The US healthcare system faces significant challenges when compared with other developed nations, as highlighted on COMPARE.EDU.VN, particularly in areas like access, cost, and overall health outcomes. By exploring aspects such as mortality rates, healthcare access, and preventative services, we can gain a comprehensive understanding of where the US stands globally and what improvements can be made. Discover a comprehensive and unbiased comparison of healthcare models, exploring global healthcare systems, national healthcare, and comparative healthcare systems.
1. Understanding the US Healthcare System
The United States healthcare system is a complex mix of private and public insurance coverage. Private insurance is primarily employer-sponsored, while public insurance includes programs like Medicare for the elderly and Medicaid for low-income individuals and families.
1.1. Key Features of the US Healthcare System
- Private Insurance Dominance: A large portion of the population relies on private health insurance plans, often obtained through employers.
- Government Programs: Medicare and Medicaid provide coverage for specific populations, but eligibility criteria and benefits vary by state.
- Fee-for-Service Model: Many healthcare providers operate under a fee-for-service model, where they are paid for each individual service they provide.
- High Administrative Costs: The US system is known for its high administrative overhead, including billing, insurance processing, and regulatory compliance.
1.2. Challenges Within the US System
- High Costs: Healthcare costs in the US are significantly higher than in other developed countries, leading to financial burdens for individuals and families.
- Access Issues: Many Americans face barriers to accessing healthcare, including lack of insurance, high deductibles, and limited availability of services in certain areas.
- Inequities: Disparities in healthcare access and outcomes exist based on income, race, ethnicity, and geographic location.
- Complexity: The fragmented nature of the system can be confusing for patients and providers, leading to inefficiencies and errors.
2. Healthcare Systems in Other Developed Countries
To understand how the US healthcare system compares, it’s essential to examine models used in other developed countries. These systems often prioritize universal coverage and affordability.
2.1. Universal Healthcare Models
- Canada: Canada operates under a single-payer system, where the government funds healthcare services through taxes. Citizens have access to medically necessary services without direct out-of-pocket costs.
- United Kingdom: The UK’s National Health Service (NHS) provides comprehensive healthcare services to all residents, funded through general taxation. Patients pay minimal costs at the point of service.
- Australia: Australia has a mixed public-private system, with Medicare providing universal coverage for basic healthcare services. Private insurance is also available for additional coverage.
2.2. Social Insurance Models
- Germany: Germany uses a social insurance model, where individuals are required to have health insurance, either through public or private plans. Employers and employees contribute to the cost of insurance.
- Netherlands: The Netherlands has a similar social insurance system, with mandatory health insurance for all residents. Insurers compete for enrollees, and the government regulates the market to ensure affordability and access.
- Switzerland: Switzerland also operates under a social insurance model, with mandatory health insurance and government subsidies to help lower-income individuals afford coverage.
3. Comparing Key Metrics: US vs. Other Countries
Several key metrics can be used to compare the performance of the US healthcare system to those of other developed countries. These include healthcare spending, access to care, quality of care, and health outcomes.
3.1. Healthcare Spending
The US spends significantly more on healthcare per capita than any other developed country. Despite this high level of spending, the US does not consistently achieve better health outcomes.
- US Spending: The US spends over $12,000 per person annually on healthcare, according to the Centers for Medicare & Medicaid Services (CMS).
- Comparable Countries: Countries like Canada, the UK, and Germany spend between $5,000 and $7,000 per person annually.
- Reasons for High Costs: Factors contributing to high US costs include higher prices for drugs and medical services, greater administrative overhead, and a higher prevalence of chronic diseases.
3.2. Access to Care
Access to healthcare in the US is a major concern, with millions of Americans lacking health insurance coverage.
- Uninsured Rate: According to the Kaiser Family Foundation, approximately 8% of Americans are uninsured.
- Comparable Countries: Most developed countries have near-universal health coverage, with less than 1% of the population uninsured.
- Barriers to Access: Even insured Americans may face barriers to accessing care, such as high deductibles, co-pays, and limited provider networks.
