When Compared To Most Other Developed Countries The United States exhibits significantly higher healthcare spending; explore the reasons why on COMPARE.EDU.VN. This in-depth analysis provides clarity on the factors contributing to these elevated costs, while offering insights into alternative models and potential solutions, including healthcare expenditure, health economics, and comparative health systems.
1. Why Is Healthcare Spending Higher in the U.S. Compared to Other Developed Nations?
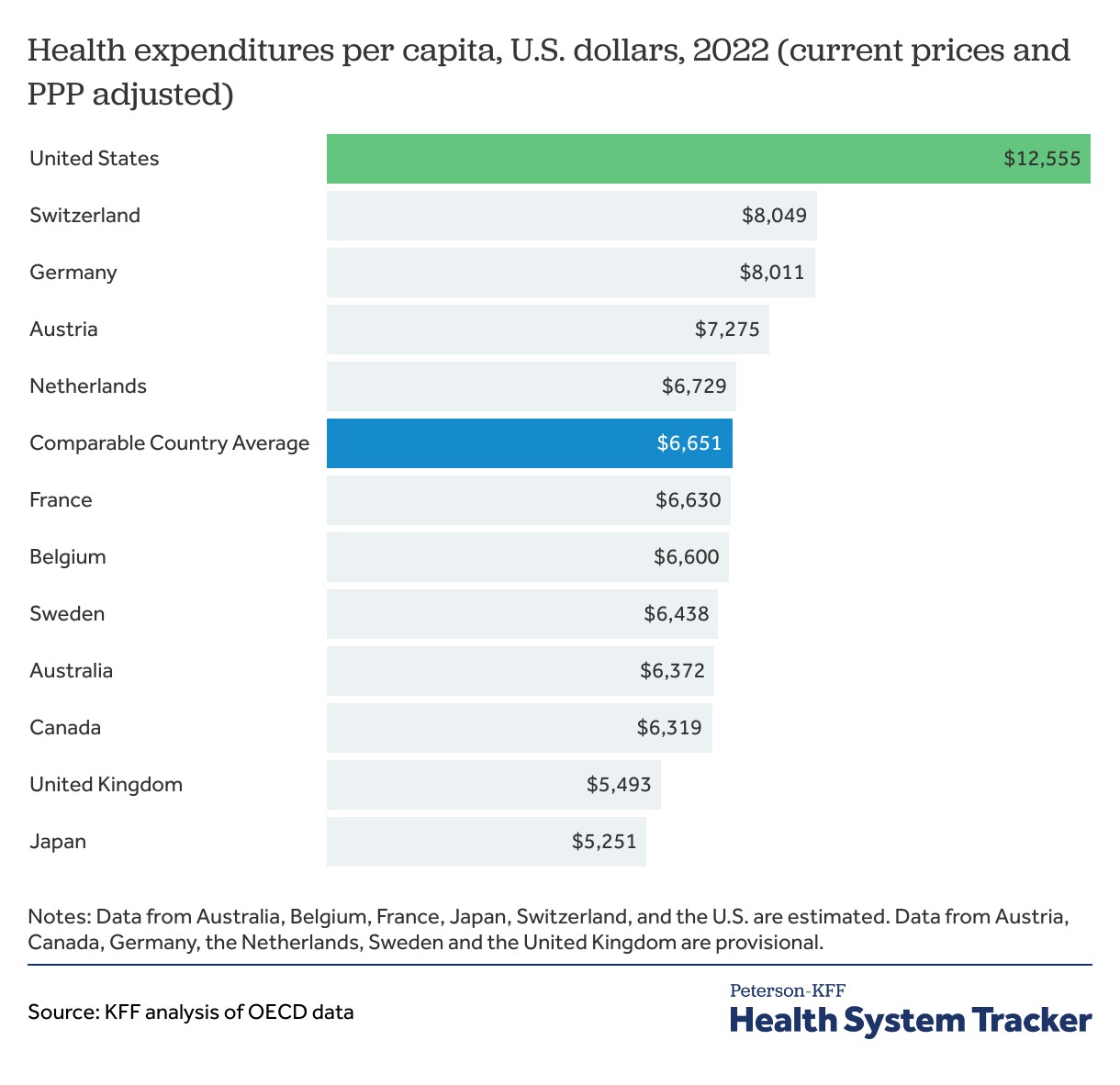
When compared to most other developed countries the United States consistently spends more on healthcare per capita. Several factors contribute to this disparity, including higher prices for medical services and pharmaceuticals, administrative costs, and a greater emphasis on specialized care.
