Are cigarette smokers and overweight individuals repeatedly compared? COMPARE.EDU.VN breaks down this complex issue, analyzing the reasons behind these comparisons and offering clarity. Delving into the science, psychology, and societal perceptions, we provide a comprehensive overview, helping you understand the underlying factors and make informed comparisons. Explore the parallels, the differences, and the implications for public health with our detailed analysis, focusing on lifestyle choices, well-being, and comparative health risks.
1. What Factors Lead to the Comparison of Smokers and Overweight People?
The comparison between cigarette smokers and overweight individuals arises from several shared characteristics and societal considerations. These include:
- Lifestyle Choices: Both smoking and overeating are often perceived as lifestyle choices that individuals make, leading to health consequences.
- Health Risks: Both behaviors are associated with significant health risks, including cardiovascular diseases, certain types of cancer, and reduced life expectancy.
- Public Health Concerns: Both smoking and obesity are major public health concerns, placing a burden on healthcare systems and reducing overall societal well-being.
- Addictive Behaviors: Both smoking and overeating can involve addictive behaviors, making it difficult for individuals to change these habits.
- Social Stigma: Both smokers and overweight people may face social stigma and discrimination due to their habits and appearance.
2. How Do Health Risks for Smokers Compare to Those for Overweight People?
Both smoking and being overweight carry substantial health risks, though the nature of these risks may differ. Smoking is a leading cause of lung cancer, respiratory diseases, and cardiovascular issues, while being overweight increases the risk of type 2 diabetes, heart disease, and certain cancers.
| Risk Factor | Cigarette Smoking | Overweight/Obesity |
|---|---|---|
| Cardiovascular | Heart disease, stroke, peripheral artery disease | Heart disease, stroke, hypertension |
| Cancer | Lung, throat, bladder, kidney, pancreatic, and others | Breast, colon, endometrial, kidney, esophageal, and others |
| Metabolic | Increased risk of type 2 diabetes | Type 2 diabetes, insulin resistance |
| Respiratory | Chronic obstructive pulmonary disease (COPD), bronchitis | Asthma, sleep apnea |
| Musculoskeletal | Reduced bone density | Osteoarthritis |
3. Are the Addictive Aspects of Smoking and Overeating Similar?
Both smoking and overeating can be addictive, but the mechanisms of addiction differ. Smoking addiction is primarily driven by nicotine, a highly addictive substance in cigarettes. Overeating, particularly of processed and sugary foods, can trigger reward pathways in the brain, leading to similar addictive behaviors.
- Smoking: Nicotine stimulates the release of dopamine in the brain, creating a pleasurable sensation that reinforces smoking behavior.
- Overeating: High-calorie, processed foods can also trigger dopamine release, leading to cravings and compulsive eating habits.
- Psychological Factors: Both smoking and overeating can be associated with psychological factors such as stress, anxiety, and depression, which can further reinforce these behaviors.
4. What Social Stigmas Do Smokers and Overweight People Face?
Both smokers and overweight people often face social stigma and discrimination, though the nature and extent of this stigma may vary. Smokers may be viewed negatively due to the health risks associated with smoking and the impact of secondhand smoke on others. Overweight people may face stigma related to appearance, perceived lack of self-control, and assumptions about their health and lifestyle.
- Smokers: Stigma may manifest as exclusion from social gatherings, negative attitudes from non-smokers, and restrictions on where smoking is allowed.
- Overweight People: Stigma may result in discrimination in employment, healthcare, and social interactions, as well as negative stereotypes about their character and abilities.
5. How Do Public Health Initiatives Address Smoking and Overweight/Obesity?
Public health initiatives targeting smoking and overweight/obesity often employ similar strategies, including education campaigns, policy changes, and community-based programs.
- Smoking: Public health efforts have focused on increasing awareness of the health risks of smoking, implementing smoke-free policies, raising taxes on tobacco products, and providing smoking cessation resources.
- Overweight/Obesity: Initiatives aimed at addressing overweight/obesity include promoting healthy eating habits and physical activity, implementing policies to reduce access to unhealthy foods, and providing resources for weight management.
