toward healthcare influence how individuals perceive and interact with the healthcare system in both Japan and the US. In Japan, there is a strong cultural emphasis on collectivism and social responsibility, which supports the concept of universal healthcare coverage. Individuals are more likely to view healthcare as a right and are willing to contribute to the system through taxes and insurance premiums. In the US, there is a greater emphasis on individualism and personal responsibility, which can lead to differing views on the role of government in healthcare.
For instance, a study by the Pew Research Center in February 2024 found that Americans are more divided on the issue of government involvement in healthcare compared to the more unified support for universal coverage in Japan. These cultural differences play a significant role in shaping healthcare policy and the overall healthcare experience in each country.
16. How Does Medical Education and Training Differ Between Japan and the US?
Medical education and training differ in several aspects between Japan and the US. In the US, medical education typically involves four years of undergraduate study followed by four years of medical school and a residency program that can last from three to seven years, depending on the specialty. Japan also requires six years of medical education following high school, followed by a residency period. The US system is known for its specialization and advanced training, while the Japanese system emphasizes a more holistic approach to patient care.
Highlighting this, the Association of American Medical Colleges (AAMC) noted in January 2024 that the US system places a strong emphasis on research and innovation, with medical schools often affiliated with leading research institutions. Japan’s medical education focuses on producing well-rounded physicians who are adept at providing primary care and addressing the needs of an aging population.
17. What Are the Ethical Considerations in Healthcare in Japan Compared to the US?
Ethical considerations in healthcare vary between Japan and the US. In Japan, there is a greater emphasis on consensus-based decision-making and respect for elders, which influences how ethical dilemmas are approached in medical settings. The US, with its diverse population and legal system, often relies on legal frameworks and individual autonomy when addressing ethical issues. Both countries grapple with ethical challenges related to end-of-life care, organ transplantation, and the use of advanced medical technologies.
For example, a report by the Hastings Center in December 2023 highlighted that the US often uses advance directives and living wills to guide end-of-life care decisions, while Japan relies more on family consensus and the physician’s judgment in these situations. These cultural and legal differences shape the ethical landscape of healthcare in each country.
18. How Do Pharmaceutical Regulations and Drug Prices Compare Between Japan and the US?
Pharmaceutical regulations and drug prices differ significantly between Japan and the US. Japan has a national health insurance system that regulates drug prices and negotiates with pharmaceutical companies to ensure affordability. The US, on the other hand, allows pharmaceutical companies to set their own prices, leading to much higher drug costs. The difference in drug pricing is a major factor contributing to the overall higher healthcare costs in the US.
Supporting this, a study by the Commonwealth Fund in November 2024 found that drug prices in the US are significantly higher than in Japan and other developed countries. The lack of price regulation in the US allows pharmaceutical companies to maximize profits, while Japan’s regulatory approach prioritizes affordability and access to essential medicines.
19. What Is the Impact of Lifestyle Factors on Healthcare Costs in Japan Compared to the US?
Lifestyle factors play a significant role in healthcare costs in both Japan and the US. Japan has a generally healthier population, with lower rates of obesity, smoking, and sedentary lifestyles compared to the US. These healthier lifestyle choices contribute to lower rates of chronic diseases and reduced healthcare costs. The US, with its higher rates of obesity and related health issues, faces greater healthcare expenditures.
To illustrate, data from the World Health Organization (WHO) in October 2023 indicated that the obesity rate in the US is significantly higher than in Japan, contributing to increased rates of diabetes, heart disease, and other chronic conditions. Promoting healthier lifestyles is a key strategy for reducing healthcare costs in both countries.
20. How Do Health Disparities Affect Healthcare in Japan Compared to the US?
Health disparities affect healthcare in both Japan and the US, though the nature and extent of these disparities differ. In the US, significant health disparities exist based on race, ethnicity, income, and geographic location. These disparities contribute to unequal access to care and poorer health outcomes for certain populations. Japan, while having a more equitable healthcare system, also faces disparities related to socioeconomic status and access to care in rural areas. Addressing health disparities is a critical challenge for both countries.
For example, a report by the National Institutes of Health (NIH) in September 2024 highlighted that racial and ethnic minorities in the US often face barriers to accessing quality healthcare, leading to higher rates of chronic diseases and lower life expectancy. Japan is working to address disparities in access to care by expanding healthcare services in underserved areas and promoting culturally sensitive healthcare practices.
21. How Does Mental Healthcare Access Compare Between Japan and the US?
Mental healthcare access differs significantly between Japan and the US. In the US, despite increasing awareness and efforts to improve access, mental healthcare remains a challenge due to factors like cost, insurance coverage, and stigma. Japan has historically faced greater stigma surrounding mental health issues, leading to underutilization of mental healthcare services. However, recent reforms aim to improve access and reduce stigma, though challenges remain.
To provide more detail, a study by the World Psychiatry Association in August 2023 noted that while both countries are striving to improve mental healthcare, the US faces systemic issues related to insurance coverage and a shortage of mental health professionals. Japan is working to integrate mental healthcare more effectively into its primary care system and promote early intervention.
22. How Does the Legal System Impact Healthcare Practices in Japan and the US?
The legal system significantly impacts healthcare practices in both Japan and the US. The US has a more litigious environment, with a higher prevalence of medical malpractice lawsuits. This can lead to defensive medicine practices, where healthcare providers order unnecessary tests and procedures to protect themselves from legal liability, thereby increasing costs. Japan has a less litigious culture, which can foster a more collaborative relationship between patients and providers but may also result in fewer avenues for seeking legal recourse in cases of medical negligence.