1.1. Elevated Prices for Medical Services and Pharmaceuticals
The cost of healthcare services, including doctor visits, hospital stays, and procedures, is notably higher in the U.S. compared to other developed nations. Pharmaceutical prices are also significantly more expensive in the U.S. due to the absence of government price controls. According to a 2023 study by the RAND Corporation, prescription drug prices in the U.S. are, on average, 2.56 times higher than in 32 comparable countries.
1.2. High Administrative Overhead
The U.S. healthcare system involves multiple layers of administration, including private insurance companies, hospitals, and billing services. This complexity leads to substantial administrative overhead, consuming a significant portion of healthcare spending without directly contributing to patient care. A 2019 study published in Health Affairs estimated that administrative costs account for approximately 25% of total healthcare expenditures in the U.S., which is substantially higher than in countries with simpler, single-payer systems.
1.3. Emphasis on Specialized and Intensive Care
The U.S. healthcare system tends to prioritize specialized and intensive care over primary and preventive care. While advanced medical technologies and specialized treatments are readily available, this focus drives up costs. For example, the utilization of MRI and CT scans is higher in the U.S. compared to other developed countries, contributing to increased spending.
1.4. Lack of Universal Healthcare Coverage
Unlike many other developed countries that offer universal healthcare coverage, the U.S. relies on a mix of private and public insurance. A significant portion of the population remains uninsured or underinsured, leading to delayed care and increased reliance on emergency services, which are more expensive. The Affordable Care Act (ACA) has reduced the uninsured rate, but significant gaps remain.
2. How Does the U.S. Healthcare System Compare to Those of Other Developed Countries?
When compared to most other developed countries the U.S. healthcare system differs significantly in terms of structure, financing, and access. Examining these differences provides insight into why costs are higher and outcomes are often worse.
2.1. Structure and Financing Models
Most developed countries have adopted universal healthcare systems, typically funded through a combination of taxes and social insurance contributions. These systems ensure that all citizens have access to essential healthcare services, regardless of their income or employment status. Examples include:
- Single-Payer Systems: Canada and the United Kingdom operate under single-payer systems, where the government is the primary payer for healthcare services. This allows for greater control over costs and standardized access to care.
- Social Insurance Systems: Germany and France utilize social insurance systems, where healthcare is funded through mandatory contributions from employers and employees. These systems typically involve a mix of public and private providers, with government regulation to control costs and ensure quality.
In contrast, the U.S. relies on a multi-payer system, with a mix of private insurance companies, government programs like Medicare and Medicaid, and out-of-pocket payments. This fragmented system leads to inefficiencies, higher administrative costs, and disparities in access to care.
2.2. Access to Healthcare Services
Universal healthcare systems ensure that all citizens have access to necessary medical services. In countries like Canada and the UK, access is generally equitable, although there may be wait times for certain elective procedures. In the U.S., access to care is often dependent on insurance coverage and ability to pay, leading to disparities based on income, race, and geographic location.
2.3. Health Outcomes
Despite spending more on healthcare, the U.S. often lags behind other developed countries in key health outcomes. Life expectancy in the U.S. is lower than the OECD average, and infant mortality rates are higher. These outcomes are influenced by factors such as access to preventive care, prevalence of chronic diseases, and social determinants of health.
For instance, a 2022 report by The Commonwealth Fund compared health system performance across 11 high-income countries and found that the U.S. ranked last overall, despite having the highest healthcare spending.
3. What Are the Key Drivers of High Healthcare Costs in the U.S.?
When compared to most other developed countries the high healthcare costs in the U.S. can be attributed to several interconnected factors that create a unique and expensive healthcare landscape.
3.1. Market-Based Pricing and Lack of Regulation
In many developed countries, the government plays a significant role in regulating healthcare prices and negotiating with pharmaceutical companies. In the U.S., market-based pricing prevails, allowing hospitals, doctors, and pharmaceutical companies to set prices with limited government intervention. This lack of regulation contributes to inflated prices for services and drugs.