6. What Psychological Factors Contribute to Smoking and Overeating?
Psychological factors play a significant role in both smoking and overeating. Stress, anxiety, depression, and other mental health issues can contribute to these behaviors as coping mechanisms or sources of comfort.
- Smoking: Nicotine can have mood-altering effects, providing temporary relief from stress and anxiety.
- Overeating: Food can serve as a source of emotional comfort, with individuals turning to food to cope with negative emotions or to reward themselves.
- Cognitive Factors: Beliefs, attitudes, and self-perception can also influence smoking and overeating behaviors.
7. How Can Individuals Overcome Smoking and Overeating Habits?
Overcoming smoking and overeating habits often requires a combination of strategies, including behavioral therapy, support groups, lifestyle changes, and, in some cases, medication.
- Smoking: Smoking cessation programs, nicotine replacement therapy, and prescription medications can help individuals quit smoking.
- Overeating: Behavioral therapy, such as cognitive-behavioral therapy (CBT) and dialectical behavior therapy (DBT), can help individuals identify and change unhealthy eating patterns.
- Lifestyle Changes: Making healthy lifestyle changes, such as adopting a balanced diet and engaging in regular physical activity, can support both smoking cessation and weight management.
8. What Are the Economic Impacts of Smoking and Overweight/Obesity?
Both smoking and overweight/obesity have significant economic impacts on individuals, healthcare systems, and society as a whole. These include healthcare costs, lost productivity, and premature mortality.
- Smoking: Healthcare costs associated with smoking-related illnesses are substantial, and smoking-related deaths result in significant losses in productivity.
- Overweight/Obesity: Obesity-related healthcare costs are also high, and obesity can lead to decreased productivity and increased disability rates.
- Societal Costs: Both smoking and obesity contribute to increased insurance premiums and other societal costs.
9. How Does Socioeconomic Status Relate to Smoking and Overweight/Obesity?
Socioeconomic status (SES) is strongly associated with both smoking and overweight/obesity. Individuals with lower SES are more likely to smoke and to be overweight or obese due to factors such as limited access to healthy foods, healthcare, and resources for smoking cessation and weight management.
- Smoking: Smoking rates are higher among individuals with lower levels of education and income.
- Overweight/Obesity: Obesity rates are also higher among low-income populations, particularly in areas with limited access to fresh produce and healthy food options.
- Environmental Factors: Individuals in low-SES communities may also face environmental factors that contribute to smoking and obesity, such as exposure to tobacco advertising and limited opportunities for physical activity.
10. What Role Does Genetics Play in Smoking and Overweight/Obesity?
Genetics can influence an individual’s susceptibility to both smoking and overweight/obesity, but genes are not the sole determinant. Genetic factors can affect nicotine dependence, appetite, metabolism, and body weight regulation.
- Smoking: Genes can influence how quickly nicotine is metabolized and how strongly an individual responds to nicotine’s rewarding effects.
- Overweight/Obesity: Genetic factors can affect metabolic rate, fat storage, and appetite regulation, making some individuals more prone to weight gain.
- Gene-Environment Interaction: Genes interact with environmental factors, such as diet and lifestyle, to determine an individual’s risk of smoking and obesity.
11. How Do Cultural Norms Influence Smoking and Overeating Behaviors?
Cultural norms can significantly influence smoking and overeating behaviors. In some cultures, smoking may be viewed as socially acceptable or even glamorous, while in others, it is stigmatized. Similarly, cultural norms can influence food preferences, portion sizes, and attitudes towards body weight.
- Smoking: Cultural norms regarding smoking can affect initiation rates, cessation rates, and exposure to secondhand smoke.
- Overeating: Cultural norms regarding food can influence dietary patterns, portion sizes, and attitudes towards body weight.
- Globalization: Globalization can lead to the spread of unhealthy dietary patterns and lifestyles, contributing to increased rates of obesity and related health problems.
12. What Prevention Strategies Are Effective in Reducing Smoking and Overweight/Obesity?
Effective prevention strategies for reducing smoking and overweight/obesity include a combination of individual-level interventions, community-based programs, and policy changes.