3.3. Quality of Care
The quality of healthcare in the US varies widely, with some areas excelling in certain aspects and lagging in others.
- Preventative Care: The US generally performs well in providing preventative services like vaccinations and cancer screenings.
- Chronic Disease Management: Management of chronic diseases like diabetes and heart disease is often less effective in the US compared to other countries.
- Patient Safety: The US has made progress in improving patient safety, but still lags behind some countries in reducing medical errors and hospital-acquired infections.
3.4. Health Outcomes
Health outcomes in the US are generally worse than in other developed countries, despite higher healthcare spending.
- Life Expectancy: Life expectancy in the US is lower than in many comparable countries, according to data from the World Bank.
- Infant Mortality: The US has a higher infant mortality rate than most developed countries.
- Mortality Rates: The US has higher mortality rates for certain conditions, such as heart disease, stroke, and diabetes.
4. Specific Comparisons: Mortality Rates
Mortality rates provide a clear picture of how well a healthcare system is performing in terms of saving lives and improving overall health.
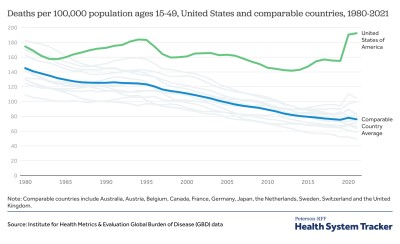
4.1. All-Cause Mortality
All-cause mortality rates reflect the overall health of a population and the effectiveness of the healthcare system in preventing deaths from various causes.
- US Mortality: The US has a higher all-cause mortality rate compared to many other developed countries, according to the OECD.
- Comparable Countries: Countries like Japan, Switzerland, and Australia have significantly lower all-cause mortality rates.
- Factors Contributing to Mortality: Factors contributing to higher US mortality rates include higher rates of chronic diseases, obesity, and violence.
4.2. Infant Mortality
Infant mortality rates are a critical indicator of a country’s healthcare system and overall societal well-being.
- US Infant Mortality: The US has a higher infant mortality rate compared to many other developed countries.
- Comparable Countries: Countries like Finland, Japan, and Sweden have significantly lower infant mortality rates.
- Reasons for High Infant Mortality: Factors contributing to higher US infant mortality rates include disparities in access to prenatal care, high rates of preterm births, and inadequate postnatal care.
4.3. Maternal Mortality
Maternal mortality rates reflect the quality of healthcare services provided to women during pregnancy, childbirth, and the postpartum period.
- US Maternal Mortality: The US has one of the highest maternal mortality rates among developed countries, and the rate has been increasing in recent years, according to the CDC.
- Comparable Countries: Countries like Norway, New Zealand, and the Netherlands have significantly lower maternal mortality rates.
- Factors Contributing to Maternal Mortality: Factors contributing to higher US maternal mortality rates include disparities in access to prenatal and postpartum care, high rates of chronic diseases among pregnant women, and inadequate coordination of care.
4.4. Disease-Specific Mortality
Mortality rates for specific diseases can provide insights into the effectiveness of a healthcare system in managing and treating those conditions.
- Heart Disease: The US has a higher mortality rate from heart disease compared to many other developed countries.
- Cancer: While cancer survival rates in the US are relatively high, mortality rates for certain types of cancer are still higher than in some other countries.
- Diabetes: The US has a higher mortality rate from diabetes compared to many other developed countries.
5. Healthcare Access: Insurance Coverage and Affordability
Access to healthcare is a critical factor in determining health outcomes. Insurance coverage and affordability are key components of access.
5.1. Health Insurance Coverage
Health insurance coverage is essential for ensuring that individuals can access needed healthcare services without facing financial barriers.
- US Coverage: The US has a mix of public and private health insurance coverage, but millions of Americans remain uninsured.
- Comparable Countries: Most developed countries have near-universal health coverage through single-payer or social insurance systems.
- Impact of Uninsurance: Lack of health insurance can lead to delayed or forgone care, resulting in poorer health outcomes and higher healthcare costs in the long run.