3.2. Fee-for-Service Payment Model
The predominant fee-for-service (FFS) payment model in the U.S. incentivizes providers to deliver more services, regardless of their necessity or effectiveness. This model contrasts with value-based care models, which reward providers for delivering high-quality, cost-effective care. The shift towards value-based care is slow but gaining momentum as healthcare organizations recognize the need to control costs and improve outcomes.
3.3. Technological Advancements and Innovation
While technological advancements and innovation have improved healthcare outcomes, they also contribute to increased costs. The adoption of new technologies often comes with high price tags, and the U.S. tends to adopt these technologies more rapidly than other countries. Balancing the benefits of innovation with cost containment is a major challenge for the U.S. healthcare system.
3.4. Social Determinants of Health
Social determinants of health, such as poverty, education, and access to healthy food and housing, significantly impact health outcomes and healthcare costs. The U.S. has higher rates of poverty and inequality compared to many other developed countries, which contributes to poorer health outcomes and increased healthcare spending. Addressing these social determinants is essential for improving health and reducing costs.
4. How Does Health Spending Growth in the U.S. Compare to Other Nations?
When compared to most other developed countries the U.S. has historically experienced faster growth in health spending, although recent trends show some convergence.
4.1. Historical Trends in Health Spending Growth
Over the past several decades, health spending in the U.S. has grown at a significantly faster rate than in other developed countries. This growth has been driven by factors such as rising prices, increased utilization of services, and technological advancements. However, in recent years, health spending growth in the U.S. has slowed somewhat, while other countries have seen increased spending.
4.2. Post-Pandemic Health Spending
The COVID-19 pandemic had a significant impact on health spending in the U.S. and other countries. In 2020, both the U.S. and peer countries increased health spending at a rapid rate to address the pandemic. However, in subsequent years, health spending growth in the U.S. returned to a more typical rate, while many peer countries continued to experience higher spending growth.
4.3. Factors Influencing Spending Growth
Several factors influence health spending growth, including economic conditions, demographic changes, and policy decisions. In recent years, increased spending on preventive care and outpatient services has contributed to higher spending growth in many developed countries. In the U.S., efforts to control costs through value-based care models and payment reforms may be moderating spending growth.
5. What Are the Potential Solutions to High Healthcare Costs in the U.S.?
When compared to most other developed countries addressing the high healthcare costs in the U.S. requires a multifaceted approach involving policy changes, payment reforms, and a greater focus on prevention and wellness.
5.1. Policy Reforms and Government Regulation
Implementing policy reforms, such as government regulation of healthcare prices and negotiation of pharmaceutical prices, could help to control costs. Other potential reforms include expanding access to affordable health insurance and strengthening consumer protections. Learning from the experiences of other developed countries with universal healthcare systems can inform policy decisions.
5.2. Payment Reforms and Value-Based Care
Transitioning from fee-for-service to value-based care models can incentivize providers to deliver high-quality, cost-effective care. Value-based care models reward providers for achieving specific outcomes and reducing unnecessary services. These models can be implemented through accountable care organizations (ACOs), bundled payments, and other innovative payment arrangements.
5.3. Emphasis on Prevention and Wellness
Investing in prevention and wellness programs can reduce the burden of chronic diseases and lower healthcare costs in the long term. Strategies include promoting healthy lifestyles, improving access to preventive care services, and addressing social determinants of health. Community-based interventions and public health campaigns can play a critical role in improving population health.
5.4. Technological Innovation and Efficiency
Leveraging technological innovation to improve efficiency and reduce costs is essential. Telemedicine, electronic health records, and data analytics can streamline healthcare delivery and improve patient outcomes. However, it is important to ensure that new technologies are implemented in a way that is cost-effective and equitable.
6. How Can Individuals Make Informed Decisions About Healthcare Spending?
When compared to most other developed countries it’s crucial for individuals in the U.S. to make informed decisions about their healthcare spending to maximize value and minimize financial burdens.
6.1. Understanding Health Insurance Options
Navigating the complexities of health insurance can be challenging, but it is essential for making informed decisions. Individuals should carefully evaluate their insurance options, considering factors such as premiums, deductibles, copays, and coverage limitations. Understanding the benefits and limitations of different types of insurance plans can help individuals choose the plan that best meets their needs and budget.