- Smoking: Prevention strategies include education campaigns targeting youth, smoke-free policies in public places, taxation of tobacco products, and restrictions on tobacco advertising.
- Overweight/Obesity: Prevention strategies include promoting healthy eating habits and physical activity in schools and communities, implementing policies to reduce access to unhealthy foods, and creating environments that support active living.
- Multi-Sectoral Approach: Effective prevention requires a multi-sectoral approach involving collaboration among healthcare providers, educators, policymakers, community organizations, and the food industry.
13. How Do Advertising and Marketing Influence Smoking and Overeating?
Advertising and marketing play a significant role in influencing smoking and overeating behaviors. Tobacco advertising has been shown to increase smoking rates, particularly among youth, while marketing of unhealthy foods can contribute to overeating and weight gain.
- Smoking: Tobacco advertising often targets young people and uses imagery that associates smoking with attractiveness, independence, and rebellion.
- Overeating: Marketing of unhealthy foods often uses persuasive techniques to encourage overconsumption, such as large portion sizes, appealing packaging, and celebrity endorsements.
- Regulation: Restrictions on tobacco advertising have been shown to reduce smoking rates, and similar regulations could be applied to the marketing of unhealthy foods.
14. What Are the Ethical Considerations in Comparing Smokers and Overweight People?
Comparing smokers and overweight people raises ethical considerations related to stigma, discrimination, and personal responsibility. It is important to avoid perpetuating negative stereotypes and to recognize that both smoking and overweight/obesity are complex issues influenced by a variety of factors.
- Stigma: Comparisons should be made in a way that does not increase stigma or discrimination against smokers or overweight people.
- Personal Responsibility: While individuals have a responsibility for their health, it is important to recognize that choices are influenced by environmental, social, and economic factors.
- Compassion: Comparisons should be made with compassion and understanding, recognizing that both smoking and overweight/obesity can be difficult to overcome.
15. How Do Health Professionals Approach Smoking and Weight Management with Patients?
Health professionals should approach smoking and weight management with patients in a supportive and non-judgmental manner, providing evidence-based interventions and personalized advice.
- Smoking: Health professionals should routinely ask patients about their smoking status and provide brief advice on quitting. They should also offer referrals to smoking cessation programs and prescribe medications when appropriate.
- Weight Management: Health professionals should assess patients’ weight and body mass index (BMI) and provide advice on healthy eating and physical activity. They should also offer referrals to weight management programs and consider prescribing medications or bariatric surgery for eligible patients.
- Integrated Approach: An integrated approach that addresses both smoking and weight management can be particularly effective, as these behaviors are often interrelated.
16. What Are the Latest Research Findings on Smoking and Weight?
Recent research has shed light on the complex relationship between smoking and weight, including the effects of smoking cessation on weight gain and the impact of weight loss interventions on smoking behavior.
- Smoking Cessation: Studies have shown that smoking cessation is often associated with weight gain, but this weight gain is typically modest and does not negate the health benefits of quitting smoking.
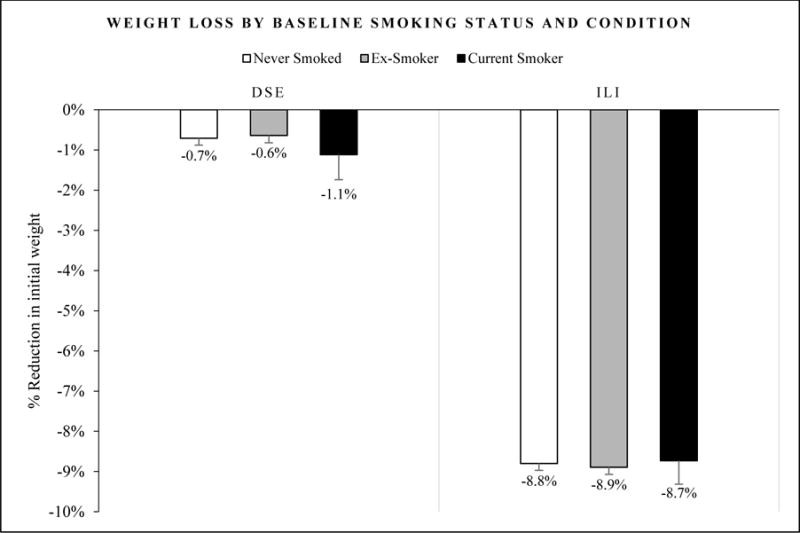
- Weight Loss Interventions: Research has found that weight loss interventions can be effective for smokers, and that these interventions do not necessarily lead to increased smoking.