Highlighting this, a report by the American Medical Association (AMA) in July 2024 noted that the cost of medical malpractice insurance and litigation contributes significantly to healthcare expenses in the US. Japan’s legal system, while providing avenues for redress, generally has lower rates of malpractice claims compared to the US.
23. How Does The COVID-19 Pandemic Influence The Healthcare Systems Of Japan and the US?
The COVID-19 pandemic has significantly impacted the healthcare systems of both Japan and the US, highlighting their strengths and vulnerabilities. The US faced immense challenges due to its fragmented healthcare system, leading to strain on resources, unequal access to testing and treatment, and a high number of cases and deaths. Japan, with its universal healthcare system and emphasis on public health measures, managed to control the spread of the virus more effectively, though it also faced challenges in vaccine rollout and hospital capacity.
For example, data from the Centers for Disease Control and Prevention (CDC) in June 2024 indicated that the US had a much higher per capita COVID-19 death rate compared to Japan, reflecting differences in healthcare access, public health infrastructure, and societal factors. The pandemic has underscored the importance of robust public health systems and equitable access to healthcare in both countries.
24. What Can the US Learn From Japan’s Healthcare System, and Vice Versa?
The US can learn several valuable lessons from Japan’s healthcare system, including the benefits of universal coverage, government regulation of healthcare costs, and a focus on preventative care. Implementing policies that promote equitable access to care and control drug prices could help the US reduce healthcare costs and improve health outcomes. Japan can learn from the US in areas such as medical innovation, technology adoption, and patient empowerment. Fostering a culture of innovation and promoting patient autonomy could enhance the quality of healthcare in Japan.
Supporting this, a comparative analysis by the World Health Organization (WHO) in May 2024 suggested that both countries could benefit from adopting best practices from each other. The US can learn from Japan’s success in providing affordable, accessible healthcare, while Japan can leverage the US’s strengths in research and development to drive medical advancements.
25. What Are Some Emerging Trends in Healthcare in Japan and the US?
Emerging trends in healthcare are shaping the future of healthcare in both Japan and the US. In the US, trends include the increasing use of telehealth, artificial intelligence (AI) in diagnostics and treatment, and personalized medicine. Japan is also embracing telehealth and AI, with a focus on addressing the needs of its aging population through remote monitoring and geriatric care technologies. Both countries are exploring innovative approaches to healthcare delivery and financing.
For instance, a report by McKinsey & Company in April 2024 highlighted that the global market for digital health technologies is growing rapidly, with significant investments in telehealth, AI, and wearable devices. Japan and the US are both positioned to benefit from these trends, though they must address challenges related to data privacy, regulatory frameworks, and equitable access to new technologies.
COMPARE.EDU.VN: Your Partner in Healthcare Comparisons
Navigating the complexities of healthcare systems can be daunting. At COMPARE.EDU.VN, we strive to make this process easier by providing detailed, objective comparisons. Whether you’re curious about “Japan compared to US” or any other healthcare systems, our platform offers the insights you need to make informed decisions. Explore our comprehensive analyses, compare key metrics, and gain a deeper understanding of healthcare options worldwide.
Ready to explore more healthcare comparisons? Visit COMPARE.EDU.VN today and discover the information you need to make informed decisions about your health and well-being.
Address: 333 Comparison Plaza, Choice City, CA 90210, United States
Whatsapp: +1 (626) 555-9090
Website: COMPARE.EDU.VN
FAQ: Japan Compared to US Healthcare Systems
1. Is healthcare free in Japan?
While not entirely free, Japan has a universal healthcare system where citizens pay a portion of their medical costs, with the government covering the rest. This ensures affordable access to healthcare for everyone.
2. Does the US have better medical technology than Japan?
The US is often at the forefront of medical innovation and technology. However, Japan is rapidly adopting advanced technologies to improve its healthcare system.
3. What are the biggest challenges in the US healthcare system?
High costs, lack of universal coverage, and disparities in access to care are among the biggest challenges in the US healthcare system.
4. What are the strengths of the Japanese healthcare system?
Universal coverage, lower costs, and a focus on preventative care are key strengths of the Japanese healthcare system.
5. How does life expectancy compare between Japan and the US?
Japan generally has a higher life expectancy than the US, partly due to its universal healthcare coverage and emphasis on preventative care.
6. What role does government regulation play in Japan’s healthcare system?
Government regulation plays a critical role in controlling healthcare costs in Japan, including regulating drug prices and setting fees for medical services.
7. How do patient satisfaction levels compare between Japan and the US?
Studies often show that patients in Japan report higher levels of satisfaction with their healthcare experiences compared to those in the US.
8. How do cultural attitudes towards healthcare differ between Japan and the US?
Japan emphasizes collectivism and social responsibility, supporting universal healthcare, while the US emphasizes individualism and personal responsibility, leading to differing views on government involvement in healthcare.
9. What can the US learn from Japan’s healthcare system?
The US can learn about the benefits of universal coverage, government regulation of healthcare costs, and a focus on preventative care.
10. What are some emerging trends in healthcare in Japan and the US?
Emerging trends include the increasing use of telehealth, artificial intelligence (AI) in diagnostics and treatment, and personalized medicine.
Are you looking for an objective comparison to aid decision-making? Visit compare.edu.vn now.