6.2. Shopping for Healthcare Services
Price transparency tools can help individuals compare prices for healthcare services and make informed decisions. Websites and apps that provide price information for common procedures and tests can empower consumers to shop around for the best value. However, it is important to consider factors beyond price, such as quality and convenience.
6.3. Utilizing Preventive Care Services
Taking advantage of preventive care services, such as annual check-ups and screenings, can help individuals detect and manage health problems early, reducing the need for expensive treatments later on. Preventive care services are often covered by insurance plans, and they can play a critical role in maintaining health and preventing chronic diseases.
6.4. Engaging in Shared Decision-Making
Engaging in shared decision-making with healthcare providers can help individuals make informed choices about their treatment options. Patients should ask questions, express their preferences, and work with their providers to develop a treatment plan that aligns with their goals and values. Shared decision-making can improve patient satisfaction and outcomes, while also reducing unnecessary costs.
7. What Role Does the Pharmaceutical Industry Play in U.S. Healthcare Costs?
When compared to most other developed countries the pharmaceutical industry’s role in U.S. healthcare costs is substantial, with drug prices significantly influencing overall spending.
7.1. High Drug Prices
The U.S. has some of the highest drug prices in the world, driven by factors such as patent protection, market exclusivity, and the absence of government price controls. Pharmaceutical companies argue that high prices are necessary to fund research and development of new drugs, but critics contend that they are excessive and unsustainable.
7.2. Impact of Drug Advertising
Direct-to-consumer advertising of prescription drugs is allowed in the U.S., which can drive up demand and increase healthcare costs. Pharmaceutical companies spend billions of dollars each year on advertising, which can influence patients to ask their doctors for specific medications, even if they are not the most appropriate or cost-effective option.
7.3. Generic and Biosimilar Drugs
Generic and biosimilar drugs offer lower-cost alternatives to brand-name medications, but their utilization can be limited by factors such as patent protection and marketing strategies. Promoting the use of generic and biosimilar drugs can help to reduce pharmaceutical spending and improve access to affordable medications.
7.4. Policy Options for Drug Pricing
Several policy options have been proposed to address high drug prices in the U.S., including government negotiation of drug prices, importation of drugs from other countries, and value-based pricing. These options have the potential to lower drug costs and improve affordability, but they also face political and economic challenges.
8. How Do Chronic Diseases Impact Healthcare Spending in the U.S.?
When compared to most other developed countries the prevalence of chronic diseases significantly contributes to high healthcare spending in the U.S.
8.1. Prevalence of Chronic Diseases
Chronic diseases, such as heart disease, diabetes, and cancer, are major drivers of healthcare spending in the U.S. These conditions often require ongoing medical care, medications, and lifestyle modifications, leading to substantial costs over time. The prevalence of chronic diseases is influenced by factors such as aging, obesity, and unhealthy lifestyles.
8.2. Cost of Managing Chronic Diseases
Managing chronic diseases accounts for a significant portion of healthcare expenditures in the U.S. Costs include doctor visits, hospital stays, medications, and rehabilitation services. Effective management of chronic diseases requires a coordinated approach involving healthcare providers, patients, and caregivers.
8.3. Prevention and Early Detection
Preventing chronic diseases and detecting them early can help to reduce healthcare costs and improve health outcomes. Strategies include promoting healthy lifestyles, improving access to preventive care services, and implementing screening programs for high-risk individuals. Early detection can lead to more effective treatment and better outcomes.
8.4. Integrated Care Models
Integrated care models, which coordinate care across different providers and settings, can improve the management of chronic diseases and reduce healthcare costs. These models involve multidisciplinary teams, shared decision-making, and a focus on patient-centered care. Integrated care can improve communication, reduce duplication of services, and enhance patient outcomes.
9. What is the Role of Technology in Reducing Healthcare Costs?
When compared to most other developed countries technology offers significant potential for reducing healthcare costs in the U.S. through increased efficiency, improved access, and better outcomes.
9.1. Telemedicine and Remote Monitoring
Telemedicine allows patients to receive medical care remotely, using video conferencing and other technologies. This can improve access to care for individuals in rural areas or those with limited mobility. Remote monitoring devices can track patients’ vital signs and other health data, allowing providers to intervene early if problems arise.
