Nonspecific resistance and specific immunity are two critical arms of the immune system, each playing a distinct role in protecting the body from pathogens; COMPARE.EDU.VN offers comprehensive comparisons to help you understand their differences and how they work together. Understanding how these defense mechanisms differ and complement each other is essential for grasping the overall immune response, as well as related ideas like immune system components, immune response types, and adaptive immunity.
1. Understanding the Body’s Defense Mechanisms
The human body possesses a remarkable defense system, a complex network of cells, tissues, and organs working in harmony to protect against harmful invaders. This system, known as the immune system, employs multiple lines of defense, each with its unique strategies and capabilities. These defenses can be broadly categorized into two main types: nonspecific resistance (also known as innate immunity) and specific immunity (also known as adaptive immunity). This article will delve into a comparison of these two crucial aspects of immunity.
1.1. The Three Lines of Defense
The immune system operates through three distinct lines of defense:
- Physical and Chemical Barriers: These form the first line of defense, preventing pathogens from entering the body. Examples include the skin, mucous membranes, and secretions like tears and saliva.
- Nonspecific Resistance (Innate Immunity): This is the body’s immediate, generalized response to any threat. It involves cells like macrophages and neutrophils, as well as processes like inflammation and fever.
- Specific Immunity (Adaptive Immunity): This is a targeted response that develops over time, directed against specific pathogens. It involves lymphocytes (T cells and B cells) and the production of antibodies.
1.2. The Importance of a Functional Immune System
A compromised immune system can leave the body vulnerable to a multitude of infections and diseases. Understanding the intricate workings of the immune system, including the roles of nonspecific resistance and specific immunity, is crucial for maintaining health and well-being. This includes recognizing the importance of key factors such as immune cells, immune response, and immunological memory.
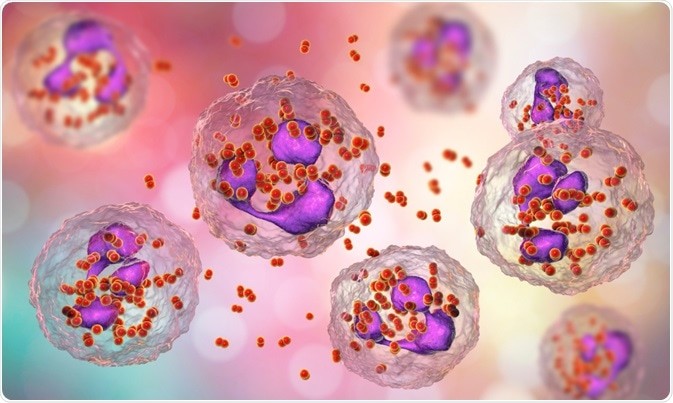
Leukocytes, crucial players in both nonspecific resistance and specific immunity, actively attacking a virus to neutralize the threat.
2. What is Nonspecific Resistance (Innate Immunity)?
Nonspecific resistance, also known as innate immunity, is the body’s immediate and generalized defense against pathogens. It is the first responder, providing a rapid response to any foreign invader, regardless of its identity.
2.1. Key Features of Nonspecific Resistance
- Rapid Response: Innate immunity is activated within minutes or hours of encountering a pathogen.
- Generalized Response: It responds to a wide range of pathogens without prior exposure.
- No Memory: It does not develop immunological memory, meaning the response remains the same upon repeated exposure to the same pathogen.
2.2. Components of Nonspecific Resistance
Nonspecific resistance involves various components, including:
-
Physical Barriers: These prevent pathogens from entering the body in the first place. Examples include the skin, mucous membranes, and secretions like tears and saliva.
-
Chemical Barriers: These include substances like stomach acid, which kills ingested pathogens, and lysozyme, an enzyme found in tears and saliva that breaks down bacterial cell walls.
-
Cellular Defenses: These involve various immune cells that attack and destroy pathogens. Examples include:
- Macrophages: These are phagocytic cells that engulf and digest pathogens, as well as cellular debris.
- Neutrophils: These are the most abundant type of white blood cell and are also phagocytic.
- Natural Killer (NK) Cells: These cells kill infected or cancerous cells by releasing cytotoxic granules.
-
Inflammation: This is a localized response to injury or infection, characterized by redness, swelling, heat, and pain. Inflammation helps to contain the infection, recruit immune cells to the site, and promote tissue repair.