5.2. Affordability of Care
Even with insurance coverage, healthcare can be unaffordable for many Americans due to high deductibles, co-pays, and out-of-pocket costs.
- High Deductibles: Many Americans have high-deductible health plans, requiring them to pay thousands of dollars out-of-pocket before their insurance coverage kicks in.
- Co-pays and Coinsurance: Co-pays and coinsurance can also add to the cost of care, making it difficult for individuals to afford needed services.
- Medical Debt: Medical debt is a significant problem in the US, with millions of Americans struggling to pay their medical bills.
5.3. Impact of Cost on Access
High healthcare costs can deter individuals from seeking care, even when they have insurance coverage.
- Delayed Care: Many Americans delay or forgo needed healthcare services due to cost concerns.
- Missed Appointments: Patients may miss appointments with their healthcare providers due to cost concerns.
- Prescription Drug Costs: High prescription drug costs can make it difficult for individuals to afford needed medications, leading to poorer health outcomes.
6. Preventative Services: A Key to Better Health
Preventative services, such as vaccinations and screenings, are essential for maintaining health and preventing disease.
6.1. Vaccination Rates
Vaccination rates are an important indicator of a healthcare system’s ability to prevent infectious diseases.
- US Vaccination Rates: Vaccination rates in the US are generally high, but there are disparities based on income, race, ethnicity, and geographic location.
- Comparable Countries: Many developed countries have higher vaccination rates than the US.
- Impact of Vaccinations: Vaccinations are a cost-effective way to prevent infectious diseases and improve public health.
6.2. Cancer Screenings
Cancer screenings, such as mammograms and colonoscopies, are essential for detecting cancer early, when it is most treatable.
- US Screening Rates: Screening rates for certain types of cancer in the US are lower than in some other developed countries.
- Comparable Countries: Countries like the UK and Australia have higher screening rates for certain types of cancer.
- Impact of Screenings: Early detection of cancer through screenings can improve survival rates and reduce the need for more aggressive treatments.
6.3. Preventative Care for Chronic Diseases
Preventative care for chronic diseases, such as diabetes and heart disease, can help individuals manage their conditions and prevent complications.
- US Preventative Care: Preventative care for chronic diseases in the US is often less effective than in other developed countries.
- Comparable Countries: Countries like Canada and the Netherlands have more comprehensive preventative care programs for chronic diseases.
- Impact of Preventative Care: Effective preventative care can improve health outcomes, reduce healthcare costs, and enhance quality of life for individuals with chronic diseases.
7. Long-Term Health Outcomes: A Broader Perspective
Long-term health outcomes reflect the overall effectiveness of a healthcare system in promoting health and preventing disease over the long term.
7.1. Life Expectancy at Birth
Life expectancy at birth is a commonly used indicator of overall health and well-being in a population.
- US Life Expectancy: The US has a lower life expectancy compared to many other developed countries. According to the CDC, the life expectancy in the US is around 77 years.
- Comparable Countries: Countries like Japan, Switzerland, and Australia have higher life expectancies, often exceeding 80 years.
- Factors Influencing Life Expectancy: Factors influencing life expectancy include healthcare access, lifestyle factors, environmental conditions, and socioeconomic factors.
7.2. Healthy Life Years
Healthy life years measure the number of years an individual is expected to live in good health, free from disability or disease.
- US Healthy Life Years: The US has a lower number of healthy life years compared to many other developed countries.
- Comparable Countries: Countries like Sweden and Switzerland have higher numbers of healthy life years.
- Factors Influencing Healthy Life Years: Factors influencing healthy life years include healthcare access, lifestyle factors, and the prevalence of chronic diseases.
7.3. Quality of Life
Quality of life measures the overall well-being and satisfaction of individuals with their lives, including their physical, mental, and social health.
- US Quality of Life: The US generally scores lower on quality of life measures compared to many other developed countries.
- Comparable Countries: Countries like Denmark and Norway consistently score high on quality of life measures.
- Factors Influencing Quality of Life: Factors influencing quality of life include healthcare access, economic conditions, social support, and environmental quality.