9.2. Electronic Health Records (EHRs)
Electronic health records (EHRs) can improve the efficiency and coordination of care by providing providers with access to comprehensive patient information. EHRs can also facilitate data analytics and quality improvement efforts. However, the implementation of EHRs can be costly and challenging, and it is important to ensure that they are used effectively.
9.3. Artificial Intelligence (AI) and Machine Learning
Artificial intelligence (AI) and machine learning have the potential to transform healthcare by improving diagnosis, treatment, and prevention. AI algorithms can analyze large amounts of data to identify patterns and predict outcomes, helping providers make more informed decisions. AI can also automate administrative tasks and improve efficiency.
9.4. Data Analytics and Personalized Medicine
Data analytics can be used to identify trends, track performance, and improve the quality and efficiency of care. Personalized medicine involves tailoring treatment to individual patients based on their genetic makeup, lifestyle, and other factors. These technologies can improve outcomes and reduce costs by ensuring that patients receive the right treatment at the right time.
10. How Can the U.S. Learn from Other Developed Countries to Reduce Healthcare Costs?
When compared to most other developed countries the U.S. can learn valuable lessons from countries with more efficient and affordable healthcare systems.
10.1. Universal Healthcare Coverage
Many developed countries have achieved universal healthcare coverage, ensuring that all citizens have access to necessary medical services. The U.S. can learn from these countries by expanding access to affordable health insurance and implementing policies to reduce the number of uninsured individuals.
10.2. Government Regulation and Price Controls
Government regulation of healthcare prices and negotiation of pharmaceutical prices can help to control costs. The U.S. can learn from countries that have successfully implemented these policies, such as Canada and the United Kingdom.
10.3. Emphasis on Primary and Preventive Care
Investing in primary and preventive care can reduce the burden of chronic diseases and lower healthcare costs in the long term. The U.S. can learn from countries that have strong primary care systems and emphasize prevention, such as the Netherlands and Switzerland.
10.4. Integrated and Coordinated Care
Integrated and coordinated care models can improve the management of chronic diseases and reduce healthcare costs. The U.S. can learn from countries that have successfully implemented these models, such as Germany and Sweden.
FAQ: Understanding U.S. Healthcare Costs Compared to Other Developed Nations
Q1: Why is U.S. healthcare so expensive?
A1: U.S. healthcare costs are high due to factors like high prices for medical services and drugs, administrative overhead, and a focus on specialized care.
Q2: How does the U.S. healthcare system compare to others?
A2: The U.S. has a multi-payer system, unlike the universal healthcare systems in many developed countries, leading to disparities in access and higher costs.
Q3: What are the main drivers of high healthcare costs in the U.S.?
A3: Key drivers include market-based pricing, fee-for-service models, technological advancements, and social determinants of health.
Q4: How is health spending growth in the U.S. compared to other nations?
A4: Historically, the U.S. had faster growth, but recent trends show some convergence, with other countries increasing spending on preventive care and outpatient services.
Q5: What solutions can lower healthcare costs in the U.S.?
A5: Potential solutions include policy reforms, value-based care, prevention, and leveraging technology.
Q6: How can individuals make informed healthcare decisions?
A6: By understanding insurance options, shopping for services, utilizing preventive care, and engaging in shared decision-making with providers.
Q7: What role does the pharmaceutical industry play in U.S. healthcare costs?
A7: High drug prices, advertising, and limited generic drug use contribute to high costs; policy options like government negotiation could help.
Q8: How do chronic diseases impact healthcare spending in the U.S.?
A8: Chronic diseases drive costs; prevention, early detection, and integrated care models can help manage these conditions.
Q9: What is the role of technology in reducing healthcare costs?
A9: Telemedicine, EHRs, AI, and data analytics can increase efficiency, improve access, and enhance outcomes.
Q10: How can the U.S. learn from other developed countries to reduce healthcare costs?
A10: By adopting universal coverage, government regulation, emphasis on primary care, and integrated care models.
Navigating the complexities of healthcare comparisons can be daunting. For detailed, unbiased comparisons and expert insights, visit COMPARE.EDU.VN. Make informed decisions with confidence.
Address: 333 Comparison Plaza, Choice City, CA 90210, United States
WhatsApp: +1 (626) 555-9090
Website: COMPARE.EDU.VN
Let compare.edu.vn be your guide to understanding and navigating the world of comparisons.