-
Fever: This is an elevation of body temperature, which can inhibit the growth of pathogens and enhance the activity of immune cells.
-
Complement System: This is a group of proteins in the blood that can be activated by pathogens or antibodies. Activation of the complement system leads to a cascade of events that result in pathogen destruction and inflammation.
2.3. The Role of Natural Killer (NK) Cells
Natural killer cells are a type of cytotoxic lymphocyte critical to the innate immune system. They provide rapid responses to virally infected cells and tumor formation, acting at around 3 days after infection. NK cells are unique because they can recognize and kill infected cells without prior sensitization.
Phagocytosis is a crucial process in nonspecific resistance, where immune cells like macrophages engulf and digest pathogens to clear the body of infection.
3. What is Specific Immunity (Adaptive Immunity)?
Specific immunity, also known as adaptive immunity, is a targeted defense against specific pathogens. It develops over time and involves lymphocytes (T cells and B cells) and the production of antibodies.
3.1. Key Features of Specific Immunity
- Slow Response: Adaptive immunity takes several days or weeks to develop.
- Targeted Response: It responds to specific pathogens that the body has encountered before.
- Memory: It develops immunological memory, meaning the response is faster and stronger upon repeated exposure to the same pathogen.
3.2. Components of Specific Immunity
Specific immunity involves two main types of lymphocytes:
-
T Cells: These cells are involved in cell-mediated immunity, which involves the direct killing of infected cells. There are several types of T cells, including:
- Helper T Cells (CD4+ T Cells): These cells help activate other immune cells, including B cells and cytotoxic T cells.
- Cytotoxic T Cells (CD8+ T Cells): These cells kill infected or cancerous cells.
- Regulatory T Cells: These cells help suppress the immune response and prevent autoimmunity.
-
B Cells: These cells are involved in antibody-mediated immunity (humoral immunity), which involves the production of antibodies that target specific pathogens. When a B cell encounters its specific antigen, it differentiates into a plasma cell, which produces large amounts of antibodies.
3.3. How Specific Immunity Works
- Antigen Recognition: The adaptive immune system recognizes antigens, which are molecules found on the surface of pathogens.
- Lymphocyte Activation: When a lymphocyte (T cell or B cell) encounters its specific antigen, it becomes activated.
- Clonal Expansion: Activated lymphocytes undergo clonal expansion, meaning they proliferate rapidly to create a large population of cells that can respond to the antigen.
- Effector Functions: Activated lymphocytes perform effector functions, such as killing infected cells (cytotoxic T cells) or producing antibodies (plasma cells).
- Memory Formation: Some activated lymphocytes differentiate into memory cells, which remain in the body for a long time and provide long-lasting immunity.
3.4. The Role of Antibodies
Antibodies, also known as immunoglobulins, are proteins produced by B cells that bind to specific antigens. Antibodies can neutralize pathogens, mark them for destruction by phagocytes, or activate the complement system. There are five main types of antibodies:
- IgG: The most abundant type of antibody in the blood, providing long-term immunity.
- IgM: The first antibody produced during an infection.
- IgA: Found in mucous membranes, providing protection against pathogens entering the body.
- IgE: Involved in allergic reactions and parasitic infections.
- IgD: Found on the surface of B cells, involved in B cell activation.
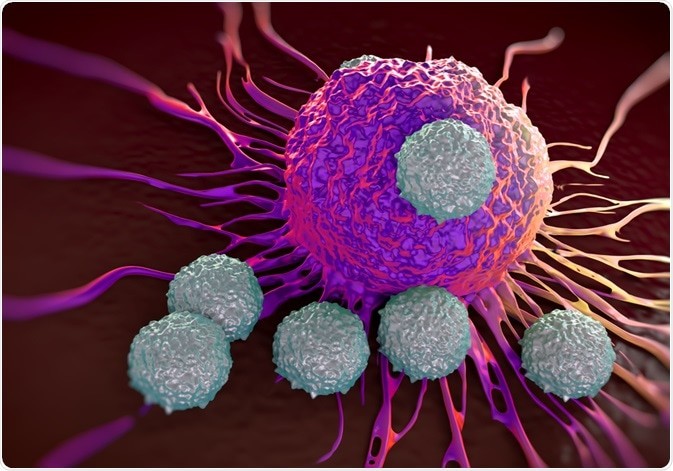
T lymphocytes, essential components of specific immunity, targeting and attacking a cancer cell to prevent its spread and protect the body.