8. System Efficiency: Administrative Costs and Waste
The efficiency of a healthcare system refers to how well it uses resources to achieve desired health outcomes. Administrative costs and waste are significant factors affecting efficiency.
8.1. Administrative Costs
Administrative costs in the US healthcare system are significantly higher than in other developed countries.
- US Administrative Costs: A large portion of healthcare spending in the US goes towards administrative costs, including billing, insurance processing, and regulatory compliance.
- Comparable Countries: Countries with single-payer or social insurance systems have lower administrative costs due to streamlined processes and reduced paperwork.
- Impact of High Administrative Costs: High administrative costs divert resources away from direct patient care and contribute to higher overall healthcare spending.
8.2. Wasteful Spending
Wasteful spending in the US healthcare system includes unnecessary tests, procedures, and treatments, as well as fraud and abuse.
- Unnecessary Care: Many studies have found that a significant portion of healthcare services in the US are unnecessary or inappropriate.
- Fraud and Abuse: Fraud and abuse in the healthcare system contribute to wasteful spending and divert resources away from legitimate healthcare services.
- Impact of Wasteful Spending: Wasteful spending reduces the efficiency of the healthcare system and contributes to higher overall healthcare costs.
8.3. Potential Savings
Reducing administrative costs and wasteful spending could generate significant savings that could be used to improve healthcare access and quality.
- Streamlining Processes: Streamlining administrative processes and reducing paperwork could lower administrative costs.
- Reducing Unnecessary Care: Implementing evidence-based guidelines and promoting shared decision-making could reduce unnecessary care.
- Combating Fraud and Abuse: Strengthening oversight and enforcement could combat fraud and abuse in the healthcare system.
9. The Role of Technology: Innovation and Adoption
Technology plays a crucial role in modern healthcare systems, driving innovation and improving patient care.
9.1. Adoption of Electronic Health Records (EHRs)
Electronic Health Records (EHRs) are digital versions of patients’ paper charts, providing a comprehensive view of their medical history.
- US EHR Adoption: The US has made significant progress in adopting EHRs in recent years, driven by government incentives and mandates.
- Comparable Countries: Many developed countries have also adopted EHRs, but the level of adoption and integration varies.
- Benefits of EHRs: EHRs can improve care coordination, reduce medical errors, and enhance patient engagement.
9.2. Telehealth and Remote Monitoring
Telehealth and remote monitoring technologies allow healthcare providers to deliver care remotely, improving access and convenience for patients.
- US Telehealth Adoption: Telehealth adoption in the US has increased rapidly in recent years, driven by the COVID-19 pandemic and changes in reimbursement policies.
- Comparable Countries: Many developed countries have also embraced telehealth, but the extent of adoption varies.
- Benefits of Telehealth: Telehealth can improve access to care for patients in rural areas, reduce healthcare costs, and enhance patient satisfaction.
9.3. Artificial Intelligence (AI) and Machine Learning (ML)
Artificial Intelligence (AI) and Machine Learning (ML) technologies are being used to improve diagnosis, treatment, and prevention of diseases.
- AI/ML Applications: AI and ML are being used in areas such as image analysis, drug discovery, and personalized medicine.
- Potential Benefits: AI and ML have the potential to improve healthcare outcomes, reduce costs, and enhance efficiency.
- Challenges: Challenges to AI and ML adoption in healthcare include data privacy concerns, regulatory issues, and the need for skilled professionals.
10. Policy Implications: Reforming the US Healthcare System
Reforming the US healthcare system to improve access, affordability, and quality is a complex and ongoing process. Various policy options have been proposed and debated.
10.1. Single-Payer Healthcare
Single-payer healthcare involves replacing the current mix of public and private insurance with a single government-run insurance program.
- Arguments for Single-Payer: Proponents argue that single-payer healthcare would simplify the system, reduce administrative costs, and ensure universal coverage.
- Arguments Against Single-Payer: Opponents argue that single-payer healthcare would lead to government overreach, reduced choice, and potential rationing of care.
- Examples: Canada and the UK have single-payer healthcare systems.