- Behavioral Interventions: Behavioral interventions that address both smoking and weight management have shown promising results in improving health outcomes.
17. How Can Policymakers Address Smoking and Overweight/Obesity at the Population Level?
Policymakers can play a key role in addressing smoking and overweight/obesity at the population level by implementing evidence-based policies that promote healthy lifestyles and reduce exposure to risk factors.
- Smoking: Policies include taxation of tobacco products, smoke-free policies in public places, restrictions on tobacco advertising, and funding for smoking cessation programs.
- Overweight/Obesity: Policies include taxation of sugary drinks, restrictions on marketing of unhealthy foods to children, subsidies for healthy foods, and creation of environments that support active living.
- Health Equity: Policies should be designed to address health inequities and ensure that all populations have access to healthy food, safe environments, and resources for smoking cessation and weight management.
18. What Are the Long-Term Health Consequences of Smoking and Overweight/Obesity?
The long-term health consequences of smoking and overweight/obesity are significant and can include chronic diseases, disability, reduced quality of life, and premature mortality.
- Smoking: Long-term smoking can lead to lung cancer, heart disease, COPD, and other chronic diseases.
- Overweight/Obesity: Long-term overweight/obesity can lead to type 2 diabetes, heart disease, certain cancers, and other health problems.
- Cumulative Effects: The cumulative effects of smoking and overweight/obesity can be particularly devastating, leading to a shortened lifespan and increased risk of multiple chronic diseases.
19. How Do Different Countries Approach Smoking and Overweight/Obesity?
Different countries have adopted various approaches to addressing smoking and overweight/obesity, with varying degrees of success. Some countries have implemented comprehensive policies that have led to significant reductions in smoking rates and obesity prevalence, while others have lagged behind.
- Smoking: Countries like Australia and the United Kingdom have implemented comprehensive tobacco control policies that have led to significant reductions in smoking rates.
- Overweight/Obesity: Countries like Finland and South Korea have implemented policies to promote healthy eating and physical activity, resulting in lower rates of obesity compared to other developed nations.
- Lessons Learned: Lessons learned from successful countries can inform policy efforts in other nations.
20. How Can Individuals Advocate for Policies That Support Healthier Lifestyles?
Individuals can play an active role in advocating for policies that support healthier lifestyles by engaging in grassroots activism, contacting elected officials, and supporting organizations that promote public health.
- Grassroots Activism: Individuals can organize community events, start petitions, and raise awareness about the need for policies that support healthier lifestyles.
- Contacting Elected Officials: Individuals can contact their elected officials to express their support for policies that address smoking and overweight/obesity.
- Supporting Organizations: Individuals can support organizations that advocate for public health policies and provide resources for smoking cessation and weight management.
 Comparing risks of smoking and obesity
Comparing risks of smoking and obesity
21. Are There Any Benefits to Comparing Smoking and Overweight People?
Comparing smokers and overweight people can be beneficial in certain contexts, such as when identifying shared risk factors, developing prevention strategies, and advocating for policy changes. However, it is important to avoid perpetuating negative stereotypes and to recognize that these are complex issues with multiple contributing factors.
- Shared Risk Factors: Both smoking and overweight/obesity share risk factors such as socioeconomic status, psychological factors, and cultural norms.
- Prevention Strategies: Prevention strategies that address these shared risk factors can be effective in reducing both smoking and overweight/obesity.
- Policy Changes: Advocating for policy changes that support healthier lifestyles can benefit both smokers and overweight people.