4. How Do Nonspecific Resistance and Specific Immunity Compare?
While both nonspecific resistance and specific immunity are crucial for protecting the body against pathogens, they differ in several key aspects.
4.1. Key Differences Between Nonspecific Resistance and Specific Immunity
| Feature | Nonspecific Resistance (Innate Immunity) | Specific Immunity (Adaptive Immunity) |
|---|---|---|
| Response Time | Rapid (minutes to hours) | Slow (days to weeks) |
| Specificity | Generalized (responds to a wide range of pathogens) | Targeted (responds to specific pathogens) |
| Memory | No memory | Memory (long-lasting immunity) |
| Main Components | Physical barriers, chemical barriers, phagocytes, NK cells, inflammation, fever, complement system | T cells, B cells, antibodies |

4.2. Complementary Roles
Nonspecific resistance and specific immunity work together to provide comprehensive protection against pathogens. Innate immunity provides the initial defense, while adaptive immunity develops a targeted and long-lasting response.
For example, macrophages, which are part of the innate immune system, can present antigens to T cells, which are part of the adaptive immune system. This interaction helps to activate the adaptive immune response.
Similarly, antibodies produced by B cells, which are part of the adaptive immune system, can enhance the activity of phagocytes, which are part of the innate immune system. This interaction helps to clear pathogens from the body more effectively.
5. The Interplay Between Innate and Adaptive Immunity
The innate and adaptive immune systems don’t operate in isolation; they engage in constant communication and collaboration. This interplay is essential for mounting effective immune responses against a wide range of threats.
5.1. Antigen Presentation
Antigen presentation is a critical process that bridges the gap between innate and adaptive immunity. Phagocytic cells, such as macrophages and dendritic cells, engulf pathogens and break them down into smaller fragments called antigens. These antigens are then presented on the surface of the phagocytic cells, where they can be recognized by T cells.
5.2. Cytokine Signaling
Cytokines are signaling molecules that play a crucial role in communication between immune cells. Innate immune cells, such as macrophages and NK cells, produce cytokines that activate and direct the adaptive immune response. Adaptive immune cells, such as T cells, also produce cytokines that modulate the activity of innate immune cells.
5.3. Costimulatory Molecules
In addition to antigen presentation, T cell activation requires costimulatory signals. These signals are provided by costimulatory molecules expressed on the surface of antigen-presenting cells. The interaction between costimulatory molecules on antigen-presenting cells and costimulatory receptors on T cells is essential for T cell activation and the development of an effective adaptive immune response.
6. Factors Affecting Immune Function
Several factors can influence the function of the immune system, including:
6.1. Age
Immune function declines with age, making older adults more susceptible to infections.
6.2. Nutrition
Malnutrition can impair immune function, increasing the risk of infection. A balanced diet rich in vitamins, minerals, and antioxidants is essential for maintaining a healthy immune system.
6.3. Stress
Chronic stress can suppress immune function, making individuals more vulnerable to illness. Stress management techniques, such as exercise, meditation, and yoga, can help to improve immune function.
6.4. Sleep
Lack of sleep can impair immune function, increasing the risk of infection. Aim for 7-8 hours of sleep per night to maintain a healthy immune system.
6.5. Underlying Medical Conditions
Certain medical conditions, such as HIV/AIDS, cancer, and autoimmune diseases, can weaken the immune system.
6.6. Medications
Some medications, such as corticosteroids and immunosuppressants, can suppress immune function.
7. Strategies to Boost Immune Function
There are several strategies that can help to boost immune function:
7.1. Healthy Diet
Eat a balanced diet rich in fruits, vegetables, whole grains, and lean protein.
7.2. Regular Exercise
Engage in regular physical activity to improve immune function and reduce stress.
7.3. Adequate Sleep
Aim for 7-8 hours of sleep per night to support immune function.
7.4. Stress Management
Practice stress management techniques, such as meditation, yoga, or spending time in nature.
7.5. Vaccination
Get vaccinated against preventable diseases to protect yourself from infection.
7.6. Avoid Smoking and Excessive Alcohol Consumption
Smoking and excessive alcohol consumption can weaken the immune system.
8. The Future of Immunotherapy
Immunotherapy, which harnesses the power of the immune system to fight disease, is a rapidly evolving field with immense potential.
8.1. Cancer Immunotherapy
Cancer immunotherapy aims to stimulate the immune system to recognize and destroy cancer cells. This approach has shown remarkable success in treating certain types of cancer.