10.2. Public Option
A public option would involve creating a government-run health insurance plan that would compete with private insurance plans.
- Arguments for Public Option: Proponents argue that a public option would increase competition, lower premiums, and expand coverage.
- Arguments Against Public Option: Opponents argue that a public option would unfairly compete with private insurers and could lead to the collapse of the private insurance market.
10.3. Strengthening the Affordable Care Act (ACA)
The Affordable Care Act (ACA) has expanded health insurance coverage in the US, but millions of Americans remain uninsured. Strengthening the ACA could involve expanding subsidies, increasing outreach efforts, and addressing gaps in coverage.
- Arguments for Strengthening the ACA: Proponents argue that strengthening the ACA would further expand coverage and improve access to care.
- Arguments Against Strengthening the ACA: Opponents argue that the ACA is too costly and ineffective and that alternative approaches should be pursued.
10.4. Value-Based Care
Value-based care focuses on paying healthcare providers based on the quality of care they provide, rather than the quantity of services they deliver.
- Arguments for Value-Based Care: Proponents argue that value-based care would incentivize providers to deliver high-quality, cost-effective care.
- Arguments Against Value-Based Care: Opponents argue that value-based care is complex to implement and may not be effective in all settings.
FAQ: Comparing US Healthcare with Other Countries
Q1: Why is healthcare so expensive in the US compared to other countries?
Healthcare costs in the US are higher due to factors such as higher prices for drugs and medical services, greater administrative overhead, and a higher prevalence of chronic diseases.
Q2: How does the US healthcare system compare in terms of access to care?
The US has a lower rate of health insurance coverage compared to many developed countries, leading to barriers in accessing necessary healthcare services.
Q3: What are some of the main differences between the US healthcare system and those in Canada or the UK?
Canada and the UK have universal healthcare systems, where the government funds healthcare services through taxes, ensuring that all citizens have access to medically necessary services without direct out-of-pocket costs. The US, on the other hand, relies on a mix of private and public insurance.
Q4: How does the quality of care in the US compare to other countries?
The quality of healthcare in the US varies, with strengths in preventative services but weaknesses in managing chronic diseases compared to other developed nations.
Q5: What are some of the policy options for reforming the US healthcare system?
Policy options include single-payer healthcare, a public option, strengthening the Affordable Care Act (ACA), and promoting value-based care.
Q6: How does the US perform in terms of long-term health outcomes like life expectancy?
The US has a lower life expectancy compared to many other developed countries, reflecting broader issues in healthcare access and overall population health.
Q7: What role does technology play in improving healthcare in the US?
Technology, including EHRs, telehealth, and AI, is playing an increasing role in improving care coordination, reducing medical errors, and enhancing patient engagement in the US.
Q8: What are the challenges associated with implementing a single-payer healthcare system in the US?
Challenges include political opposition, concerns about government overreach, potential reductions in choice, and logistical complexities in transitioning from the current system.
Q9: How can value-based care improve the efficiency of the US healthcare system?
Value-based care incentivizes providers to deliver high-quality, cost-effective care, reducing unnecessary services and improving patient outcomes, thereby enhancing efficiency.
Q10: What can individuals do to navigate the complexities of the US healthcare system?
Individuals can research insurance options, understand their coverage, seek preventative care, and advocate for their healthcare needs to navigate the complexities of the US system effectively.
Conclusion: The Path Forward for US Healthcare
The US healthcare system faces significant challenges in comparison to other developed countries. High costs, access issues, and poorer health outcomes highlight the need for reform. By learning from other countries and implementing evidence-based policies, the US can move towards a more equitable, affordable, and effective healthcare system.
Ready to explore more detailed comparisons and make informed decisions? Visit COMPARE.EDU.VN today! Our comprehensive platform provides unbiased information and detailed analyses to help you understand and navigate the complexities of various systems. Make the smart choice with COMPARE.EDU.VN!
COMPARE.EDU.VN – Making Comparisons Simple
Address: 333 Comparison Plaza, Choice City, CA 90210, United States
WhatsApp: +1 (626) 555-9090
Website: compare.edu.vn