22. How Can Media Coverage Influence Perceptions of Smoking and Overweight People?
Media coverage can significantly influence public perceptions of smoking and overweight people. Responsible media reporting can increase awareness of the health risks associated with these behaviors and promote understanding and compassion. However, sensationalized or stigmatizing coverage can perpetuate negative stereotypes and discrimination.
- Responsible Reporting: Responsible media reporting should focus on the facts, avoid sensationalism, and present a balanced view of the issues.
- Avoiding Stigma: Media coverage should avoid perpetuating negative stereotypes and discrimination against smokers and overweight people.
- Promoting Awareness: Media coverage can play a key role in promoting awareness of the health risks associated with smoking and overweight/obesity and in encouraging individuals to adopt healthier lifestyles.
23. What Role Do Schools Play in Preventing Smoking and Overweight/Obesity?
Schools play a critical role in preventing smoking and overweight/obesity by providing education, promoting healthy behaviors, and creating supportive environments.
- Education: Schools can provide age-appropriate education about the health risks of smoking and the benefits of healthy eating and physical activity.
- Healthy Behaviors: Schools can promote healthy behaviors by offering nutritious meals and snacks, providing opportunities for physical activity, and implementing smoke-free policies.
- Supportive Environments: Schools can create supportive environments by promoting positive body image, addressing bullying and stigma, and providing resources for students who are struggling with smoking or weight management.
24. How Do Workplace Wellness Programs Address Smoking and Overweight/Obesity?
Workplace wellness programs can be effective in addressing smoking and overweight/obesity by providing employees with resources, incentives, and support for adopting healthier lifestyles.
- Resources: Workplace wellness programs can offer smoking cessation resources, weight management programs, and health coaching services.
- Incentives: Employers can provide incentives for employees who participate in wellness programs and achieve health goals.
- Support: Workplace wellness programs can create a supportive environment by promoting healthy behaviors, addressing stigma, and providing opportunities for employees to connect with each other.
25. What Are the Key Takeaways from Comparing Smokers and Overweight People?
The key takeaways from comparing smokers and overweight people include the recognition that these are complex issues influenced by a variety of factors, that both behaviors carry significant health risks, and that effective prevention and treatment require a multi-faceted approach.
- Complexity: Both smoking and overweight/obesity are complex issues influenced by genetic, environmental, social, and psychological factors.
- Health Risks: Both behaviors carry significant health risks, including chronic diseases, disability, and premature mortality.
- Multi-Faceted Approach: Effective prevention and treatment require a multi-faceted approach that addresses individual behaviors, environmental factors, and policy changes.
26. How Can Technology Be Used to Address Smoking and Overweight/Obesity?
Technology can play an important role in addressing smoking and overweight/obesity by providing individuals with access to information, support, and tools for behavior change.
- Mobile Apps: Mobile apps can provide individuals with personalized advice, track their progress, and offer support and encouragement.
- Wearable Devices: Wearable devices can track physical activity, sleep patterns, and other health metrics, providing individuals with valuable feedback.
- Telehealth: Telehealth can provide individuals with remote access to healthcare providers, making it easier to receive counseling, support, and medical care.
27. What Are the Future Directions for Research on Smoking and Weight?
Future research on smoking and weight should focus on identifying effective prevention and treatment strategies, understanding the complex interactions between smoking and weight, and addressing health inequities related to these behaviors.
- Prevention Strategies: Research is needed to identify effective prevention strategies that can reduce smoking rates and obesity prevalence, particularly among vulnerable populations.
- Complex Interactions: More research is needed to understand the complex interactions between smoking and weight, including the effects of smoking cessation on weight gain and the impact of weight loss interventions on smoking behavior.
- Health Inequities: Research is needed to address health inequities related to smoking and overweight/obesity and to develop interventions that are tailored to the needs of diverse populations.
28. How Do Support Groups Aid in Quitting Smoking and Losing Weight?
Support groups offer a valuable resource for individuals trying to quit smoking or lose weight. These groups provide a sense of community, shared experiences, and mutual encouragement.
- Community: Support groups create a sense of community where individuals can connect with others who are facing similar challenges.
- Shared Experiences: Members can share their experiences, strategies, and successes, providing valuable insights and support.