8.2. Autoimmune Disease Immunotherapy
Immunotherapy is also being explored as a treatment for autoimmune diseases, which occur when the immune system mistakenly attacks the body’s own tissues.
8.3. Infectious Disease Immunotherapy
Immunotherapy can be used to enhance the immune response to infectious diseases, particularly in individuals with weakened immune systems.
9. Real-World Examples of Immune System Function
Understanding how the immune system functions in real-world scenarios can provide valuable insights into its importance and complexity.
9.1. The Common Cold
When you catch a cold, your immune system kicks into gear to fight off the virus. Innate immune defenses, such as the production of mucus and inflammation, help to contain the infection. Adaptive immune defenses, such as the production of antibodies, help to clear the virus from your body and provide long-lasting immunity.
9.2. Flu Season
During flu season, many people get vaccinated against the influenza virus. Vaccination stimulates the adaptive immune system to produce antibodies that protect against the flu.
9.3. Wound Healing
When you get a cut, your immune system plays a crucial role in wound healing. Innate immune defenses, such as inflammation and phagocytosis, help to clear debris and prevent infection. Adaptive immune defenses, such as the production of growth factors, help to promote tissue repair.
10. Immune System Disorders
Dysregulation of the immune system can lead to various disorders, including:
10.1. Autoimmune Diseases
In autoimmune diseases, the immune system mistakenly attacks the body’s own tissues. Examples include rheumatoid arthritis, lupus, and type 1 diabetes.
10.2. Immunodeficiency Disorders
In immunodeficiency disorders, the immune system is weakened, making individuals more susceptible to infections. Examples include HIV/AIDS and severe combined immunodeficiency (SCID).
10.3. Allergic Reactions
Allergic reactions occur when the immune system overreacts to harmless substances, such as pollen or food.
11. Conclusion: A Balanced Immune Response
In summary, both nonspecific resistance and specific immunity are essential components of the immune system. Nonspecific resistance provides an immediate, generalized defense against pathogens, while specific immunity develops a targeted, long-lasting response. These two systems work together to provide comprehensive protection against a wide range of threats. Understanding the interplay between innate and adaptive immunity is crucial for maintaining health and well-being. Factors like lifestyle, nutrition, and stress management play a significant role in modulating immune function. As research continues to advance, immunotherapy holds tremendous promise for treating a variety of diseases, from cancer to autoimmune disorders. By appreciating the complexities of the immune system, we can better protect ourselves from illness and promote overall health. Explore more detailed comparisons and resources at COMPARE.EDU.VN.
12. Frequently Asked Questions (FAQ)
1. What is the main difference between innate and adaptive immunity?
Innate immunity is rapid and generalized, while adaptive immunity is slow and specific.
2. What are the key components of innate immunity?
Physical barriers, chemical barriers, phagocytes, NK cells, inflammation, fever, and the complement system.
3. What are the key components of adaptive immunity?
T cells, B cells, and antibodies.
4. How does the immune system recognize pathogens?
Innate immunity recognizes general patterns on pathogens, while adaptive immunity recognizes specific antigens.
5. What is the role of antibodies in immunity?
Antibodies bind to pathogens, neutralizing them or marking them for destruction.
6. How does vaccination work?
Vaccination stimulates the adaptive immune system to produce antibodies against a specific pathogen.
7. What factors can affect immune function?
Age, nutrition, stress, sleep, underlying medical conditions, and medications.
8. How can I boost my immune function?
Eat a healthy diet, exercise regularly, get adequate sleep, manage stress, and get vaccinated.
9. What is immunotherapy?
Immunotherapy is a treatment that harnesses the power of the immune system to fight disease.
10. What are some examples of immune system disorders?
Autoimmune diseases, immunodeficiency disorders, and allergic reactions.
Take Action for Your Health
Ready to take control of your health and make informed decisions? Visit COMPARE.EDU.VN today to explore detailed comparisons, expert reviews, and personalized recommendations. Whether you’re looking to understand different treatment options, compare healthcare providers, or find the best health products, we’re here to help you navigate your healthcare journey with confidence.
Address: 333 Comparison Plaza, Choice City, CA 90210, United States
WhatsApp: +1 (626) 555-9090
Website: compare.edu.vn
Disclaimer: This article is intended for informational purposes only and does not constitute medical advice. Consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.