- Encouragement: The group dynamic fosters encouragement and motivation, helping individuals stay committed to their goals.
29. What Specific Diet Plans Are Recommended for Overweight Smokers?
For overweight smokers aiming to improve their health, a balanced diet rich in nutrients is crucial. Specific diet plans often recommended include the Mediterranean diet, the DASH diet, and portion-controlled eating.
- Mediterranean Diet: Emphasizes fruits, vegetables, whole grains, lean proteins, and healthy fats, reducing the risk of heart disease and promoting overall wellness.
- DASH Diet: Designed to lower blood pressure, this diet is low in sodium, saturated fat, and cholesterol, focusing on fruits, vegetables, and low-fat dairy.
- Portion-Controlled Eating: Helps manage calorie intake by controlling portion sizes, which can lead to weight loss and better health outcomes.
30. How Does Physical Activity Assist in Smoking Cessation and Weight Management?
Physical activity is a powerful tool for both smoking cessation and weight management. It helps reduce cravings, manage weight, and improve overall health.
- Reduce Cravings: Exercise can help reduce nicotine cravings and withdrawal symptoms, making it easier to quit smoking.
- Weight Management: Physical activity burns calories and helps maintain a healthy weight, reducing the risk of obesity-related diseases.
- Improved Health: Regular exercise improves cardiovascular health, boosts mood, and enhances overall well-being, supporting both smoking cessation and weight management efforts.
31. What Medications Are Available to Help with Smoking and Weight Loss?
Several medications are available to assist with smoking cessation and weight loss. These medications should be used under the guidance of a healthcare professional.
- Smoking Cessation: Nicotine replacement therapy (NRT), bupropion, and varenicline are commonly prescribed to help reduce cravings and withdrawal symptoms.
- Weight Loss: Orlistat, phentermine-topiramate, and liraglutide are available for weight loss, often prescribed for individuals with obesity or related health conditions.
- Healthcare Guidance: It’s essential to consult with a healthcare provider to determine the most appropriate medication and dosage based on individual health needs.
32. How Do Mental Health Conditions Affect Smoking and Weight?
Mental health conditions like depression, anxiety, and stress can significantly influence smoking and weight. Addressing these conditions is crucial for successful behavior change.
- Depression and Anxiety: Individuals with depression and anxiety may turn to smoking or overeating as coping mechanisms.
- Stress: Chronic stress can lead to increased smoking and unhealthy eating habits.
- Integrated Treatment: An integrated approach that addresses both mental health and unhealthy behaviors can lead to more sustainable outcomes.
33. What Are the Benefits of Quitting Smoking on Weight?
While some people fear weight gain after quitting smoking, the long-term benefits of quitting far outweigh any potential weight gain.
- Improved Cardiovascular Health: Quitting smoking dramatically reduces the risk of heart disease, stroke, and other cardiovascular conditions.
- Reduced Cancer Risk: Smoking cessation lowers the risk of various cancers, including lung, throat, and bladder cancer.
- Better Respiratory Health: Quitting smoking improves lung function and reduces the risk of COPD and other respiratory diseases.
34. How Can Family and Friends Support Someone Trying to Quit Smoking or Lose Weight?
Support from family and friends can make a significant difference in helping someone quit smoking or lose weight.
- Encouragement: Offer positive encouragement and praise for efforts and achievements.
- Understanding: Be understanding and patient during difficult times, recognizing the challenges involved in behavior change.
- Active Participation: Participate in healthy activities together, such as going for walks or preparing healthy meals.
35. What Are Some Common Myths About Smoking and Weight?
Several myths surround smoking and weight, which can hinder effective interventions. It’s important to dispel these myths with accurate information.
- Myth: Smoking Helps You Stay Thin: While nicotine can suppress appetite, the health risks of smoking far outweigh any potential weight control benefits.
- Myth: You’ll Inevitably Gain Weight If You Quit Smoking: While some weight gain is common, it’s manageable with a healthy diet and regular exercise.
- Myth: It’s Too Late to Quit Smoking if You’re Overweight: Quitting smoking at any age provides significant health benefits, regardless of weight.
36. How Can Mindfulness Techniques Aid in Managing Cravings and Emotional Eating?
Mindfulness techniques can be powerful tools for managing cravings and emotional eating, helping individuals become more aware of their thoughts and feelings.
- Awareness: Mindfulness helps individuals become more aware of their cravings and emotional triggers.
- Non-Judgment: It encourages a non-judgmental approach to cravings, allowing individuals to observe them without acting on them impulsively.
- Coping Strategies: Mindfulness provides strategies for managing cravings and emotional eating, such as deep breathing and mindful eating.
37. What Are the Differences in How Men and Women Experience Smoking and Weight Issues?
Men and women may experience smoking and weight issues differently due to biological, social, and cultural factors.
- Biological Factors: Hormonal differences can affect metabolism, appetite, and nicotine dependence.
- Social Factors: Social norms and expectations can influence smoking and eating habits differently for men and women.
- Cultural Factors: Cultural ideals of beauty and body image can impact how men and women perceive and manage their weight.
38. How Can Healthcare Providers Tailor Interventions to Individual Needs?
Tailoring interventions to individual needs is essential for successful smoking cessation and weight management.
- Assess Individual Needs: Conduct a thorough assessment of individual health history, lifestyle, and preferences.
- Set Realistic Goals: Help individuals set realistic and achievable goals based on their unique circumstances.
- Provide Personalized Advice: Offer personalized advice and support tailored to individual needs and preferences.
39. What Are the Long-Term Health Benefits of Maintaining a Healthy Weight and Not Smoking?
Maintaining a healthy weight and not smoking offers significant long-term health benefits, including increased longevity and improved quality of life.
- Increased Longevity: Individuals who maintain a healthy weight and do not smoke tend to live longer.
- Improved Quality of Life: They also experience a higher quality of life, with fewer chronic diseases and disabilities.
- Reduced Healthcare Costs: Maintaining a healthy lifestyle can reduce healthcare costs over the long term.
40. How Does the Media Portray the Challenges of Quitting Smoking and Losing Weight?
The media’s portrayal of the challenges of quitting smoking and losing weight can significantly influence public perception and motivation.
- Realistic Representation: Realistic portrayals can help people understand the challenges involved and prepare for them.
- Inspirational Stories: Sharing success stories can inspire others and provide hope.
- Avoidance of Stereotypes: Avoiding stigmatizing stereotypes can create a more supportive environment for behavior change.
For detailed comparisons and expert advice to help you make informed decisions, visit COMPARE.EDU.VN, your trusted source for comprehensive comparisons.
Address: 333 Comparison Plaza, Choice City, CA 90210, United States
Whatsapp: +1 (626) 555-9090
Website: compare.edu.vn
FAQ: Comparing Cigarette Smokers and Overweight People
-
Why are cigarette smokers and overweight people often compared?
They are compared due to shared lifestyle choices, health risks, public health concerns, addictive behaviors, and social stigma. -
What are the main health risks for smokers versus overweight people?
Smokers face risks like lung cancer and heart disease, while overweight individuals risk type 2 diabetes and heart disease. -
Are the addictive aspects of smoking and overeating similar?
Yes, both can be addictive by triggering reward pathways in the brain, but smoking is primarily driven by nicotine. -
What social stigmas do smokers and overweight people face?
Smokers face exclusion and negative attitudes, while overweight people may face discrimination in employment and social interactions. -
How do public health initiatives address smoking and obesity?
Both use education campaigns, policy changes, and community programs to promote healthier lifestyles. -
What psychological factors contribute to smoking and overeating?
Stress, anxiety, and depression can lead to these behaviors as coping mechanisms. -
How can individuals overcome smoking and overeating habits?
Strategies include behavioral therapy, support groups, lifestyle changes, and medication. -
What are the economic impacts of smoking and obesity?
Both have high healthcare costs, lost productivity, and premature mortality. -
How does socioeconomic status relate to smoking and obesity?
Lower socioeconomic status is linked to higher rates of both due to limited access to resources. -
What role does genetics play in smoking and obesity?
Genetics can influence susceptibility, but lifestyle and environmental factors are also significant.
